A Comprehensive Overview of Discectomy for Patients and Healthcare Professionals
Introduction
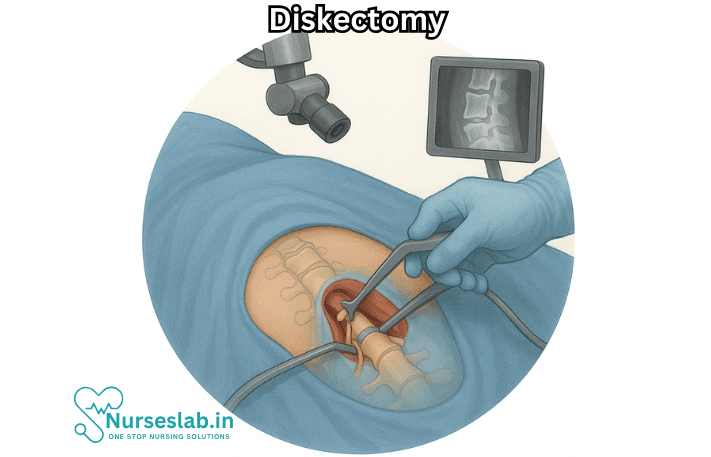
Diskectomy is a surgical procedure performed to remove all or part of a herniated or damaged intervertebral disc in the spine. This operation is commonly recommended to relieve pressure on spinal nerves or the spinal cord when conservative treatments fail. As spinal conditions become increasingly prevalent due to aging populations and sedentary lifestyles, understanding the purpose, process, and outcomes of discectomy is crucial for both patients and healthcare providers.
What is a Diskectomy?
A discectomy, sometimes spelled “diskectomy,” is derived from the words “disc”—referring to the cushion-like structures between the vertebrae—and “ectomy,” meaning removal. The most common indication for this surgery is a herniated disc, where the soft inner material (nucleus pulposus) protrudes through the outer layer (annulus fibrosus), compressing nerves and causing pain, weakness, or numbness in the back, legs, or arms.
Anatomy of the Spine and Intervertebral Discs
The human spine is composed of 33 vertebrae separated by intervertebral discs. These discs function as shock absorbers, allowing flexibility and movement while maintaining the structural integrity of the spine. Each disc contains a gelatinous center and a tough surrounding ring. When a disc herniates, inflammation and nerve irritation may result, leading to significant neurological symptoms.
Indications for Diskectomy
Not all disc herniations require surgical intervention. The decision to perform a discectomy is based on several criteria, including the severity of symptoms and the response to non-surgical treatments. Common indications include:
- Severe or persistent leg or arm pain due to nerve compression (radiculopathy)
- Loss of strength, sensation, or reflexes in the limbs
- Impaired bladder or bowel function (cauda equina syndrome, a surgical emergency)
- Failure of conservative therapies such as physical therapy, medications, and spinal injections
Conservative Treatments Prior to Diskectomy
Before considering surgery, most patients undergo a period of non-surgical management, which may include:
- Physical therapy and exercise programs
- Nonsteroidal anti-inflammatory drugs (NSAIDs) or other pain medications
- Epidural steroid injections
- Activity modification and rest
Only when these measures are insufficient does surgical intervention become the next step.
Types of Diskectomy Procedures
Several surgical techniques can be used to perform a discectomy, each with unique advantages and limitations.
Open Diskectomy
This traditional approach involves a small incision in the back, allowing the surgeon direct access to the affected disc. Muscles and tissues are retracted to visualize the spinal column, and the herniated portion of the disc is carefully removed.
Microdiskectomy
A microdiscectomy is a minimally invasive variant, utilizing an operating microscope and small instruments to access the spine through a much smaller incision. This technique reduces tissue trauma, postoperative pain, and recovery time compared to open surgery.
Endoscopic Diskectomy
Endoscopic discectomy employs specialized instruments and a tiny camera inserted through a thin tube. This procedure is less invasive, often allowing for same-day discharge and expedited return to normal activities.
The Diskectomy Procedure: Step-by-Step
While the exact steps vary depending on the technique, the general process includes:
- Anesthesia: Discectomy is usually performed under general anesthesia, though local anesthesia with sedation may be used for some minimally invasive approaches.
- Incision and Exposure: The surgeon makes an incision over the affected area, moves muscles aside, and visualizes the spinal column and nerve roots.
- Removal of the Disc Material: Using surgical instruments and, in some cases, a microscope or endoscope, the herniated or damaged disc material that is compressing the nerve is carefully removed.
- Closure: The incision is closed with sutures or staples, and a sterile dressing is applied.
Risks and Complications
Like all surgeries, diskectomy carries certain risks, though serious complications are uncommon. Possible risks include:
- Infection at the surgical site
- Bleeding or hematoma formation
- Nerve injury or persistent pain
- Recurrence of disc herniation
- Spinal fluid leak (dural tear)
- Blood clots (deep vein thrombosis)
Preoperative planning and adherence to sterile technique reduce these risks significantly.
Recovery and Rehabilitation
Many patients experience rapid improvement in symptoms following discectomy. The recovery process depends on the extent of surgery, preoperative health, and adherence to postoperative care instructions.
Immediate Postoperative Period
Patients are often encouraged to walk within hours of surgery. Pain is managed with medications, and most can return home the same day or within 24-48 hours. Detailed discharge instructions focus on wound care, activity restrictions, and signs of complications.
Long-Term Recovery
Gradual return to daily activities is recommended, with avoidance of heavy lifting or strenuous exercise for several weeks. Physical therapy may be prescribed to enhance flexibility, strength, and spinal health. Most individuals can return to work—especially in sedentary jobs—within 2-6 weeks, though full recovery for more physically demanding occupations may take longer.
Outcomes and Prognosis
Discectomy is associated with high rates of patient satisfaction and symptom relief. Success rates range from 80% to 90% for improvement of nerve pain and associated symptoms. Factors influencing outcomes include:
- Severity and duration of preoperative symptoms
- Presence of neurological deficits
- Overall health and lifestyle factors
- Adherence to rehabilitation protocols
Recurrence and Prevention
A small percentage of patients may experience a recurrence of disc herniation at the same or different spinal level. Preventive strategies include maintaining a healthy weight, practicing good posture, engaging in regular exercise, and using proper body mechanics when lifting objects.
Special Considerations
Discectomy in Older Adults
Older adults may have additional health challenges, such as osteoporosis or degenerative disc disease, that can complicate surgical decision-making and recovery. A multidisciplinary approach involving surgeons, primary care providers, and physical therapists is often warranted.
Pediatric Diskectomy
Though rare, discectomy may be performed in children or adolescents with severe disc herniation and neurological compromise. The principles of care are similar, but special attention is paid to growth and development.
Emerging Technologies
Advancements in medical imaging, surgical instrumentation, and robotics continue to refine discectomy techniques. Image-guided navigation and intraoperative neuromonitoring enhance precision and safety, potentially leading to even better outcomes in the future.
Nursing Care of the Patient Undergoing Diskectomy
Nursing care for patients undergoing diskectomy is crucial to ensure optimal recovery, prevent complications, and promote patient education and psychosocial well-being. This comprehensive guide explores all aspects of nursing care throughout the preoperative, intraoperative, and postoperative phases.
Preoperative Nursing Care
Patient Assessment
- Baseline Neurological Status: Thoroughly assess and document sensory and motor function, muscle strength, pain level, and any evidence of nerve root involvement. This provides a reference for postoperative comparisons.
- Medical History and Comorbidities: Review the patient’s history for chronic illnesses (e.g., diabetes, hypertension, bleeding disorders) that may impact surgical outcomes and healing.
- Medication Review: Evaluate all current medications, including anticoagulants, steroids, NSAIDs, and herbal supplements, which may affect bleeding risk or interact with anesthetics.
Patient Education
- Explain the surgical procedure, expected outcomes, and potential risks or complications in clear, understandable language.
- Discuss the role of the patient in recovery, including the importance of early mobilization and following postoperative instructions.
- Introduce pain management strategies, such as the use of PCA (patient-controlled analgesia), oral analgesics, and non-pharmacological techniques.
- Describe postoperative restrictions, including activity limitations, wound care, braces (if necessary), and signs of complications to watch for.
- Alleviate anxiety by providing opportunities for questions, addressing misconceptions, and involving family or caregivers in discussions as appropriate.
Preparation for Surgery
- Ensure that all necessary preoperative investigations are completed (e.g., blood work, ECG, imaging studies).
- Maintain NPO (nil per os) status as ordered prior to surgery.
- Assist the patient in bathing/showering and donning a surgical gown.
- Remove jewelry, dentures, prostheses, and other personal items as required.
- Verify surgical consent and mark the operative site according to hospital policy.
Intraoperative Nursing Care
Patient Positioning and Safety
- Collaborate with the surgical team to ensure proper positioning (usually prone or lateral) to allow optimal access to the spine and prevent pressure injuries.
- Pad bony prominences and maintain alignment of the spine.
- Monitor for inadvertent nerve or tissue compression during positioning.
Infection Prevention
- Follow strict aseptic technique throughout the procedure.
- Administer prophylactic antibiotics as ordered.
Monitoring
- Monitor vital signs, oxygen saturation, and blood loss during surgery.
- Communicate any unexpected changes to the surgical or anesthesia team promptly.
Postoperative Nursing Care
Immediate Postoperative Period (PACU)
- Airway, Breathing, and Circulation (ABCs): Ensure airway patency, monitor respiratory rate, oxygen saturation, and hemodynamic stability.
- Pain Management: Assess pain using standardized scales and administer prescribed analgesics. Monitor for adverse effects and effectiveness.
- Neurological Assessment: Frequently evaluate sensory and motor function in the affected limbs, comparing findings to preoperative baseline.
- Surgical Site Monitoring: Inspect the incision for bleeding, drainage, swelling, or signs of infection.
- Positioning: Maintain the patient in a neutral spinal alignment, usually supine with a small pillow under the knees to decrease strain on the back.
- Urinary Function: Monitor for urinary retention, especially in patients who received spinal or epidural anaesthesia.
Ongoing Postoperative Care (Ward)
Pain Management:
- Continue regular pain assessments and provide analgesia as needed.
- Encourage non-pharmacological methods such as repositioning, ice/heat packs, relaxation techniques, and distraction.
- Monitor for signs of over-sedation or respiratory depression.
Neurological Monitoring:
- Perform regular checks of limb strength, sensation, and movement.
- Observe for new or worsening neurological deficits (e.g., numbness, tingling, weakness, loss of bowel/bladder control), and report changes immediately.
Prevention of Complications
- Deep Vein Thrombosis (DVT): Encourage early movement as tolerated, apply compression stockings or devices, and administer prophylactic anticoagulants as prescribed.
- Pulmonary Complications: Encourage deep breathing exercises, coughing, and use of an incentive spirometer to reduce atelectasis risk.
- Wound Care: Keep the incision site clean and dry, change dressings as per protocol, and observe for signs of infection (redness, swelling, discharge, fever).
- Prevent Pressure Ulcers: Reposition the patient regularly and inspect the skin for breakdown.
Mobility and Rehabilitation
- Follow surgeon’s instructions regarding bed rest, log-rolling techniques for turning, and gradual progression to sitting, standing, and walking.
- Collaborate with physiotherapists to develop and implement an individualised rehabilitation plan.
- Educate the patient in safe movement and the avoidance of activities that increase spinal strain (e.g., bending, twisting, lifting heavy objects).
Patient and Family Education
- Review wound care procedures, signs of infection, and when to seek medical attention.
- Discuss pain management strategies and the importance of adhering to prescribed regimens.
- Emphasise activity restrictions and the gradual return to normal activities.
- Provide written and verbal instructions for home care and follow-up appointments.
- Include family members or caregivers in teaching sessions as appropriate.
Discharge Planning
- Assess the patient’s readiness for discharge based on mobility, pain control, wound healing, and understanding of home care instructions.
- Arrange for home care services or outpatient physiotherapy if needed.
- Ensure the patient has a follow-up appointment with the surgeon or spine specialist.
- Provide contact information for questions or concerns after discharge.
Psychosocial Considerations
- Recognise the emotional impact of surgery, including anxiety, fear of recurrence, or concerns about returning to work and daily activities.
- Offer reassurance and emotional support, encouraging the patient to express concerns and ask questions.
- Facilitate communication between the patient, family, and healthcare team.
- Refer to counselling or support services if signs of depression, adjustment difficulties, or significant distress are identified.
Special Considerations
- Patients with extensive comorbidities, obesity, or advanced age may require tailored care plans and closer monitoring.
- Minimally invasive versus open diskectomy procedures may have differing protocols for pain management, mobilisation, and discharge timing.
- Monitor for recurrent symptoms, such as return of leg pain or numbness, and coordinate prompt evaluation if indicated.
Documentation
- Thoroughly document all assessments, interventions, patient responses, education provided, and communication with other team members.
- Maintain accurate records of vital signs, neurological status, wound appearance, pain levels, administered medications, and mobility progress.
REFERENCES
- American Academy of Orthopaedic Surgeons. Endoscopic Diskectomy (https://orthoinfo.aaos.org/en/treatment/endoscopic-disketcomy/). Last reviewed 7/2023.
- American Academy of Orthopaedic Surgeons. Preparing for Low Back Surgery. https://orthoinfo.aaos.org/en/treatment/preparing-for-low-back-surgery/. Last reviewed 4/2022.
- Health Education & Content Services. Spine surgery: Getting ready before and caring for yourself after. Mayo Clinic; 2019.
- Butler AJ, Munakomi S, Donnally III CJ. Discectomy (https://www.ncbi.nlm.nih.gov/books/NBK544281/). [Updated 2023 Aug 13]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Accessed 9/30/2023.
- National Library of Medicine (U.S.). Diskectomy. https://medlineplus.gov/ency/article/007250.htm. Last reviewed 6/8/2022.
- Sivakanthan S, Hasan S, Hofstetter C. Full-Endoscopic Lumbar Discectomy. https://pubmed.ncbi.nlm.nih.gov/31739919/. Neurosurg Clin N Am. 2020;31(1):1-7.
- Azar FM, et al. Degenerative disorders of the thoracic and lumbar spine. In: Campbell’s Operative Orthopaedics. 14th ed. Elsevier; 2021. https://www.clinicalkey.com.
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





