Introduction
Microsurgical Testicular Sperm Extraction, commonly abbreviated as microTESE, stands as a beacon of hope for individuals and couples facing the challenges of male infertility. This advanced surgical procedure is meticulously designed to retrieve sperm directly from the testicular tissue using high-magnification microscopy. Primarily utilized in cases of non-obstructive azoospermia—a condition where no sperm is present in the ejaculate due to impaired or absent sperm production—microTESE offers the prospect of biological parenthood where other methods have failed.
Background and Rationale
Infertility affects millions around the globe, with male factors contributing to nearly half of all cases. Among these, azoospermia is a particularly daunting diagnosis, classified into two types: obstructive and non-obstructive. While obstructive azoospermia arises from physical blockages in the male reproductive tract, non-obstructive azoospermia (NOA) is the result of inadequate sperm production within the testicles themselves.
Traditional methods for sperm retrieval, such as Testicular Sperm Aspiration (TESA) and Testicular Sperm Extraction (TESE), involve blindly extracting testicular tissue or fluid in search of sperm. However, these approaches often yield low success rates, especially in NOA cases, due to the patchy nature of sperm production. Recognizing the need for increased precision, microTESE emerged, leveraging microsurgical techniques to identify and selectively extract seminiferous tubules most likely to contain sperm, thereby maximizing the likelihood of retrieval while minimizing tissue damage.
Indications for microTESE
MicroTESE is primarily indicated for men diagnosed with non-obstructive azoospermia, particularly when:
- Genetic or idiopathic factors compromise sperm production within the testicles.
- Previous attempts at sperm retrieval (TESA, TESE) have failed or yielded insufficient sperm for assisted reproduction.
- Patients seek to use their own sperm in assisted reproductive technologies, such as Intracytoplasmic Sperm Injection (ICSI).
It may also be considered in certain cases of obstructive azoospermia where other retrieval methods are contraindicated or unsuccessful, though this scenario is less common.
The microTESE Procedure: Step by Step
Preoperative Preparation
Prior to microTESE, patients undergo comprehensive evaluation:
- Blood tests to assess hormone levels (FSH, LH, testosterone).
- Genetic screening for conditions such as Klinefelter syndrome or Y-chromosome microdeletions.
- Imaging studies (ultrasound) to evaluate testicular structure and volume.
- Consultation with reproductive endocrinology and andrology specialists to discuss risks, benefits, and alternatives.
Surgical Technique
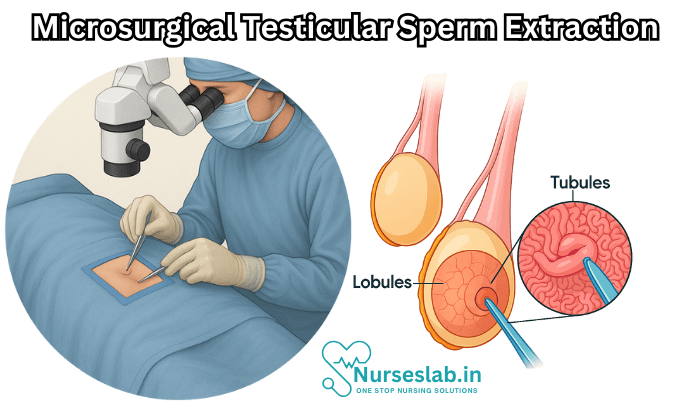
MicroTESE is typically performed under general anesthesia in a sterile operating room. The procedure involves the following steps:
- The surgeon makes a small incision in the scrotal skin and delivers the testicle for examination.
- Using an operating microscope capable of 20-25x magnification, the surgeon identifies and isolates seminiferous tubules that appear more likely to contain sperm—these are usually larger and more opaque.
- Selected tubules are carefully excised, minimizing removal of normal tissue.
- Extracted tissue samples are handed off to an embryologist, who immediately examines them under high-powered microscopy to search for viable sperm.
- If sperm are found, they are processed and cryopreserved for use in assisted reproduction, most commonly with ICSI.
- The testicle is meticulously reconstructed, and the incision is closed with fine sutures.
Duration and Recovery
The duration of microTESE varies depending on the complexity of the individual’s testicular architecture and the ease of sperm retrieval. Generally, the procedure lasts one to three hours. Recovery is typically swift, with most patients able to return to light activities within a few days, although physical exertion and sexual activity should be avoided for several weeks.
Outcomes and Success Rates
MicroTESE has revolutionized the management of non-obstructive azoospermia, offering significantly higher success rates compared to conventional sperm retrieval techniques. Success, in this context, is defined by the identification and extraction of viable sperm suitable for fertilization through ICSI.
Several factors influence the likelihood of success:
- Underlying etiology of azoospermia (genetic vs. idiopathic).
- Testicular volume and histology.
- Patient age and hormonal profile.
- Surgeon experience and facility resources.
Reported sperm retrieval rates with microTESE range from 40% to 60% in men with NOA, compared to less than 30% with blind techniques (TESA/TESE). The quality of sperm obtained may be low, but even a single viable sperm can result in fertilization and pregnancy when combined with advanced reproductive technologies.
Risks and Complications
As a microsurgical procedure, microTESE is considered safe with a low rate of serious complications. Nevertheless, patients must be informed of potential risks:
- Postoperative pain and swelling: Mild to moderate discomfort is common and typically resolves within days.
- Infection: Rare due to sterile technique, but possible at the incision site or within the testicle.
- Bleeding or hematoma: Accumulation of blood may require intervention if severe.
- Testicular damage: Although minimal with microTESE, excessive tissue removal could affect hormone production or lead to atrophy in rare cases.
- Anesthesia-related risks: Standard risks apply, including allergic reactions and breathing difficulties.
Most complications are minor and temporary, with permanent damage being extremely rare in the hands of experienced microsurgeons.
Patient Experience and Counselling
Embarking on microTESE is both a medical and emotional journey. Patients and their partners should receive thorough counselling regarding:
- Likelihood of sperm retrieval based on personal medical history.
- Alternative options if microTESE is unsuccessful, such as donor sperm or adoption.
- Ethical, psychological, and financial considerations.
- Potential need for multiple procedures or attempts.
Reproductive psychologists and counsellors are often part of the care team, supporting patients through the decision-making process and, if necessary, addressing grief or disappointment if results are unfavorable.
microTESE and Assisted Reproductive Technology (ART)
The sperm retrieved via microTESE are usually not motile or sufficient for conventional in vitro fertilization (IVF). Instead, Intracytoplasmic Sperm Injection (ICSI) is employed, wherein a single sperm is directly injected into an egg to facilitate fertilization. This technique has enabled thousands of couples to achieve pregnancy and experience parenthood despite severe male infertility.
Sperm can be used fresh (within hours of retrieval) or frozen for future cycles. Success rates for pregnancy using microTESE-derived sperm and ICSI are comparable to those using sperm from men with less severe infertility, although outcomes vary with maternal age and other factors.
Nursing Care of Patients Undergoing Microsurgical Testicular Sperm Extraction (microTESE)
This advanced procedure has revolutionized the management of male infertility, offering hope to individuals and couples seeking biological parenthood through assisted reproductive technologies such as Intracytoplasmic Sperm Injection (ICSI). Due to the delicate nature of microTESE and the psychological impact of infertility, holistic and skilled nursing care is critical for positive patient outcomes.
Preoperative Nursing Care
Patient Assessment and Preparation
- Medical History: Obtain a thorough health history, including previous surgeries, comorbid conditions (e.g., diabetes, hypertension), allergies, and current medications (especially anticoagulants).
- Psychosocial Assessment: Assess emotional status, coping mechanisms, and support systems. Infertility treatments can cause significant psychological stress, and patients may experience anxiety, depression, or feelings of inadequacy.
- Informed Consent: Ensure the patient fully understands the procedure, its purpose, risks, benefits, and alternatives. Address any questions or concerns and confirm that the consent form is signed and documented.
Preoperative Instructions
- Fasting: Advise the patient on preoperative fasting guidelines, usually nothing by mouth (NPO) for at least 6-8 hours before surgery, depending on anesthesia requirements.
- Medication Management: Instruct the patient about withholding or continuing medications as per the physician’s orders, especially anticoagulants, antiplatelets, or diabetes medications.
- Personal Hygiene: Guide the patient to shower and perform genital hygiene before admission. Shaving is typically performed in the operating room to reduce infection risk.
- Preoperative Laboratory Testing: Ensure completion of relevant investigations such as CBC, coagulation profile, blood glucose, and infectious disease screening as ordered.
- Preoperative Checklist: Confirm all documentation, identification, and allergy bands are in place. Remove jewelry and secure valuables.
Emotional Support
- Counseling: Offer counseling or referral to a mental health professional if the patient expresses significant distress.
- Patient Education: Explain the surgical process, expected recovery, and possible complications in simple terms to reduce anxiety and promote cooperation.
- Partner/Family Involvement: Encourage the involvement of partners or family members for emotional support and shared understanding.
Intraoperative Nursing Care
Patient Safety and Positioning
- Verification: Confirm patient identity, correct procedure, and surgical site before anesthesia induction as part of the surgical safety checklist.
- Positioning: Assist in placing the patient in the appropriate supine position with careful padding of pressure points to prevent nerve injury and maintain comfort.
Infection Prevention
- Sterile Technique: Ensure strict adherence to aseptic and sterile techniques throughout the procedure to minimize infection risk.
- Skin Preparation: Assist with antiseptic skin preparation of the scrotal area as per protocol.
Intraoperative Monitoring
- Vital Signs: Continuously monitor heart rate, blood pressure, oxygen saturation, and respiratory status.
- Fluid Balance: Record input and output to detect any imbalances.
- Documentation: Maintain accurate intraoperative records of medications, fluids, and any notable events.
Support for Surgical Team
- Instrument Handling: Prepare and provide microsurgical instruments, maintaining a clear and organized field.
- Specimen Management: Handle and label testicular tissue samples meticulously for prompt transfer to the embryology laboratory.
Postoperative Nursing Care
Immediate Postoperative Care
- Recovery Room Monitoring: Observe the patient in the post-anesthesia care unit (PACU) until fully awake. Monitor for airway patency, hemodynamic stability, and pain control.
- Pain Management: Assess pain using appropriate scales and administer prescribed analgesics. Non-pharmacologic methods such as ice packs or scrotal support may also be advised.
- Vital Signs: Monitor temperature, pulse, respiratory rate, and blood pressure regularly to detect complications early.
- Wound Assessment: Inspect the surgical site for bleeding, hematoma formation, or signs of infection (redness, swelling, discharge).
Patient Education and Discharge Planning
- Wound Care: Instruct the patient to keep the surgical site dry and clean. Change dressings as directed and observe for signs of infection.
- Activity Restrictions: Advise light activity and avoidance of strenuous exercise, heavy lifting, or sexual activity until cleared by the surgeon (usually 1–2 weeks).
- Pain and Swelling: Explain that mild pain and scrotal swelling are common and typically subside within a few days. Recommend supportive underwear or scrotal support devices.
- Medication Instructions: Review prescriptions for antibiotics, analgesics, and any other supportive medications. Emphasize adherence to prescribed regimens.
- Signs of Complications: Educate about symptoms that require immediate medical attention, such as severe pain, excessive swelling, fever, purulent discharge, or difficulty urinating.
- Follow-up Appointments: Stress the importance of attending all scheduled follow-ups for wound assessment, suture removal (if needed), and discussion of laboratory results (sperm retrieval outcomes).
Emotional and Psychological Support
- Empathetic Communication: Provide a supportive environment for discussing concerns about fertility, sexual function, or anxieties related to the procedure or its results.
- Referral to Counseling: Recommend professional counseling or support groups for individuals and couples undergoing infertility treatment, as emotional distress is common.
Potential Complications and Nursing Interventions
- Hematoma: Monitor for scrotal swelling and discoloration. Apply ice packs as prescribed and elevate the scrotum. Notify the surgeon if signs worsen.
- Infection: Maintain aseptic technique during dressing changes. Watch for fever, redness, or discharge from the incision. Administer antibiotics as ordered.
- Pain: Provide regular pain assessment and timely analgesia. Encourage the use of supportive briefs.
- Psychological Impact: Address anxiety or depressive symptoms proactively and involve mental health professionals as needed.
- Delayed Wound Healing: Promote adequate nutrition and hydration. Monitor and report any issues with wound closure or persistent drainage.
Special Considerations
- Confidentiality: Respect patient privacy regarding infertility diagnosis and treatment at all times.
- Cultural Sensitivity: Be aware of and sensitive to cultural beliefs about fertility, masculinity, and reproductive health.
- Documentation: Maintain thorough, accurate, and timely records of all nursing interventions, assessments, and patient education provided.
REFERENCES
- American Society for Reproductive Medicine. Surgical Techniques for Sperm Retrieval: What Should I Know. https://www.reproductivefacts.org/news-and-publications/fact-sheets-and-infographics/surgical-techniques-for-sperm-retrieval-what-should-i-know? Last revised 2015.
- Flannigan R, Bach PV, Schlegel PN. Microdissection testicular sperm extraction. Transl Androl Urol. 2017 Aug;6(4):745-752. doi: 10.21037/tau.2017.07.07. PMID: 28904907; PMCID: PMC5583061.
- American Urological Association. What Is Sperm Retrieval. https://www.urologyhealth.org/urology-a-z/s/sperm-retrieval?
- Esteves SC. Microdissection TESE versus Conventional TESE for Men with Nonobstructive Azoospermia Undergoing Sperm Retrieval. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9060172/. Int Braz J Urol. 2022 May-Jun;48(3):569-578.
- Spahovic H, Alic J, Göktolga Ü, et al. “Second-look” Micro Testicular Sperm Extraction (MicroTESE) in Patients with Non-obstructive Azoospermia Following Histopathological Analysis. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7520053/). Med Arch. 2020 Aug;74(4):279-284.
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





