A comprehensive overview of intrauterine adhesions and their impact on women’s health
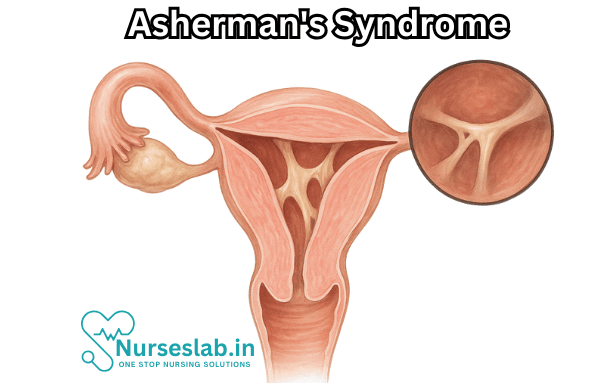
Asherman’s Syndrome, also known as Intrauterine Synechiae or Intrauterine Adhesions, is a rare but significant gynecological condition characterized by scar tissue formation within the uterine cavity. This can lead to a variety of menstrual abnormalities, fertility issues, and complications with pregnancy. First described by the German gynecologist Joseph G. Asherman in 1948, the syndrome has since been recognized as an important cause of secondary amenorrhea and infertility in women.
What is Asherman’s Syndrome?
Asherman’s Syndrome is defined by the presence of adhesions—bands of fibrous scar tissue—that partially or completely obliterate the uterine cavity and/or the cervical canal. These adhesions may range from thin, filmy bands to dense, thick scars that can bind the walls of the uterus together. In severe cases, the cavity may be almost entirely occluded.
Causes and Risk Factors
The most common cause of Asherman’s Syndrome is trauma to the endometrial lining of the uterus, typically following a surgical procedure. The main contributing factors include:
- Dilation and Curettage (D&C): This is the most frequent cause, particularly when performed after pregnancy-related events such as miscarriage, abortion, or postpartum hemorrhage. Aggressive or repeated D&Cs significantly increase the risk.
- Uterine Surgery: Procedures such as myomectomy (removal of fibroids), cesarean section, or removal of retained placenta can damage the uterine lining and lead to adhesion formation.
- Infections: Severe pelvic infections, especially those involving the endometrium (endometritis), can result in scarring.
- Radiation Therapy: Rarely, pelvic irradiation for cancer treatment may cause damage to the uterine lining.
- Genetic or Congenital Factors: While uncommon, some women may have a predisposition to abnormal wound healing, increasing the likelihood of adhesions.
Women who undergo multiple uterine procedures, particularly in a short span of time, are at higher risk for developing adhesions. The severity of Asherman’s Syndrome is often related to the extent of endometrial trauma and the subsequent healing response.
Symptoms of Asherman’s Syndrome
The symptoms can vary widely depending on the extent and location of the adhesions. Some women may be asymptomatic, while others may experience:
- Menstrual abnormalities: This is the most common symptom. It may manifest as hypomenorrhea (light periods), amenorrhea (absence of periods), or infrequent menstruation (oligomenorrhea).
- Infertility: Many women with Asherman’s Syndrome have difficulty conceiving, as adhesions can prevent implantation or embryo development.
- Recurrent pregnancy loss: Adhesions can compromise the uterine environment, leading to miscarriages.
- Pelvic pain: Some women report cramping or pain, particularly if menstrual blood is unable to exit the uterus due to blockage (hematometra).
- Abnormal placentation: In rare cases, women may experience complications such as placenta accreta in subsequent pregnancies due to scarring.
It is important to note that not all women with uterine adhesions will experience all of these symptoms, and the condition may go undiagnosed until an evaluation for infertility or recurrent miscarriage is performed.
Diagnosis
Diagnosing Asherman’s Syndrome can be challenging and often requires a combination of clinical suspicion and imaging. The following approaches are commonly used:
- Patient History: A detailed history focusing on previous uterine procedures, infections, or trauma is essential.
- Transvaginal Ultrasound: This may reveal an irregular or narrowed endometrial cavity, although it is not always definitive.
- Hysterosalpingography (HSG): A special X-ray using contrast dye to outline the uterine cavity, highlighting areas of blockage or irregularity.
- Sonohysterography: Saline infusion through the cervix followed by ultrasound can help visualize intrauterine adhesions.
- Hysteroscopy: Considered the gold standard for diagnosis, this involves direct visualization of the uterine cavity with a small camera. It allows for both diagnosis and treatment in the same procedure.
Blood tests and other laboratory investigations are generally unhelpful unless there is suspicion of infection or other underlying pathology.
Classification of Asherman’s Syndrome
Several classification systems have been developed, but the most widely accepted ones categorize the syndrome based on the extent and density of adhesions, as well as the menstrual pattern. The American Fertility Society (AFS) classification is commonly used, grouping cases as mild, moderate, or severe.
Treatment Options
The primary goal of treatment is to restore the normal anatomy and function of the uterine cavity, thereby improving menstrual flow and fertility prospects. Management typically includes:
- Hysteroscopic Adhesiolysis: This minimally invasive procedure is the treatment of choice. Under direct visualization, a surgeon uses fine instruments to cut and remove adhesions.
- Postoperative Hormonal Therapy: Estrogen therapy is often prescribed to stimulate regrowth of the endometrial lining and prevent reformation of adhesions.
- Mechanical Barriers: After surgery, devices such as balloon catheters or intrauterine devices (IUDs) may be placed temporarily to keep the uterine walls apart during healing.
- Antibiotics: Prescribed if infection is suspected or as a preventive measure after surgical intervention.
In severe cases where the uterine lining is extensively damaged, restoring normal function may be challenging, and alternative options for childbearing, such as surrogacy or adoption, may need to be considered.
Prognosis and Long-Term Outcomes
The prognosis depends on the severity of adhesions and the success of surgical treatment. Many women with mild to moderate Asherman’s Syndrome experience restoration of menstrual cycles and improved fertility after treatment. However, recurrence of adhesions is possible, particularly if the underlying cause persists or if extensive scarring was present.
Pregnancies following successful treatment tend to have higher risks, including abnormal placentation, preterm labor, or low birth weight. Close monitoring by a specialist is essential during any subsequent pregnancy.
Prevention
- Preventing Asherman’s Syndrome primarily involves:
- Prompt treatment of uterine infections and careful monitoring after postpartum or post-abortal procedures in at-risk individuals.
- Minimizing unnecessary uterine procedures, particularly D&Cs, and opting for medical management of miscarriages or retained products of conception when feasible.
- Adopting gentle surgical techniques and using smaller instruments during uterine surgery
Nursing Care of Patients with Asherman’s Syndrome
1. Assessment and Diagnosis
- Comprehensive History Taking: Obtain detailed medical, surgical, and menstrual history, focusing on previous uterine procedures, infections, and reproductive history.
- Symptom Assessment: Monitor for key symptoms such as amenorrhea (absence of menstruation), hypomenorrhea (scanty periods), infertility, and cyclical pelvic pain.
- Physical and Emotional Evaluation: Assess for signs of psychological distress, anxiety, or depression related to reproductive health concerns.
2. Preoperative Nursing Care
- Patient Education: Explain the diagnosis, potential procedures (such as hysteroscopic adhesiolysis), and expected outcomes in simple language. Use visual aids when possible.
- Consent and Preparation: Ensure informed consent is obtained. Prepare the patient physically and emotionally for any planned interventions.
- Baseline Investigations: Assist with preoperative investigations like blood tests, ultrasound, or hysteroscopy as prescribed.
3. Postoperative Nursing Care
- Monitoring: Observe vital signs, bleeding, and signs of infection. Monitor for pain and provide appropriate analgesia as prescribed.
- Infection Prevention: Maintain strict aseptic technique during all procedures. Educate the patient on signs of infection and the importance of personal hygiene.
- Medication Administration: Administer prescribed medications such as antibiotics, hormonal therapy (oestrogen to promote endometrial healing), and analgesics.
- Catheter Care: If a Foley’s catheter or intrauterine device is placed to prevent re-adhesion, educate the patient on its purpose and care requirements.
4. Psychological and Emotional Support
- Counselling: Provide a supportive environment for patients to express their fears and concerns, particularly regarding fertility and psychological distress.
- Family Involvement: Involve family members in counselling and education sessions as per the patient’s preference.
- Referral: Refer to mental health professionals or support groups if significant emotional or psychological issues are identified.
5. Patient Education and Discharge Planning
- Self-Care Instructions: Teach the patient about personal hygiene, recognising signs of infection, wound care (if applicable), and medication adherence.
- Follow-Up: Emphasise the importance of scheduled follow-up visits for monitoring recovery, assessing uterine healing, and early detection of complications.
- Fertility Counselling: Discuss future fertility prospects, available reproductive technologies, and the potential need for assisted reproductive techniques if indicated.
6. Complication Management
- Early Detection: Educate the patient to report symptoms such as fever, severe pain, heavy bleeding, or foul-smelling discharge immediately.
- Prompt Intervention: Collaborate with the healthcare team for timely management of complications like infection, recurrent adhesions, or haemorrhage.
REFERENCES
- National Organization for Rare Disorders. Asherman’s Syndrome. https://rarediseases.org/rare-diseases/ashermans-syndrome/#:~:text=Asherman’s%20syndrome%20is%20an%20uncommon,%2C%20in%20many%20instances%2C%20infertility.
- MyoClinic, Asherman syndrome: A rare collection of symptoms that can profoundly affect patients, Nov. 12, 2024, https://www.mayoclinic.org/medical-professionals/obstetrics-gynecology/news/asherman-syndrome-a-rare-collection-of-symptoms-that-can-profoundly-affect-patients/mac-20575535
- Smikle C, Yarrarapu SNS, Khetarpal S. Asherman Syndrome. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-.
- Ruvalcaba, Aranza & Pineda Melendres, Miriam & Gutierrez, Fitzgerald & Alba, Saulo & Flores, Carlos. (2023). Asherman’s Syndrome: A Comprehensive Review of Pathophysiology, Diagnosis, and Treatment Strategies. INTERNATIONAL JOURNAL OF MEDICAL SCIENCE AND CLINICAL RESEARCH STUDIES. 03. 10.47191/ijmscrs/v3-i10-27.
- Anderson-Bagga FM, Sze A. Placenta Previa. [Updated 2023 Jun 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/sites/books/NBK539818/
- Dreisler E, Kjer J. Asherman’s syndrome: current perspectives on diagnosis and management. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6430995/. Int J Womens Health. 2019; 11: 191-198.
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





