A Comprehensive Guide to Procedure, Indications, and Care
Introduction
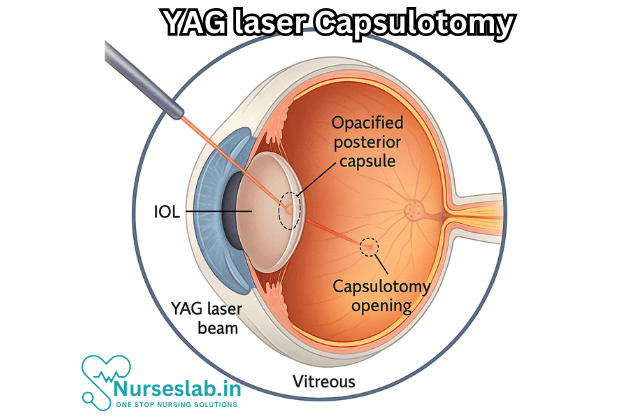
YAG Laser Capsulotomy is a widely performed ophthalmological procedure that addresses a common complication following cataract surgery: posterior capsule opacification (PCO), also known as a “secondary cataract.” This non-invasive laser treatment restores vision clarity that may become clouded months or years after successful cataract removal.
The Basis of the Procedure
Understanding Posterior Capsule Opacification (PCO)
Cataract surgery involves removing the eye’s natural cloudy lens and replacing it with an artificial intraocular lens (IOL). The lens is encased in a thin, clear membrane called the lens capsule. In most surgeries, a significant part of the anterior capsule is removed to facilitate lens replacement, but the posterior capsule is left intact to support the new lens. Over time, cells remaining in the capsule may proliferate and migrate to the posterior portion, forming a cloudy or wrinkled layer — this is posterior capsule opacification (PCO).
PCO can develop in up to 20-30% of patients within the first two to five years after cataract surgery, making it the most common long-term complication of the procedure.
What is YAG Laser Capsulotomy?
The YAG Laser Capsulotomy is a non-surgical, outpatient procedure that uses a neodymium-doped yttrium aluminum garnet (Nd:YAG) laser to create an opening in the clouded posterior capsule. This creates a clear visual axis, allowing light to pass unimpeded to the retina and restoring the patient’s vision.
Indications for YAG Laser Capsulotomy
The primary indication for YAG Laser Capsulotomy is the presence of visually significant PCO. Symptoms include:
- Gradual blurring or decrease in vision after cataract surgery
- Glare or halos, especially when driving at night
- Difficulty reading or seeing fine details
- Reduced contrast sensitivity
A comprehensive eye examination will reveal PCO when the ophthalmologist inspects the posterior capsule using slit-lamp biomicroscopy.
The YAG Laser Capsulotomy Procedure
Pre-procedure Preparation
- The patient undergoes a full eye examination to confirm the diagnosis and ensure the IOL is stable.
- Pupil dilation is performed with eye drops to improve access and visibility of the capsule.
- Intraocular pressure may be measured prior to the procedure.
- Topical anesthetic drops are applied to numb the eye and minimize discomfort.
Step-by-step Technique
- The patient is seated at a slit lamp, similar to a routine eye examination.
- A contact lens may be gently placed on the eye to help focus the laser and stabilize the eye.
- The ophthalmologist focuses the YAG laser on the posterior capsule, usually aiming for the central visual axis.
- Short, precise pulses of laser energy are delivered to create a small opening — often circular or cruciate — in the capsule.
- The procedure typically takes only a few minutes, and the laser energy does not damage the surrounding ocular structures or the IOL.
Immediate Aftercare
- The patient’s vision is checked immediately after the procedure.
- Eye pressure is measured to rule out any acute increase (spike in intraocular pressure, or IOP).
- Anti-inflammatory eye drops may be prescribed to reduce any mild irritation or inflammation.
- The patient is advised to avoid rubbing the eye and to report symptoms like sudden vision loss, pain, or flashes of light.
Benefits of YAG Laser Capsulotomy
- Restores clarity of vision quickly — most patients notice improvement within hours or days.
- Minimally invasive, non-surgical, and performed in an outpatient clinic setting.
- Does not require stitches, injections, or general anesthesia.
- Generally safe with a low risk of complications.
- Allows for a rapid return to daily activities.
Risks and Potential Complications
While YAG Laser Capsulotomy is considered very safe, as with any medical procedure, there are potential risks and complications. These include:
- Transient increase in intraocular pressure (IOP): In most cases, this resolves spontaneously or with medication.
- Retinal detachment: The risk is low (less than 1%), but it is slightly elevated after the procedure, particularly in high-risk individuals (such as those with high myopia).
- Cystoid macular edema: Swelling in the central retina may rarely occur and can be managed with medications.
- Pitting or displacement of the intraocular lens (IOL): Rarely, if the laser pulse is misdirected.
- Inflammation or infection (extremely rare).
- Floaters: Many patients notice new floaters after the procedure; these usually diminish over time.
Who Should Avoid YAG Laser Capsulotomy?
The procedure is generally safe for most people with PCO; however, some cases may warrant caution or postponement:
- Active intraocular infection or uncontrolled inflammation
- Unstable intraocular lens position
- Very young children (rare indication for PCO)
- Patients who do not have visually significant symptoms
Patient Experience and Recovery
Most patients experience mild discomfort, if any, during the procedure. Vision may be blurry or hazy for a few hours afterward due to dilation and debris from the laser pulses. Many report a rapid improvement in clarity and function, often returning to normal activities on the same or next day.
Patients may notice floaters, flashes, or minor irritation, but serious complications are rare. Follow-up appointments are scheduled within a week to ensure pressure stability and check the visual outcome.
Outcomes and Prognosis
YAG Laser Capsulotomy has an excellent track record for restoring vision impaired by PCO. Studies show high rates of patient satisfaction, with over 95% experiencing significant improvement in visual acuity. The benefits are generally permanent, as the capsule cannot become cloudy again; however, very rarely, residual lens epithelial cells may cause some opacification around the edge of the capsulotomy, which rarely needs further intervention.
Nursing Care of a Patient Undergoing YAG Laser Capsulotomy (Posterior Capsulotomy)
The YAG (yttrium-aluminum-garnet) laser is employed to create an opening in this clouded capsule, thereby restoring visual clarity. As with any ocular procedure, meticulous nursing care before, during, and after the intervention is essential for a successful outcome and patient satisfaction.
Preoperative Nursing Care
1. Patient Assessment and Education
- Medical History Review: Assess the patient’s ophthalmic and systemic history, with particular attention to past cataract surgery, allergies (especially to medications or topical anesthetics), and coexisting conditions such as diabetes or hypertension.
- Medication Assessment: Determine the current medication regimen. Note the use of anticoagulants, antiplatelet agents, and any ocular medications.
- Consent: Ensure that informed consent has been obtained after explaining the nature, benefits, risks, and alternatives of the YAG laser capsulotomy procedure in understandable language.
- Patient Education:
- Describe the procedure, emphasizing that it is quick, painless, and typically performed in an outpatient setting.
- Set realistic expectations regarding improvement in vision.
- Discuss potential complications, such as transient increase in intraocular pressure (IOP), retinal detachment, or inflammation.
- Advise patients to arrange for transportation home post-procedure, as vision may be temporarily blurred.
2. Physical Preparation
- Vital Signs: Record baseline vital signs, including blood pressure, pulse, and temperature.
- Ocular Assessment: Document visual acuity and conduct a thorough ocular examination as per the physician’s instructions.
- Eye Drops Administration: Instill prescribed mydriatic (pupil-dilating) and topical anesthetic drops prior to the procedure. Cycloplegics may be ordered as well.
- NPO Status: Generally, fasting is not required for this procedure, but follow institutional policies and specific physician instructions.
3. Psychological Support
- Provide reassurance to alleviate anxiety. Address any fears or misconceptions about the laser and the procedure itself.
- Ensure privacy and a calm environment in the waiting area.
Intraoperative Nursing Care
1. Procedural Support
- Patient Positioning: Assist the patient to sit comfortably at the YAG laser machine (slit lamp). Proper alignment and stabilization of the head are crucial for safety and precision.
- Eye Preparation: Confirm that the operative eye has been correctly identified and prepared. Ensure that prescribed eye drops have been administered.
- Monitoring: Observe for any signs of discomfort, restlessness, or adverse reactions during the procedure.
2. Equipment Management
- Instrument Readiness: Prepare and check all necessary equipment, including the YAG laser device, protective eyewear, and emergency supplies.
- Safety Protocols: Ensure all safety measures are in place—eye protection for staff and patient, warning signage for laser use, and adherence to institutional laser safety guidelines.
3. Assistance to Ophthalmologist
- Be ready to assist the ophthalmologist as needed, offering additional anesthetic drops or other supplies during the session.
- Document the laser settings, number of pulses, and any complications or unusual events during the procedure.
Postoperative Nursing Care
1. Immediate Post-Procedure Assessment
- Observation: Monitor for immediate complications such as pain, photophobia, sudden decrease in vision, or signs of intraocular pressure elevation.
- Vital Signs: Reassess and document vital signs if indicated, especially in patients with significant comorbidities.
- Visual Acuity: Conduct a brief vision check following the procedure, as per institutional protocol.
2. Medication Administration
- Instill prescribed anti-inflammatory drops (e.g., corticosteroids or NSAIDs) to reduce the risk of postoperative inflammation.
- Administer IOP-lowering medications if indicated, as a spike in intraocular pressure can occur within hours of the procedure.
3. Patient Education and Discharge Instructions
- Activity: Advise patients to avoid strenuous activities for at least 24 hours and to refrain from rubbing the eyes.
- Warning Signs: Educate on symptoms warranting immediate medical attention, including:
- Sudden loss of vision
- Severe eye pain
- Flashes of light or floaters (could indicate retinal detachment)
- Redness, swelling, or discharge from the eye
Follow-Up: Emphasize the importance of attending scheduled follow-up appointments for intraocular pressure measurement and assessment of visual recovery.
Medication Compliance: Stress adherence to prescribed eye drop regimens and review the correct technique for self-administration.
Visual Recovery: Explain that vision may be blurry for a few hours or days postoperatively, but most patients experience significant improvement shortly thereafter.
4. Documentation
- Record all assessments, medications administered, patient responses, teaching provided, and any complications encountered during the perioperative period.
Potential Complications and Nursing Management
- Increased Intraocular Pressure (IOP): Monitor for signs such as headache, nausea, or eye pain. Administer IOP-lowering medications as ordered and report persistent elevation to the ophthalmologist promptly.
- Retinal Detachment: Recognize and educate about signs (flashes, floaters, “curtain” over vision). Immediate referral is essential if suspected.
- Macular Edema: Watch for reports of persistent blurry vision, distortion, or central vision loss. Notify the ophthalmologist if these symptoms occur.
- Inflammation or Infection: Monitor for redness, pain, photophobia, or discharge. Administer anti-inflammatories as prescribed and reinforce hand hygiene.
- Hemorrhage: Although rare, be alert to sudden pain, decreased vision, or visible bleeding, and seek immediate medical attention if observed.
Special Considerations
- Pediatric and Non-Communicative Patients: Adjust communication techniques and enlist family support to ensure understanding and compliance.
- Patients with Comorbidities: Collaborate with other healthcare providers to optimize overall health and manage chronic conditions pre- and post-procedure.
- Psychosocial Support: Address anxieties, misconceptions, and emotional well-being throughout the care continuum.
REFERENCES
- American Academy of Ophthalmology EyeWiki. Posterior Capsule Opacification. https://eyewiki.aao.org/Posterior_Capsule_Opacification. Updated 7/9/2024.
- Karahan E, Er D, Kaynak S. An Overview of Nd:YAG Laser Capsulotomy. Med Hypothesis Discov Innov Ophthalmol. 2014 Summer;3(2):45-50. PMID: 25738159; PMCID: PMC4346677.
- Biffi E, Gulmiri A, Patel B. Advanced Ocular Procedures. In: Reilly J, Gaiser H, Young B, eds. Clinical Procedures for Ocular Examination. 5th ed. McGraw Hill; 2024.
- Chen O, Greenfield LR, Raikar DH, et al. A Reevaluation of the Complication Rates and Follow-up Protocol of Nd:YAG Laser Capsulotomy. Invest. Ophthalm Vis Sci. 2023 June;64(8):3318.
- Lighthizer N, Johnson S, Holthaus J, et al. Nd:YAG Laser Capsulotomy: Efficacy and Outcomes Performed by Optometrists. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10662619/. Optom Vis Sci. 2023 Oct;100(10):665-669.
- McHugh J, Pringle E. Lasers in Ophthalmology. In: Riordan-Eva P, Augsburger JJ, eds. Vaughan & Asbury’s General Ophthalmology. 19th ed. McGraw-Hill Education; 2017.
- Moshirfar M, Milner D, Patel BC. Cataract Surgery. https://www.ncbi.nlm.nih.gov/books/NBK559253/. 2023 Jul 18. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan.
- Sabbagh L. PCO: What’s Wrong With Doing a YAG? https://www.reviewofophthalmology.com/article/pco-whats-wrong-with-doing-a-yag Review of Ophthalmology. 2018 May:34-38.
- The Ophthalmic News and Education (ONE) Network® of the American Academy of Ophthalmology. Nd:YAG Laser Posterior Capsulotomy. https://www.aao.org/education/current-insight/ndyag-laser-posterior-capsulotomy-3. Published 11/4/2013.
- Ursell PG, Dhariwal M, O’Boyle D, Khan J, Venerus A. 5 year incidence of YAG capsulotomy and PCO after cataract surgery with single-piece monofocal intraocular lenses: a real-world evidence study of 20,763 eyes (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7182577/). Eye (Lond). 2020 May;34(5):960-968.
- Zhang AY, Kumar D, Tripathy K. Laser Principles in Ophthalmology (https://www.ncbi.nlm.nih.gov/books/NBK582153/). 2023 Aug 25. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan.
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





