Robotic hernia surgery is a minimally invasive procedure that uses robotic-assisted technology to repair hernias. The surgeon operates from a console, controlling robotic instruments that offer enhanced precision, dexterity, and visualization. The herniated tissue is repositioned, and a synthetic mesh is often placed to reinforce the abdominal wall.
Introduction
Hernia surgery has evolved dramatically over the past several decades, moving from open repairs to minimally invasive laparoscopic techniques, and now, to the cutting edge of robotic-assisted procedures. Robotic hernia surgery represents a synthesis of technological advancement and surgical expertise, offering new opportunities for precision, flexibility, and patient outcomes. This document provides an in-depth exploration of robotic hernia surgery, its advantages, the technology involved, indications and contraindications, procedural steps, recovery, risks, and the future of this innovative surgical approach.
Understanding Hernias
A hernia occurs when an internal part of the body pushes through a weakness in the muscle or surrounding tissue wall. The most common types of hernias include inguinal (groin), umbilical (belly button), incisional (resulting from previous surgery), femoral (upper thigh), and hiatal (upper stomach).
Hernias may cause discomfort, pain, or more serious complications such as strangulation of the protruding tissue, requiring surgical intervention. While some hernias may be watched or managed conservatively, surgical repair is the definitive treatment for most cases.
The Evolution of Hernia Surgery
Traditionally, hernias were repaired using open procedures, which required large incisions to access the herniated tissue. This approach, while effective, was associated with significant postoperative pain, longer hospital stays, and slower recovery.
With the advent of laparoscopic techniques, surgeons could repair hernias through a few small incisions using a camera and specialized instruments. Laparoscopy reduced many of the drawbacks of open surgery—minimizing scarring, shortening hospital stays, and speeding up recovery. However, laparoscopic surgery also presented challenges: the instruments were rigid, the field of vision was two-dimensional, and dexterity was limited compared to open surgery.
Robotic surgery builds upon the foundations of laparoscopy, addressing many of its limitations.
Robotic Surgery: An Overview
Robotic surgical systems, such as the da Vinci Surgical System, provide surgeons with a high-definition, three-dimensional view of the surgical site and wristed instruments that can mimic the range of motion of a human hand. The surgeon operates from a console, manipulating joysticks and foot pedals, which translate movements with sub-millimeter precision.
Key features of robotic surgical systems include:
- Enhanced Visualization: 3D, high-definition optics provide unparalleled clarity and depth perception.
- Improved Dexterity: Robotic instruments rotate and bend beyond the capacity of human wrists, allowing for meticulous dissection and suturing.
- Stability and Precision: The system filters out hand tremors, ensuring steady and accurate movements.
- Ergonomics: Surgeons can operate while seated at a console, reducing fatigue during complex or lengthy procedures.
Robotic Hernia Surgery: Indications and Candidacy
Robotic hernia repair is suitable for a wide range of hernia types, including:
- Inguinal hernias
- Ventral or incisional hernias
- Umbilical hernias
- Recurrent hernias (after previous repair)
- Complex or large hernias
Ideal candidates for robotic hernia surgery are individuals seeking minimally invasive repair, especially those with complex or recurrent hernias, obesity, or multiple previous abdominal surgeries. Not all patients are suitable; contraindications may include uncontrolled bleeding disorders, severe cardiopulmonary disease, or inability to tolerate anesthesia or pneumoperitoneum (the inflation of the abdomen with gas required for the procedure).
Preoperative Preparation
Preparation for robotic hernia surgery typically involves:
- A thorough medical evaluation, including imaging studies (such as ultrasound or CT scan) to assess the hernia’s size and location.
- Counseling on the risks, benefits, and alternatives to surgery.
- Preoperative instructions regarding fasting, medication management, and arranging for postoperative support.
The Robotic Hernia Repair Procedure
1. Anesthesia and Positioning
Patients undergo general anesthesia. The patient is positioned to optimize access to the hernia, usually lying flat with arms tucked and legs apart.
2. Port Placement and Access
Several small incisions—typically ranging from 5 to 12 mm—are made in the abdomen to accommodate the robotic instruments and camera. The abdominal cavity is insufflated with carbon dioxide gas to create working space.
3. Docking the Robot
The robotic arms are brought to the operating table and docked to the ports. The surgeon moves to the console, gaining control over the camera and instruments.
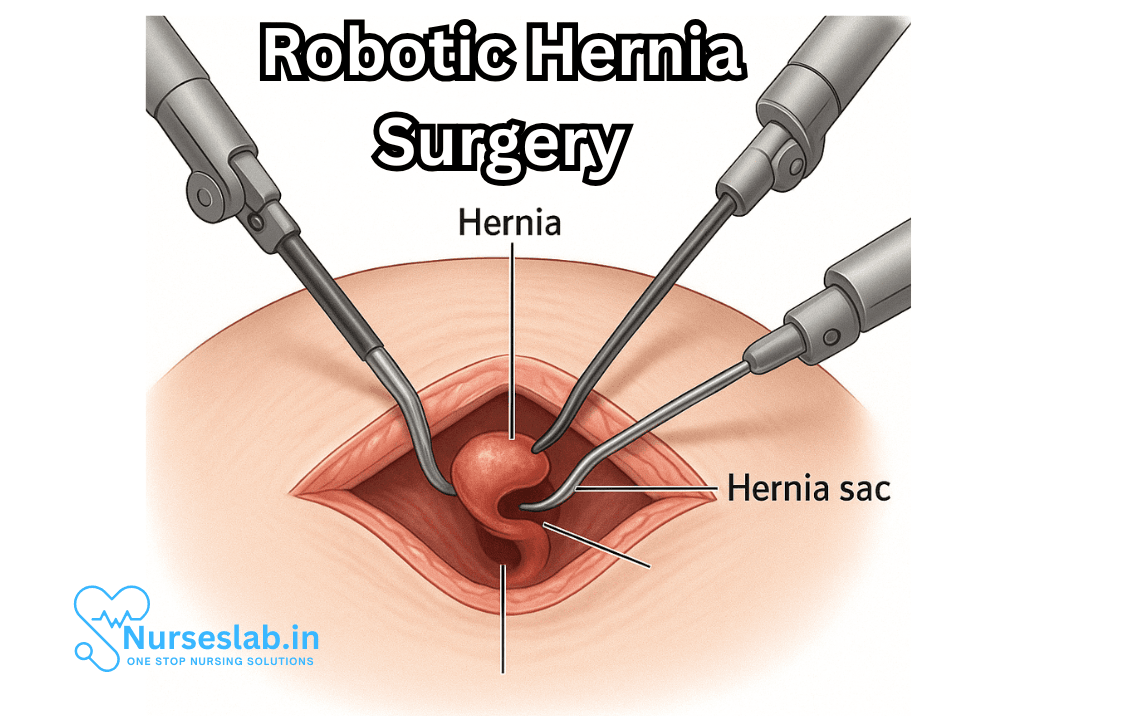
4. Hernia Reduction and Sac Dissection
The herniated tissue is gently reduced back into its correct anatomical position. The hernia sac (the protruding tissue) is dissected away from surrounding structures.
5. Mesh Placement and Closure
A synthetic mesh is often used to reinforce the weakened area. The mesh is positioned and secured using sutures, tacks, or glue. The defect is closed with meticulous suturing, and the instruments are withdrawn. The small incisions are closed with sutures or surgical glue.
Special Techniques in Robotic Hernia Repair
Robotic surgery allows for advanced reconstructive techniques, such as posterior component separation or transversus abdominis release (TAR), which can be vital in large or complex ventral hernias.
Benefits of Robotic Hernia Surgery
Robotic hernia repair offers several advantages compared to traditional open or even laparoscopic procedures:
- Smaller incisions and less scarring
- Reduced postoperative pain
- Shorter hospital stays and faster return to normal activity
- Lower risk of infection and wound complications
- Enhanced precision, particularly in complex or recurrent cases
- Improved visualization for challenging anatomical locations
Several studies have demonstrated that robotic techniques may offer improved outcomes, especially for patients with obesity, recurrent hernias, or large abdominal wall defects.
Risks and Considerations
As with any surgery, robotic hernia repair carries potential risks:
- Bleeding or infection
- Injury to surrounding organs (bowel, bladder, blood vessels)
- Hernia recurrence
- Chronic pain or discomfort
- Complications related to anesthesia
- Technical difficulties or need to convert to open surgery
Robotic surgery is generally very safe. However, the cost and availability of robotic systems may limit access in some settings, and not all surgeons are trained in these advanced techniques.
Recovery After Robotic Hernia Surgery
Recovery is typically swift compared to open surgery. Most patients can return home the same day or after a short hospital stay. Full recovery varies based on the size and type of hernia repaired and the patient’s overall health, but many can resume light activities within a week and more strenuous pursuits within a few weeks.
Postoperative care includes:
- Pain management (often requiring less medication than open surgery)
- Wound care instructions
- Early mobilization to reduce risk of blood clots
- Follow-up appointments to monitor for complications or recurrence
Comparing Robotic, Laparoscopic, and Open Hernia Repairs
While laparoscopic and robotic approaches are both minimally invasive, robotics provides enhanced dexterity, visualization, and ergonomic comfort for the surgeon, possibly translating to better outcomes in complex cases. However, robotic procedures may take longer and are generally more costly due to the sophisticated equipment.
Open repairs are still appropriate in specific situations, such as very large or strangulated hernias, or when minimally invasive techniques are contraindicated.
The Future of Robotic Hernia Surgery
Robotic technology is rapidly advancing. Future systems are expected to become more compact, affordable, and accessible, with improved haptic feedback, artificial intelligence assistance, and integration with advanced imaging modalities. Ongoing research is evaluating long-term outcomes, cost-effectiveness, and patient satisfaction.
Patient Perspectives and Informed Decision-Making
Patients considering hernia repair should have thorough discussions with their surgeons about all available options, the risks and benefits of each approach, and the surgeon’s experience with robotic procedures. Informed, shared decision-making is vital to achieving the best possible outcome
Nursing Care for Patients Undergoing Robotic Hernia Surgery
Nurses are pivotal in ensuring patient safety, promoting healing, preventing complications, and supporting patients’ emotional and physical well-being throughout the surgical journey.
Understanding Robotic Hernia Surgery
Robotic hernia surgery utilizes a surgical robot, typically controlled by a skilled surgeon from a console. The device translates the surgeon’s hand movements into precise actions using tiny instruments introduced into the patient’s body through small incisions. Common indications for robotic hernia repair include inguinal, ventral, and incisional hernias.
The robotic approach offers several advantages:
- Enhanced visualization with 3D imaging
- Greater dexterity and range of motion for the surgeon
- Reduced postoperative pain and scarring
- Shorter hospital stays and faster return to normal activities
Nursing care must be tailored to the unique requirements of this surgical modality, addressing the patient holistically from admission to discharge.
Preoperative Nursing Care
Patient Assessment and Preparation
The nurse begins by conducting a thorough assessment, including medical history, allergies, medication review, and previous surgical procedures. Key considerations include:
- Evaluating risk factors such as obesity, smoking, diabetes, and cardiovascular conditions that may influence surgical outcomes or wound healing.
- Education: Nurses provide detailed information about the robotic procedure, expected outcomes, potential risks, and benefits. Addressing patient concerns and clarifying misconceptions helps reduce anxiety and fosters cooperation.
- Preoperative instructions: The patient is instructed to fast before surgery and may need to discontinue certain medications (such as anticoagulants or NSAIDs) to lower bleeding risk. Bowel preparation may be required for certain types of hernia repairs.
Emotional Support
Robotic surgery can be daunting for some patients. Nurses offer empathetic support, encourage questions, and provide reassurance regarding the safety and efficacy of the technology. If needed, nurses facilitate communication with the surgical team for additional clarification.
Physical Preparation
- Skin preparation: The planned surgical site is cleansed with antiseptic agents to minimize infection risk.
- Preoperative vital signs are recorded, and baseline laboratory investigations are reviewed.
- Patient positioning: Nurses ensure the patient is comfortable, with proper padding and alignment, to prevent pressure injuries during surgery.
- IV access: Initiate intravenous lines for administration of fluids, medications, and anesthesia.
Intraoperative Nursing Care
Operating Room Preparation
Nurses collaborate with the surgical team to prepare the robotic system, ensuring all instruments and equipment are sterile, functioning, and available. They also perform time-out procedures to verify patient identity, surgical site, and planned intervention.
Patient Monitoring and Safety
- Continuous monitoring of vital signs (heart rate, blood pressure, oxygen saturation, respiratory rate) is crucial.
- Nurses watch for adverse reactions to anesthesia and intervene promptly if necessary.
- Careful attention is given to the patient’s positioning to prevent nerve injury or pressure ulcers, as robotic procedures may be lengthy.
- Documentation of intraoperative events, medication administration, and fluid balance is meticulously maintained.
Communication
Nurses act as the patient’s advocate, alerting the surgical team to any changes in status and facilitating efficient teamwork throughout the procedure.
Postoperative Nursing Care
After robotic hernia surgery, attentive nursing care is essential to promote healing, detect complications early, and support recovery.
Immediate Postoperative Care
- Monitoring in Recovery: The patient is transferred to the post-anesthesia care unit (PACU), where nurses continuously monitor vital signs, oxygenation, pain level, and consciousness.
- Pain Management: Robotic surgery typically results in less pain than open procedures, but adequate pain control is still vital. Nurses administer prescribed analgesics and assess pain using standardized scales.
- Incision Site Assessment: Nurses check the surgical site for bleeding, swelling, drainage, or signs of infection. Dressings are monitored and changed as needed, following aseptic technique.
- Prevention of Complications: Nurses are vigilant for early signs of complications such as hemorrhage, deep vein thrombosis (DVT), urinary retention, and respiratory issues.
Promoting Early Recovery
- Mobilization: Encouraging early ambulation reduces the risk of DVT and promotes bowel function. Nurses assist patients in sitting up, standing, and walking as tolerated.
- Nutrition: Once the patient is fully awake and nausea is controlled, oral intake is gradually resumed. Nurses educate patients about the importance of hydration and balanced nutrition for wound healing.
- Respiratory Exercises: Deep breathing and coughing exercises help prevent postoperative pulmonary complications, especially in patients with a history of respiratory disease.
Patient Education
Education is a cornerstone of nursing care in robotic hernia surgery. Nurses provide detailed discharge instructions regarding:
- Incision care: How to keep the surgical site clean and dry, recognize signs of infection, and when to change dressings.
- Activity restrictions: Guidance on lifting, exercise, driving, and return to work, tailored to the specific procedure performed.
- Pain management: Use of prescribed medications, non-pharmacological techniques, and when to seek help for uncontrolled pain.
- Symptoms requiring immediate attention: Educate patients on warning signs such as fever, severe pain, redness, swelling, drainage, or difficulty urinating.
- Follow-up appointments: The importance of attending scheduled check-ups for suture removal, wound assessment, and evaluation of recovery progress.
Complication Prevention and Management
Nurses play a crucial role in the early identification and management of complications associated with robotic hernia surgery. Common risks include:
- Infection: Prevented by strict aseptic technique during dressing changes and careful monitoring for redness, heat, or drainage.
- Bleeding: Nurses monitor for abnormal bruising or swelling at the incision site and notify the surgical team promptly.
- Hernia Recurrence: Education about activity modifications and adherence to postoperative guidelines helps minimize recurrence risk.
- Venous Thromboembolism: Early mobilization, use of compression devices, and pharmacologic prophylaxis as prescribed.
- Urinary Retention: Monitoring for adequate urine output and assisting with voiding as needed; catheterization if indicated.
Psycho-social Support and Holistic Care
Beyond physical care, nurses address the psychological and emotional needs of patients. Fear, anxiety, and concerns about recovery are common. Nurses provide resources for emotional support, facilitate family involvement, and connect patients with support groups if desired. Culturally sensitive care and respect for individual preferences are essential throughout the perioperative period.
Discharge Planning
Effective discharge planning ensures continued recovery at home and reduces the risk of readmission. Nurses coordinate with multidisciplinary teams including physicians, therapists, and social workers to create individualized care plans. This includes:
- Ensuring the patient understands medication regimens and wound care instructions
- Arranging home health services if needed for wound care, mobility assistance, or rehabilitation
- Providing contact information for urgent issues and scheduling follow-up visits
Documentation
Accurate documentation is vital for continuity of care. Nurses record all assessments, interventions, patient responses, medication administration, and discharge instructions. This legal record supports quality assurance, communication among healthcare providers, and future treatment decisions.
REFERENCES
- Armijo PR, Pokala B, Flores L, Hosein S, Oleynikov D. Current state of robotic use in inguinal hernia repair: a survey of minimally invasive hernia surgeons. https://pubmed.ncbi.nlm.nih.gov/32141046/. Updates Surg. 2020;72(1):179-184.
- Das C, Jamil T, Stanek S., et al. Inguinal hernias. In: Brunicardi F, Andersen DK, Billiar TR, et al., eds. Schwartz’s Principles of Surgery. 11th ed. New York, NY: McGraw Hill; 2019.
- Collins CE, Renshaw S, Huang LC. Robotic vs open approach for older adults undergoing retromuscular ventral hernia repair. Ann Surg. 2023;277(4):697–703.
- Kudsi OY, McCarty JC, Paluvoi N, Mabardy AS. Transition from laparoscopic totally extraperitoneal inguinal hernia repair to robotic transabdominal preperitoneal inguinal hernia repair: a retrospective review of a single surgeon’s experience. World J Surg. 2017;41:2251–7.
- Ye L, Childers CP, de Virgilio M. Clinical outcomes and cost of robotic ventral hernia repair: systematic review. BJS Open. 2021;5:zrab098.
- Haladu N, Alabi A, Brazzelli M, et al. Open versus laparoscopic repair of inguinal hernia: an overview of systematic reviews of randomised controlled trials. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9160137/). Surg Endosc. 2022;36(7):4685-4700.
- Solaini L, Cavaliere D, Avanzolini A, Rocco G, Ercolani G. Robotic versus laparoscopic inguinal hernia repair: an updated systematic review and meta-analysis. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9314304/. J Robot Surg. 2022;16(4):775-781.
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





