Understanding Orthognathic Surgery, Its Process, and Its Impact
Introduction
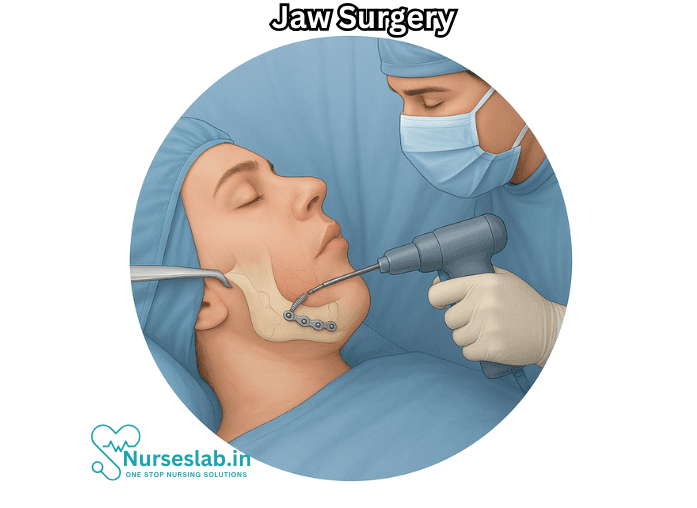
Jaw surgery, medically known as orthognathic surgery, refers to a complex procedure that corrects irregularities of the jaw bones and realigns the jaws and teeth to improve function and appearance. It is often performed by oral and maxillofacial surgeons in conjunction with orthodontic treatment. Jaw surgery can profoundly influence a person’s ability to chew, speak, and breathe, as well as enhance facial harmony and self-confidence.
What Is Jaw Surgery?
Orthognathic surgery is not a single procedure but rather a series of surgical corrections tailored to the individual’s anatomical needs. It may involve repositioning the upper jaw (maxilla), the lower jaw (mandible), or both. Sometimes, the chin is also adjusted, a procedure called genioplasty. These corrections are performed when jaw misalignments are too severe to be treated with orthodontics alone.
The Reasons for Jaw Surgery
People may require jaw surgery for various reasons, including:
- Malocclusion: Severe misalignment of teeth, such as underbite, overbite, or open bite, that cannot be resolved with braces alone.
- Facial Imbalance: Asymmetry of the face due to jaw discrepancies, such as a receding chin or jutting jaw.
- Functional Issues: Problems with chewing, biting, or swallowing; chronic jaw or temporomandibular joint (TMJ) pain; excessive wear and tear on teeth.
- Sleep Apnea: Structural abnormalities contributing to obstructive sleep apnea.
- Speech Problems: Certain jaw positions can affect the ability to speak clearly.
- Birth Defects or Trauma: Congenital conditions like cleft palate or injuries that affect jaw structure.
Types of Jaw Surgery
The three primary types of jaw surgery are:
- Maxillary Osteotomy: Surgery performed on the upper jaw (maxilla) to correct issues such as an open bite, crossbite, or significant upper jaw misalignment.
- Mandibular Osteotomy: Operations on the lower jaw (mandible), often to correct underbites or receding chins.
- Bimaxillary Osteotomy: Both the upper and lower jaws are repositioned in a single surgery for complex cases.
- Genioplasty: Surgical reshaping or repositioning of the chin, which may be performed alone or in conjunction with the above procedures.
The Jaw Surgery Process
Orthognathic surgery is a multi-stage process involving thorough planning, coordination between the oral surgeon and orthodontist, and a significant recovery period.
1. Evaluation and Planning
The journey typically begins with a comprehensive evaluation:
- Clinical examination by an orthodontist and oral surgeon.
- Dental X-rays, 3D imaging, photographs, and dental impressions.
- Simulation of jaw movements and facial profile changes using computer modeling.
- A treatment plan is devised, often in collaboration with other specialists.
2. Pre-Surgical Orthodontics
Before surgery, patients usually undergo orthodontic treatment (braces) for 12 to 18 months. This phase aligns the teeth to their optimal positions, ensuring the best fit once the jaws are realigned.
3. The Surgical Procedure
Jaw surgery is generally performed in a hospital under general anesthesia. The surgeon makes incisions inside the mouth, minimizing visible scars. Bone segments are carefully cut, repositioned, and secured with plates, screws, or wires.
Depending on the complexity, the procedure can last several hours. Common techniques include:
- Le Fort I osteotomy for upper jaw movement.
- Bilateral sagittal split osteotomy for lower jaw repositioning.
- Chin osteotomy if genioplasty is performed.
4. Hospital Stay and Early Recovery
Most patients spend one to three nights in the hospital. Post-operative care includes pain management, antibiotics to prevent infection, and instructions on oral hygiene and diet (often liquids or soft foods for several weeks).
5. Post-Surgical Orthodontics and Follow-Up
Braces are typically retained for several more months after surgery to fine-tune the bite. Regular follow-ups with the orthodontist and surgeon ensure proper healing.
Risks and Potential Complications
Like any major surgery, orthognathic surgery carries risks. These include:
- Bleeding and swelling
- Infection
- Nerve injury resulting in temporary or, rarely, permanent numbness of the lips, cheeks, or tongue
- Relapse of jaw position
- Problems with bite or jaw function
- Need for additional surgeries
- Risks associated with anesthesia
A skilled surgical team and careful planning minimize these risks.
Recovery and Aftercare
Recovery from jaw surgery is extensive and requires patience. Most people can return to school or work within two to six weeks, though full healing may take 9 to 12 months.
Key aspects of recovery:
- Swelling and bruising peak in the first week and gradually diminish.
- Pain is managed with prescribed medications and cold compresses.
- Oral hygiene is crucial; special mouth rinses and gentle brushing may be recommended.
- Diet progresses from liquids to soft foods and eventually back to regular foods as healing allows.
- Speech therapy may help with adaptation after major jaw repositioning.
- Physical therapy can improve jaw function and mobility.
Benefits of Jaw Surgery
While the journey can be challenging, jaw surgery offers numerous benefits:
- Enhanced facial appearance and symmetry
- Improved bite, chewing, and swallowing
- Clearer speech
- Relief from pain or discomfort related to jaw disorders
- Better long-term oral health by preventing uneven wear and TMJ problems
- Increased self-confidence and quality of life
Alternative Treatments
Not all jaw discrepancies require surgery. Alternatives may include:
- Orthodontic appliances (like expanders or functional appliances) for growing children
- Braces or clear aligners for minor misalignments
- Dental restorations or prosthetics to adjust bite relationships
- Non-surgical management for sleep apnea (e.g., CPAP devices)
Your oral healthcare team will determine the best approach based on your individual case.
Jaw Surgery and Mental Health
Undergoing jaw surgery, especially for visible facial concerns, can significantly affect a person’s mental and emotional health. Many patients report increased self-esteem and satisfaction post-procedure, but the prolonged process and recovery may also trigger anxiety or depression. Access to counseling or support groups during recovery can be beneficial.
Cost and Insurance Considerations
The cost of jaw surgery varies widely depending on geographical location, the complexity of the case, hospital fees, and insurance coverage. Some insurance providers cover all or part of the cost if the surgery is deemed medically necessary (e.g., to correct functional problems), but not for purely cosmetic reasons. It is crucial to consult with your healthcare provider and insurance company for a detailed assessment.
Nursing Care of the Patient with Jaw Surgery
The procedure not only improves the function and appearance of the jaws but also enhances overall oral health. Nursing care plays a pivotal role in ensuring a smooth recovery and minimizing complications for patients undergoing jaw surgery.
Preoperative Nursing Care
1. Patient Assessment
- Medical History: Collect a thorough medical, dental, and surgical history, including allergies, history of bleeding disorders, and previous anesthesia reactions.
- Medication Review: Note current medications, especially anticoagulants, antiplatelets, and herbal supplements that may affect bleeding or healing.
- Psychosocial Assessment: Assess the patient’s understanding of the procedure, expectations, anxiety, and support systems. Address psychological preparation and coping mechanisms.
2. Preoperative Education
- Procedure Explanation: Provide detailed information about the surgical process, expected duration, anesthesia, and postoperative course in understandable terms.
- Nutritional Guidance: Instruct patients about the transition to a liquid or soft diet after surgery and the importance of adequate nutrition for healing.
- Oral Hygiene: Educate patients on maintaining meticulous oral hygiene prior to surgery to reduce the risk of postoperative infection.
- Preoperative Fasting: Reinforce instructions regarding fasting (NPO status) as per anesthesiologist guidelines.
- Preoperative Testing: Ensure completion of laboratory tests, imaging, and consent forms.
3. Physical Preparation
- Administer prescribed preoperative medications, such as prophylactic antibiotics or anxiolytics.
- Assist with oral rinses or tooth brushing to minimize oral bacterial load.
- Ensure removal of dentures, jewelry, and contact lenses before surgery.
- Verify patient identification and surgical site as part of the safety checklist.
Immediate Postoperative Nursing Care
1. Airway Management
Maintaining a patent airway is the foremost priority following jaw surgery, as postoperative swelling and bleeding may compromise breathing.
- Monitor for signs of airway obstruction, such as stridor, use of accessory muscles, or cyanosis.
- Position the patient in a semi-Fowler’s or upright position to decrease edema and promote drainage.
- Keep suction equipment at the bedside to clear secretions effectively and prevent aspiration.
- Be prepared to perform emergency interventions, including airway repositioning, if indicated.
2. Monitoring and Assessment
- Frequently assess vital signs (temperature, pulse, blood pressure, respiratory rate, oxygen saturation).
- Observe for excessive bleeding, hematoma formation, or surgical site infection.
- Assess the patient’s level of consciousness and response to stimuli following anesthesia.
- Evaluate for any signs of nerve injury, such as numbness or weakness around the jaw, lips, or tongue.
3. Pain Management
- Administer prescribed analgesics as needed, considering both pharmaceutical and non-pharmacological options (ice packs, relaxation techniques).
- Assess pain regularly using appropriate scales and document the patient’s response to interventions.
- Educate patients about the expected nature of pain and methods to manage it effectively.
4. Fluid and Nutrition Management
- Start with intravenous fluids as ordered until the patient is able to tolerate oral intake.
- Gradually advance to clear liquids, full liquids, and then soft or pureed foods as tolerated and prescribed.
- Monitor intake and output, and observe for signs of dehydration or electrolyte imbalance.
- Instruct the patient to drink fluids with a straw only if permitted by the surgeon, as suction can sometimes disrupt the surgical site.
5. Wound and Oral Care
- Maintain strict oral hygiene to prevent infection by providing gentle mouth rinses as ordered, avoiding vigorous rinsing or brushing near the surgical site.
- Monitor the incision site for redness, swelling, discharge, or foul odor.
- Apply cold compresses externally to reduce swelling during the initial 24-48 hours.
- Teach the patient not to disturb any sutures, drains, or fixation devices (such as arch bars or wires).
6. Communication Support
- Assess the patient’s ability to speak; if jaw fixation is present, provide alternative communication tools (writing pads, communication boards, or digital devices).
- Facilitate communication with family and healthcare team members to alleviate anxiety and confusion.
7. Prevention of Complications
- Monitor for signs and symptoms of infection (fever, increased pain, pus).
- Observe for deep vein thrombosis, especially if mobility is reduced postoperatively.
- Educate the patient and family about symptoms that warrant immediate medical attention.
Ongoing Postoperative Nursing Care
1. Education and Self-Care Training
- Instruct the patient on safe oral hygiene measures, such as using soft toothbrushes or prescribed mouthwashes.
- Educate about dietary modifications, emphasizing the need for high-calorie, high-protein foods in liquid or soft form to support healing.
- Teach techniques for pain management, wound care, and the importance of follow-up appointments.
- Explain the rationale for activity restrictions and provide guidance on gradual return to normal activities.
2. Emotional and Psychological Support
- Address concerns related to body image, speech changes, or altered appearance post-surgery.
- Provide reassurance, encourage expression of emotions, and refer to counseling services if needed.
- Support the patient in adjusting to lifestyle changes resulting from jaw fixation or altered oral intake.
3. Long-term Monitoring
- Schedule regular follow-ups to monitor healing, nutrition, and overall recovery.
- Assess for chronic complications, such as persistent numbness, malocclusion, or infection.
- Coordinate with dietitians, speech therapists, and physiotherapists for comprehensive rehabilitation.
Special Considerations
1. Patients with Jaw Fixation
- Maintain wire cutters or scissors at the bedside in the event of vomiting or airway obstruction, as per institutional policy.
- Educate the patient and family about emergency protocols if jaw fixation must be released outside the hospital.
- Emphasize the importance of not inserting objects into the mouth that could damage fixation devices.
2. Pediatric and Geriatric Patients
- Adapt care plans to address developmental and cognitive differences in pediatric patients, providing age-appropriate education and emotional support.
- For older adults, monitor closely for delirium, dehydration, and delayed wound healing.
Discharge Planning
- Provide written and verbal instructions regarding oral hygiene, wound care, medication management, and dietary guidelines.
- Ensure that the patient and caregivers understand signs of complications and know when and how to seek medical attention.
- Arrange follow-up appointments and referrals as needed for ongoing care.
REFERENCES
- Al-Asfour A, Waheedi M, Koshy S. Survey of patient experiences of orthognathic surgery: health-related quality of life and satisfaction., https://pubmed.ncbi.nlm.nih.gov/29373200/. Int J Oral Maxillofac Surg. 2018 Jun;47(6):726-731.
- American Academy of Oral and Maxillofacial Surgeons. Corrective Jaw Surgery., https://myoms.org/what-we-do/corrective-jaw-surgery/. Last updated 4/2021.
- American Society of Plastic Surgeons. Orthognathic Surgery., https://www.plasticsurgery.org/reconstructive-procedures/orthognathic-surgery/glossary.
- Yan A, Chen YR. Orthognathic Surgery to Enhance the Smile., https://pubmed.ncbi.nlm.nih.gov/36396264/. Clin Plast Surg. 2023 Jan;50(1):81-89.
- Mayo Clinic Staff. (2018). Jaw surgery.
https://www.mayoclinic.org/tests-procedures/jaw-surgery/about/pac-20384990 - Zammit D, Ettinger RE, Sanati-Mehrizy P, Susarla SM. Current Trends in Orthognathic Surgery., https://pubmed.ncbi.nlm.nih.gov/38138203/. Medicina (Kaunas). 2023 Nov 30;59(12):2100.
- Cote CJ, et al., eds. Mandibular skeletal orthognathic surgery. In: A Practice of Anesthesia for Infants and Children. 7th edition. Elsevier; 2022. https://www.clinicalkey.com.
- Kwon T-G, et al. Current status of surgery first approach (part II): Precautions and complications. Maxillofacial Plastic and Reconstructive Surgery. 2019; doi:10.1186/s40902-019-0206-4.
- Yan A, et al. Orthognathic surgery to enhance the smile. Clincs in Plastic Surgery. 2022; doi:10.1016/j.cps.2022.07.001.
- Zammit D, et al. Current trends in orthognathic surgery. Medicina. 2023; doi:10.3390/medicina59122100.
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





