Introduction
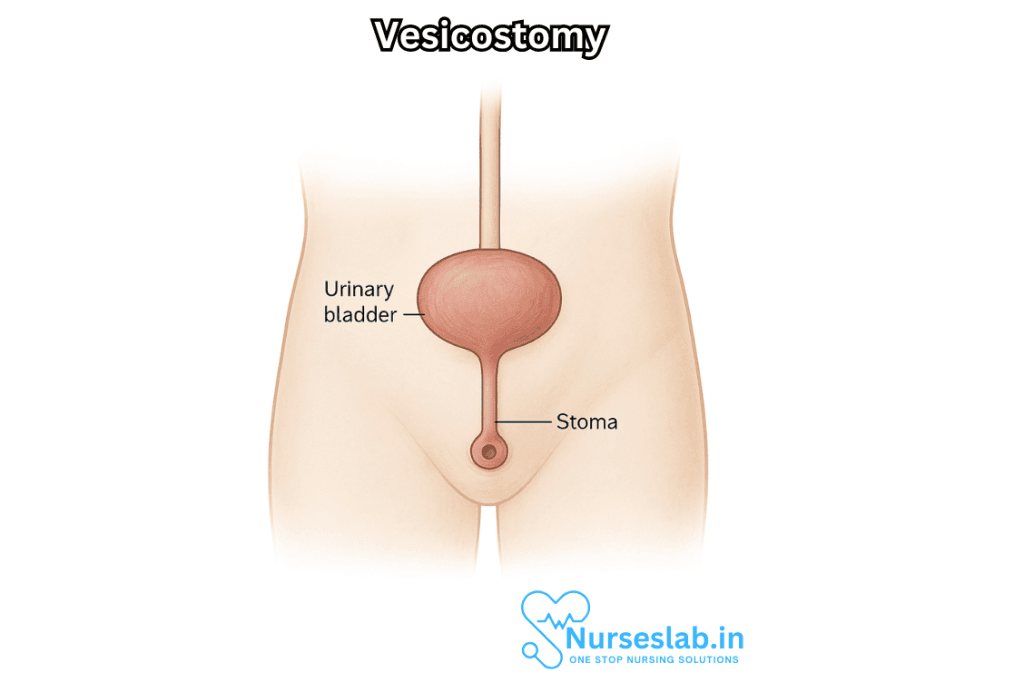
Vesicostomy is a surgical procedure that creates a direct opening from the bladder to the abdominal wall, allowing for urinary diversion and continuous drainage. Most commonly performed in pediatric populations, especially for children with congenital or acquired lower urinary tract dysfunction, vesicostomy remains an important intervention for specific urologic conditions. Although less common in adults, the procedure can be life-changing or even life-saving in select cases. This document provides a comprehensive overview of vesicostomy, covering indications, surgical techniques, postoperative care, complications, and long-term outcomes.
Indications for Vesicostomy
Vesicostomy is primarily indicated in situations where there is a need for low-pressure bladder drainage due to obstruction, poor bladder emptying, or risk of upper urinary tract damage. Common indications include:
- Posterior Urethral Valves (PUV): Congenital obstruction of the posterior urethra in male infants, leading to urinary retention and risk of renal damage.
- Neurogenic Bladder: Bladder dysfunction due to neurological disorders such as spina bifida, spinal cord injury, or myelomeningocele.
- Bladder Outlet Obstruction: Conditions that cause blockage of urine flow, not amenable to less invasive management.
- Recurrent Urinary Tract Infections (UTIs): Particularly in children with incomplete bladder emptying, vesicostomy may reduce infection risk.
- Unmanageable Incontinence: In rare cases, as a temporary measure for severe incontinence not responsive to conservative therapy.
- Failed Conservative Management: When catheterization, medications, or other treatments fail to protect the upper urinary tract.
Pathophysiology and Rationale
Vesicostomy diverts urine away from the urethra, thereby reducing intravesical (bladder) pressure. By providing a low-pressure outlet, the risk of backflow into the kidneys (vesicoureteral reflux), urinary tract infections, and progressive renal damage is reduced. In children with incomplete bladder emptying or severe obstruction, vesicostomy can preserve renal function while allowing the bladder and urinary tract to grow and develop.
Preoperative Evaluation
Prior to vesicostomy, a thorough assessment is needed, including:
- Medical History and Physical Examination: Focusing on urological, neurological, and renal aspects.
- Imaging Studies: Renal and bladder ultrasound, voiding cystourethrogram (VCUG), and sometimes MRI to assess anatomy and function.
- Urodynamics: To evaluate bladder compliance, capacity, and detrusor pressures.
- Laboratory Tests: Renal function tests (creatinine, BUN), urinalysis, and urine culture.
Surgical Technique
The most common form of vesicostomy is the Blocksom technique, though variations exist. The procedure is usually performed under general anesthesia.
General Steps:
- Incision: A small (usually 1.5-2.5 cm) transverse or vertical incision is made in the lower abdomen (infraumbilical or suprapubic region).
- Bladder Exposure: The bladder is brought up to the abdominal wall through the incision.
- Bladder Opening: The bladder dome is opened, and the edges are sutured to the skin, creating a stoma through which urine can drain freely.
- Securing the Stoma: The stoma is fashioned to prevent narrowing or closure, ensuring reliable drainage.
Postoperative Care:
- Wound Care: The stoma must be kept clean and dry, with regular monitoring for signs of infection or blockage.
- Diapering in Infants: For children, frequent diaper changes are necessary to keep the area clean and prevent skin irritation.
- Monitoring Output: Observation of urine flow and color; any reduction in output or changes in appearance should prompt medical evaluation.
- Education: Parents and caregivers are instructed in stoma care, signs of complications, and when to seek medical help.
Complications
While vesicostomy is generally safe, complications can occur. These include:
- Stomal Stenosis: Narrowing of the stoma, leading to impaired drainage and potential bladder distention.
- Urinary Tract Infections: Although vesicostomy can reduce infection rates, ascending infections may still occur.
- Stomal Prolapse: Protrusion of the bladder mucosa through the stoma, sometimes requiring revision.
- Skin Irritation: Prolonged exposure of skin to urine can cause dermatitis or breakdown.
- Bleeding or Infection: As with any surgical procedure, there is a risk of postoperative bleeding or wound infection.
- Bladder Calculi (Stones): Chronic stoma can lead to stone formation within the bladder.
Long-Term Management and Outcomes
Vesicostomy is often considered a temporary solution, especially in young children. As the child grows or as definitive management of the underlying condition becomes feasible, vesicostomy may be closed and alternative interventions pursued (such as clean intermittent catheterization or urethral reconstruction).
Follow-up and Monitoring
- Regular Clinic Visits: Patients require ongoing follow-up to monitor renal function, stoma patency, and urinary tract health.
- Renal Ultrasound: Periodic imaging to track kidney growth and identify complications.
- Urodynamics: May be repeated to assess bladder function after diversion or closure.
Quality of Life
A well-managed vesicostomy can significantly improve quality of life by reducing infections, preserving renal function, and allowing children to grow and thrive. However, stoma care can be demanding, and psychosocial support for patients and families is important.
Alternatives to Vesicostomy
While vesicostomy is effective in select cases, other urinary diversion strategies may be considered depending on age, anatomy, and overall health:
- Clean Intermittent Catheterization (CIC): Preferred in older children and adults who can cooperate and have suitable anatomy.
- Suprapubic Catheterization: Placement of a catheter directly into the bladder through the abdomen for continuous or intermittent drainage.
- Continent Diversion Procedures: Creation of a reservoir with controlled emptying, such as Mitrofanoff procedure.
- Definitive Surgery: Surgical correction of the underlying anatomical cause (e.g., valve ablation in PUV).
Vesicostomy in Adults
Although rare, vesicostomy may be performed in adults with complex lower urinary tract issues, most often as a last resort when other options are not feasible. Indications include severe neurogenic bladder with recurrent infections or incontinence, or in cases of urethral trauma or malignancy.
Historical Perspective
Vesicostomy has been performed since the early 20th century and has evolved with advances in pediatric urology, anesthesia, and surgical technique. While the number of vesicostomies performed has decreased with the advent of catheterization and improved techniques, the procedure remains of vital importance in certain scenarios.
Nursing Care for Patients with Vesicostomy
Nursing care for patients with vesicostomy requires a thorough understanding of the procedure, ongoing assessment, infection prevention, stoma care, and education for both the patient and family. This document provides a detailed framework for providing evidence-based, compassionate nursing care to patients living with vesicostomy.
Preoperative Nursing Considerations
- Educate the patient and family about the procedure, expected outcomes, and postoperative care requirements
- Assess baseline renal function, bladder capacity, and the presence of ongoing infections
- Ensure informed consent is obtained and documented
- Prepare the skin in the operative area, ensuring it is clean and free of infection
- Monitor emotional status and provide psychological support, especially for pediatric patients and their families
Postoperative Nursing Care
Postoperative care is critical in ensuring healing, preventing complications, and promoting patient comfort and adaptation. The following aspects outline comprehensive nursing responsibilities:
Assessment and Monitoring
- Monitor vital signs and observe for signs of postoperative complications, including bleeding, infection, or urinary leakage around the stoma
- Assess urine output for color, quantity, and clarity, noting any changes that may indicate infection or obstruction
- Inspect the stoma site for redness, swelling, discharge, or breakdown of surrounding skin
- Monitor pain levels and provide appropriate analgesia as prescribed
Stoma and Skin Care
Proper care of the stoma and surrounding skin is essential to prevent infection and skin breakdown.
- Gently cleanse the area around the stoma with warm water and mild soap, avoiding harsh chemicals or vigorous scrubbing
- Pat the area dry and apply a protective barrier cream if prescribed
- Inspect for any signs of moisture-associated skin damage, erythema, or ulceration
- Change dressings as needed, using sterile technique to prevent introduction of pathogens
- Monitor for granulation tissue, which may require intervention if excessive
Infection Prevention
Patients with vesicostomy are at increased risk of urinary tract infections due to the direct communication between the bladder and external environment.
- Practice strict hand hygiene before and after providing care
- Educate the patient and family on hand hygiene and stoma care
- Use sterile equipment during dressing changes and any procedures involving the stoma
- Monitor for fever, malaise, foul-smelling urine, or increased stoma drainage, and report findings promptly
Urine Collection and Management
- Collect urine in a clean, dry, appropriately sized container if continuous drainage is required
- Empty urine containers frequently to prevent overflow and accidental contamination
- Document urine output accurately, note changes in volume, and report abnormal findings
- Promote adequate fluid intake unless contraindicated to help flush the urinary tract and reduce infection risk
Pain Management
- Regularly assess pain using age-appropriate scales
- Administer prescribed analgesics and monitor for effectiveness
- Provide comfort measures such as positioning, distraction, and supportive conversation
Nutrition and Hydration
- Encourage a well-balanced diet to promote wound healing and overall health
- Monitor for dehydration, especially in the presence of increased urinary output
- Consult with dietitians for individualized nutrition plans as needed
Psychosocial Support
Living with a vesicostomy, especially in children, can be challenging and may impact self-esteem and social interactions.
- Provide emotional support to patients and families, addressing concerns about body image and adaptation
- Encourage participation in support groups or counseling services
- Provide age-appropriate education about vesicostomy and self-care
Patient and Family Education
Empowering patients and families with knowledge is a cornerstone of successful vesicostomy care.
- Educate on daily stoma care, signs of infection, and when to seek medical attention
- Provide written and verbal instructions for urine collection, skin protection, and equipment usage
- Teach techniques for safe dressing changes and disposal of medical waste
- Discuss the importance of regular follow-up with healthcare providers
- Explain activity limitations and precautions as advised by the surgical team
Managing Complications
While vesicostomy is generally safe, complications can occur and must be addressed promptly:
- Infection: Monitor closely for local or systemic signs; treat with antibiotics as prescribed
- Stomal stenosis: Watch for decreased urine flow or difficulty with drainage; surgical revision may be required
- Skin irritation or breakdown: Implement strategies for moisture control and skin protection
- Urinary leakage around stoma: Assess for proper stoma function and secure dressing fit
- Granulation tissue overgrowth: May require topical treatment or surgical excision
Long-Term Nursing Considerations
For patients with a long-term vesicostomy, ongoing support and care are essential:
- Encourage routine assessment and follow-up for renal function and bladder health
- Monitor for psychosocial challenges, especially during school-age years and adolescence
- Support reintegration into social, educational, and recreational activities
- Facilitate transition to self-care as appropriate for age and development
- Coordinate multidisciplinary care with physicians, stoma nurses, social workers, and therapists
Discharge Planning and Community Support
Effective discharge planning ensures that the patient and family feel confident in managing vesicostomy at home:
- Assess readiness for discharge based on mastery of self-care skills and understanding of complications
- Arrange for home nursing visits or telehealth check-ins as needed
- Provide contact information for healthcare providers and support resources
REFERENCES
- Rouzrokh M, Mirshemirani A, Khaleghnejad-Tabari A, Sadeghian N, Mohajerzadeh L, Mohkam M. Protective temporary vesicostomy for upper urinary tract problems in children: a five-year experience. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4025121/. Iran J Pediatr. 2013 Dec;23(6):648-52.
- Fischer KM, Bowen DK, Kovell RC, Canning DA, Weiss DA. Follow-up and outcomes of patients with long-term cutaneous vesicostomies at a single institution. Urology. 2020;144:255–60. https://doi.org/10.1016/j.urology.2020.04.130.
- Hofmann A, Haider M, Cox A, Vauth F, Rosch WH. Is vesicostomy still a contemporary method of managing posterior urethral valves? Children (Basel). 2022;9(2) https://doi.org/10.3390/children9020138.
- Masatoshi Kumagai, Masaaki Imamura, Vesicostomy: An alternative approach for complicated adult patients with urinary retention, Continence Reports, Volume 8,2023,100040,ISSN 2772-9745, https://www.sciencedirect.com/science/article/pii/S2772974523000200
- Salih EM, Abdrabuh AM, Okasha AH, Galal H. Temporary vesicostomy in pediatrics: What are the potential predictors of functional and morphological improvement of the upper urinary tract?. https://pubmed.ncbi.nlm.nih.gov/34602355/J Pediatr Urol. 2021 Dec;17(6):834.e1-834.e9
- Sharifiaghdas F, Mirzaei M, Nikravesh N. Can transient resting of the bladder with vesicostomy reduce the need for a major surgery in some patients? J Pediatr Urol. 2019;15(4):379 e1- e8. https://doi.org/10.1016/j.jpurol.2019.03.026.
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





