Arrhythmia is a medical term used to describe an irregularity in the rate or rhythm of the heartbeat. It encompasses a wide range of heart rhythm disturbances, which can cause the heart to beat too fast, too slow, or with an inconsistent rhythm. In some cases, arrhythmias may be harmless and even go unnoticed. In other circumstances, they may signal a serious underlying condition and lead to complications such as stroke or heart failure.
What is Arrhythmia?
The heart’s role is to pump blood efficiently throughout the body, a function orchestrated by a precise sequence of electrical impulses. When these impulses are disrupted, the heart may fall out of sync, causing an arrhythmia. The term “arrhythmia” itself stems from Greek, where “a-” means “without” and “rhythmos” means “rhythm.”
In a typical adult at rest, the heart beats at a regular pace of 60-100 beats per minute. An arrhythmia occurs when these rhythms deviate from normal—becoming too rapid (tachycardia), too slow (bradycardia), or erratic.
Types of Arrhythmia
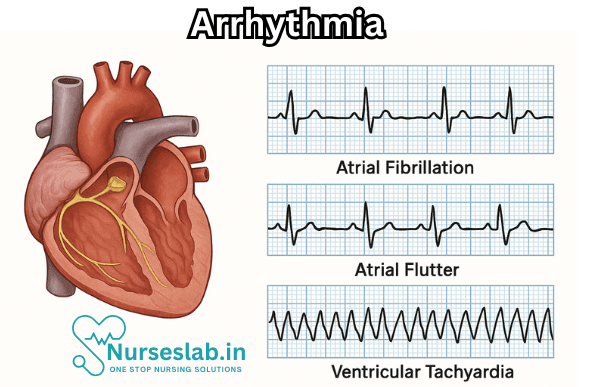
Arrhythmias can be classified in several ways, but most commonly by the speed of the heartbeat or the place of origin within the heart. The major types include:
1. Tachycardia (Fast Heartbeat)
When the heart beats faster than 100 beats per minute at rest, it is known as tachycardia. Tachycardias are further categorized by their origin in the heart:
- Supraventricular Tachycardia (SVT): Originates above the ventricles (the upper chambers of the heart). Includes atrial fibrillation, atrial flutter, and paroxysmal supraventricular tachycardia.
- Ventricular Tachycardia: Originates in the ventricles (the lower chambers). Can be life-threatening, especially if sustained.
2. Bradycardia (Slow Heartbeat)
A heart rate slower than 60 beats per minute is called bradycardia. While some slow heartbeats are benign (such as in athletes), others may signal electrical system dysfunction:
- Sick Sinus Syndrome: The heart’s natural pacemaker (the sinus node) does not function properly.
- Heart Block: Electrical signals are delayed or blocked as they travel through the heart.
3. Premature (Extra) Beats
These are early beats that disrupt the normal heart rhythm. They are usually benign and often described as feeling like a “skipped beat” or a “flutter.”
- Premature Atrial Contractions (PACs): Extra beats originating in the atria.
- Premature Ventricular Contractions (PVCs): Extra beats from the ventricles.
4. Fibrillation
This is a rapid and irregular beating of the heart muscle:
- Atrial Fibrillation (AFib): The atria quiver instead of beating effectively. AFib increases the risk of blood clots, stroke, and heart failure.
- Ventricular Fibrillation (VFib): The ventricles quiver and cannot pump blood effectively. VFib is a medical emergency requiring immediate intervention.
5. Flutter
Flutter involves a rapid but regular rhythm, typically in the atria (atrial flutter), and can sometimes progress to fibrillation.
Causes and Risk Factors
Arrhythmias arise from disruptions in the heart’s electrical system. Several factors can contribute to the development of arrhythmia:
- Coronary artery disease (blockages in the heart’s arteries)
- High blood pressure
- Heart failure or enlarged heart
- Valve disorders
- Congenital heart defects (present at birth)
- Electrolyte imbalances (such as potassium, sodium, calcium, or magnesium)
- Overuse of alcohol, caffeine, or recreational drugs
- Thyroid disorders (especially hyperthyroidism or hypothyroidism)
- Sleep apnea
- Certain medications or supplements
- Genetic predisposition or family history
Symptoms of Arrhythmia
Not all arrhythmias cause noticeable symptoms. When they do occur, they may include:
- Palpitations (a feeling of fluttering, pounding, or irregular heartbeat)
- Dizziness or lightheadedness
- Shortness of breath
- Chest pain or discomfort
- Fatigue or weakness
- Fainting (syncope) or near-fainting spells
- Anxiety
In severe cases, especially with ventricular arrhythmias, sudden cardiac arrest can occur.
Diagnosis of Arrhythmia
Diagnosing an arrhythmia typically begins with a detailed medical history and physical examination. The following tests and monitoring methods may be used:
- Electrocardiogram (ECG/EKG): Records electrical signals in the heart and is the most common diagnostic tool.
- Holter Monitor: A portable device worn for 24-48 hours to capture intermittent arrhythmias.
- Event Monitor: Similar to a Holter monitor but used for longer periods to record irregular events.
- Echocardiogram: Uses ultrasound waves to create images of the heart’s structure and function.
- Stress Test: Monitors the heart during exercise or medication-induced stress.
- Electrophysiological Study (EPS): Invasive test mapping the heart’s electrical activity to identify the source of arrhythmias.
- Blood tests to check for electrolyte imbalances, thyroid problems, or other underlying conditions.
Treatment Options
The treatment for arrhythmia depends on its type, severity, underlying cause, and the presence of symptoms. Approaches include:
- Lifestyle Changes: Reducing caffeine, alcohol, and avoiding stimulants; managing stress; eating a heart-healthy diet; and regular exercise.
- Medications: These may include antiarrhythmic drugs to control rhythm, beta-blockers, calcium channel blockers, anticoagulants (to reduce stroke risk in AFib), or medications to treat contributing conditions.
- Cardioversion: An electrical or chemical procedure to restore a normal heart rhythm, often used for AFib or atrial flutter.
- Catheter Ablation: Minimally invasive procedure that destroys the small area of heart tissue causing the arrhythmia.
Implantable Devices:
- Pacemaker: Used for bradycardia; this device sends electrical pulses to prompt the heart to beat at a normal rate.
- Implantable Cardioverter-Defibrillator (ICD): Monitors and corrects serious ventricular arrhythmias.
Surgery:
In rare cases, procedures such as the Maze procedure are undertaken to correct arrhythmias resistant to other treatments.
Living with Arrhythmia
A diagnosis of arrhythmia can be unsettling, but many people lead full and active lives with proper management. Regular follow-up with a healthcare provider is essential. It’s important to:
- Take prescribed medications as directed
- Monitor heart rate and symptoms
- Adopt healthy lifestyle habits
- Be alert for any new or worsening symptoms
- Carry identification indicating your heart condition and any implanted devices
Prevention Strategies
While not all arrhythmias can be prevented, some strategies reduce risk:
- Maintain a healthy weight and blood pressure
- Limit alcohol and caffeine consumption
- Avoid illicit drugs and over-the-counter stimulants
- Treat underlying health conditions, such as thyroid problems or sleep apnea
- Engage in regular physical activity
- Quit smoking
- Manage stress and get enough sleep
When to Seek Medical Help
Contact a healthcare provider if you experience:
- Unexplained fainting or near-fainting spells
- Persistent palpitations, chest pain, or shortness of breath
- Symptoms of heart failure (swelling, fatigue, sudden weight gain)
Call emergency services if someone collapses or is unresponsive, as this may signal cardiac arrest from a life-threatening arrhythmia.
Nursing Care of Patients with Arrhythmia
Nursing Interventions
Ensuring Patient Safety:
- Maintain a calm environment to reduce anxiety, which can exacerbate arrhythmias.
- Ensure bed rails are up for patients at risk of syncope or falls.
- Keep emergency equipment (defibrillator, oxygen supply) readily available at the bedside.
Medication Administration:
Administer antiarrhythmic drugs as prescribed, monitoring for efficacy and adverse effects.
Educate patients about the importance of medication adherence and potential side effects.
Oxygen Therapy:
Administer supplemental oxygen if required to optimise tissue oxygenation, especially in patients with hypoxaemia.
Fluid and Electrolyte Balance:
Monitor intake and output, and assess for signs of fluid overload or dehydration.
Check serum electrolyte levels (especially potassium and magnesium), as imbalances can precipitate arrhythmias.
Patient Education:
Teach patients and families about arrhythmia, risk factors, warning signs, and when to seek immediate medical attention.
Encourage lifestyle modifications such as smoking cessation, limiting caffeine and alcohol, and maintaining a healthy diet.
Psychological Support:
- Provide reassurance to alleviate fear and anxiety related to the condition.
- Involve family members in care and education to enhance support systems.
Emergency Management
- Be prepared to initiate cardiopulmonary resuscitation (CPR) and advanced cardiac life support (ACLS) protocols if the patient develops life-threatening arrhythmias.
- Assist with electrical cardioversion or defibrillation as required.
- Ensure prompt communication with the medical team for rapid intervention.
Discharge Planning and Follow-Up
- Provide clear instructions regarding medication, follow-up appointments, and lifestyle changes.
- Educate on recognising early signs of recurrence and the importance of adhering to prescribed therapy.
- Arrange for home care or community nursing support if needed, especially for patients with chronic or recurrent arrhythmias.
REFERENCES
- American Heart Association. Arrhythmia. https://www.heart.org/en/health-topics/arrhythmia. Accessed 3/20/2023.
- Akella K, et al. (2020). Impact of yoga on cardiac autonomic function and arrhythmias.
https://www.ncbi.nlm.nih.gov/labs/pmc/articles/PMC7533135/ - Desai DS, Hajouli S. Arrhythmias. https://www.ncbi.nlm.nih.gov/books/NBK558923/. [Updated 2022 Jun 11]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-.
- Heart and Stroke Foundation of Canada. Arrhythmi. https://www.heartandstroke.ca/heart-disease/conditions/arrhythmia.
- Cohagan B, et al. (2021). Torsade de Pointes.
https://www.ncbi.nlm.nih.gov/books/NBK459388/ - Merck Manual Consumer Version. Overview of Abnormal Heart Rhythms. https://www.merckmanuals.com/home/heart-and-blood-vessel-disorders/abnormal-heart-rhythms/overview-of-abnormal-heart-rhythms.
- Al-Khatib SM, Stevenson WG, Ackerman MJ, et al. 2017 AHA/ACC/HRS guideline for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death. Circulation. 2018;138(13). doi:10.1161/CIR.0000000000000549
- National Heart, Lung, and Blood Institute. What Is An Arrhythmia?. https://www.nhlbi.nih.gov/health/arrhythmias Accessed 3/20/2023.
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





