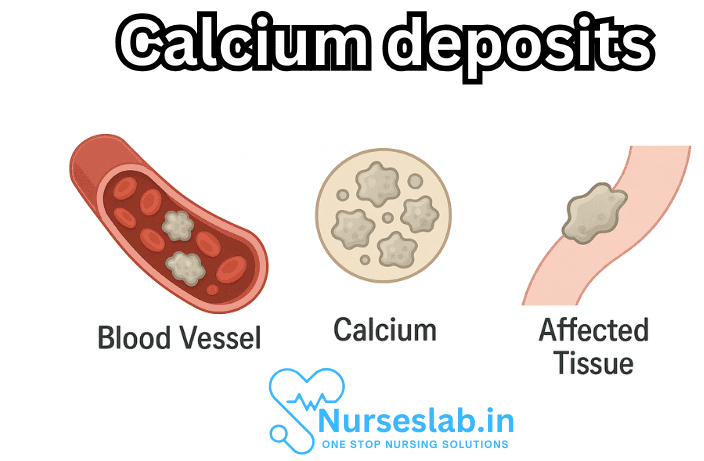
Calcium deposits, medically referred to as calcifications, are accumulations of calcium salts in body tissues. The formation of these deposits is often a complex process and can occur in various organs and tissues, leading to a wide array of health implications. While some calcium deposits are harmless, others may indicate underlying medical conditions or cause symptoms that require intervention.
What are Calcium Deposits?
Calcium deposits are hard accumulations formed when calcium—a mineral essential for healthy bones, teeth, and physiological functions—settles in soft tissues where it does not belong. Under normal circumstances, calcium is vital for muscle contraction, nerve transmission, and blood clotting. However, when excess calcium salts precipitate out of the blood and accumulate in organs or tissues, they can interfere with function and generate concerns.
There are several types of calcification, each with unique causes and consequences:
- Dystrophic Calcification: Occurs in damaged or necrotic tissues, even when blood calcium levels are normal.
- Metastatic Calcification: Results from elevated blood calcium levels, often due to metabolic disturbances, leading to deposits in otherwise healthy tissues.
- Idiopathic Calcification: Appears without a clear cause, sometimes in localized regions such as joints or tendons.
Common Sites for Calcium Deposits
Calcium deposits can form in virtually any tissue or organ. Some of the most frequently affected sites include:
- Joints and Tendons: Known as calcific tendinitis, it commonly affects the shoulders, elbows, knees, and hips.
- Skin and Subcutaneous Tissue: This presents as hard lumps under the skin, called calcinosis cutis.
- Arteries: Calcification of arterial walls (arteriosclerosis) can contribute to cardiovascular disease.
- Breasts: Detected via mammography, breast calcifications are often benign but may sometimes indicate malignancy.
- Kidneys: Renal calcifications can form stones or indicate chronic kidney disease.
- Lungs: Pulmonary calcifications may signal previous infections or chronic inflammation.
- Brain: Intracranial calcifications can be associated with infections, tumors, or metabolic conditions.
Causes of Calcium Deposits
The mechanisms leading to calcium deposits are diverse and sometimes multifactorial. The most common causes are:
1. Injury and Tissue Damage
Damaged tissues release substances that attract calcium ions, leading to local deposition. Examples include muscle tears, chronic tendon overuse, or trauma.
2. Inflammation and Infection
Chronic inflammation, as seen in autoimmune diseases like lupus or rheumatoid arthritis, can cause dystrophic calcification. Some infections (e.g., tuberculosis) leave behind calcified lesions as the body walls off the infection.
3. Metabolic Imbalances
Conditions that alter calcium or phosphate metabolism—such as hyperparathyroidism, chronic kidney disease, or excessive vitamin D intake—can raise blood calcium levels and promote metastatic calcification.
4. Genetic Conditions
Rare genetic diseases, such as pseudoxanthoma elasticum or familial tumoral calcinosis, disrupt normal calcium regulation, leading to abnormal deposits.
5. Aging
With age, tissues may degenerate and calcify, especially in the arteries, heart valves, and joints.
6. Medication and Environmental Factors
Certain drugs (e.g., corticosteroids) and exposures (e.g., silica) can increase the risk of calcification.
Symptoms of Calcium Deposits
The clinical presentation of calcium deposits depends on their location, size, and underlying cause. Some individuals remain asymptomatic, while others experience discomfort or impaired function.
| Location | Common Symptoms |
| Joints/Tendons | Pain, swelling, reduced mobility, stiffness |
| Arteries | High blood pressure, chest pain, risk of heart attack/stroke |
| Skin | Hard lumps, skin ulceration, inflammation |
| Kidneys | Flank pain, hematuria, urinary tract infections |
| Breasts | Usually asymptomatic, sometimes palpable lumps |
| Lungs | Chronic cough, shortness of breath (if extensive) |
| Brain | Neurological symptoms (rare), seizures, headaches |
Diagnosis of Calcium Deposits
Diagnostic procedures include:
- Physical Examination: Palpation of lumps or assessment of joint pain and movement.
- Imaging Studies: X-rays, ultrasounds, CT scans, and MRIs are highly effective at visualizing calcifications.
- Blood Tests: Analysis of calcium, phosphate, vitamin D, and parathyroid hormone levels helps determine metabolic causes.
- Biopsy: In cases of suspected malignancy or unclear origin, tissue samples may be taken for microscopic examination.
Treatment of Calcium Deposits
Therapy is tailored to the cause, location, and severity of the calcification. In many cases, no treatment is required if the deposits are asymptomatic and benign. For symptomatic or problematic cases, treatment options include:
Conservative Management
- Rest and Physical Therapy: Especially effective for tendon and joint calcifications.
- Anti-inflammatory Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs) can reduce pain and swelling.
- Dietary Adjustments: Regulating calcium and vitamin D intake may be necessary in cases caused by excessive supplementation.
Medical Interventions
- Extracorporeal Shockwave Therapy (ESWT): Uses sound waves to break up deposits in tendons and soft tissue.
- Chelation Therapy: Rarely used, can help dissolve deposits in some cases.
- Corticosteroid Injections: Reduce inflammation in affected tissues.
Surgical Management
- Minimally Invasive Procedures: Needle aspiration or arthroscopy can remove deposits from joints or soft tissue.
- Open Surgery: Reserved for large, painful, or functionally impairing deposits.
Prevention of Calcium Deposits
Preventive strategies depend on the underlying cause:
- Adequate Hydration: Helps prevent kidney stones and some other types of calcification.
- Balanced Diet: Maintain appropriate intake of calcium, phosphate, and vitamin D.
- Regular Physical Activity: Supports joint health and prevents injury.
- Monitoring Blood Calcium Levels: Particularly important for individuals with metabolic or endocrine disorders.
- Treating Underlying Conditions: Effective management of autoimmune, inflammatory, or metabolic diseases lowers risk.
Nursing Care of Patients with Calcium Deposits
As a nurse, providing optimal care to patients with calcium deposits requires a thorough understanding of the underlying causes, potential complications, and tailored nursing interventions. This document offers an in-depth exploration of the nursing care for patients experiencing calcium deposits, encompassing assessment, planning, implementation, and education.
Comprehensive Nursing Assessment
History and Physical Examination
- Gather a detailed medical, surgical, and medication history, focusing on risk factors such as chronic kidney disease, endocrine disorders, autoimmune conditions, or previous trauma.
- Assess for symptoms such as pain, swelling, decreased mobility, skin changes, or presence of palpable lumps.
- Evaluate patient’s nutritional intake, especially calcium and vitamin D consumption.
- Review laboratory data: serum calcium, phosphorus, parathyroid hormone (PTH), vitamin D, renal function tests.
Inspection and Palpation
- Inspect affected areas for signs of inflammation (redness, warmth, swelling).
- Palpate for masses, tenderness, or firmness in soft tissues.
- Assess joint range of motion and functional limitations.
- Monitor for signs of complications such as ulceration, infection, or nerve impingement.
Diagnostic Investigations
- Imaging: X-rays, CT scans, or MRIs to localize and characterize deposits.
- Biopsy (if indicated): To rule out malignancy or confirm diagnosis.
Nursing Diagnoses
Based on assessment findings, possible nursing diagnoses may include:
- Acute or chronic pain related to tissue inflammation or pressure from deposits.
- Impaired physical mobility related to joint or soft tissue involvement.
- Risk for impaired skin integrity due to ulceration or infection over deposits.
- Disturbed body image related to visible lumps or deformity.
- Deficient knowledge regarding condition and care requirements.
Nursing Planning and Goal Setting
The goals of nursing care for patients with calcium deposits are to:
- Manage and minimize pain and discomfort.
- Prevent complications such as skin breakdown and infection.
- Promote optimal mobility and functionality.
- Educate the patient and family about the condition and its management.
- Support psychological well-being and coping mechanisms.
Implementation: Nursing Interventions
Pain Management
- Administer analgesics as prescribed (e.g., acetaminophen, NSAIDs, or stronger medications if necessary).
- Apply local heat or cold packs, as appropriate, to reduce discomfort and inflammation.
- Encourage gentle range-of-motion exercises within tolerance to prevent stiffness.
- Offer relaxation techniques or distraction strategies to help the patient cope with persistent pain.
Skin and Wound Care
- Inspect skin overlying calcium deposits daily for signs of pressure injury, ulceration, or infection (redness, exudate, foul odor).
- Keep the skin clean and dry; use protective dressings if needed to minimize friction or pressure.
- Collaborate with wound care specialists for advanced ulcers or non-healing wounds.
- Monitor for systemic signs of infection such as fever, malaise, or increased white blood cell count.
Mobility Support
- Encourage movement and activity as tolerated; provide assistive devices (e.g., canes, walkers) to maximize independence.
- Refer to physical or occupational therapy for tailored exercise regimens and adaptive strategies.
- Educate on joint protection techniques to prevent further injury.
- Position the patient comfortably, using pillows or supports to relieve pressure on affected areas.
Monitoring and Prevention of Complications
- Regularly assess for changes in the size, consistency, or number of calcium deposits.
- Monitor laboratory values (serum calcium, phosphate, renal function) as indicated.
- Report sudden increases in pain, new neurological symptoms, or other concerning changes to the healthcare provider promptly.
- Ensure appropriate management of underlying conditions such as renal failure or hyperparathyroidism.
Patient and Family Education
Empowering patients and families with knowledge is a cornerstone of nursing care:
- Explain the nature and potential causes of calcium deposits, emphasizing the importance of adherence to prescribed therapies and follow-up appointments.
- Instruct on signs and symptoms that require immediate medical attention (e.g., severe pain, signs of infection, loss of function).
- Discuss dietary modifications, particularly if hypercalcemia or renal disease is present—this may include restricting calcium or phosphate intake as directed by a nutritionist.
- Provide information on medication regimens, including possible side effects and the importance of not missing doses.
- Address psychosocial concerns: Visible lumps or movement limitations can impact self-esteem; offer support and counseling referrals if needed.
Collaborative Care and Referrals
Management of patients with calcium deposits is best achieved through multidisciplinary collaboration:
- Work closely with physicians, dietitians, physical and occupational therapists, social workers, and wound care specialists.
- Facilitate referrals for specialist evaluation, such as endocrinology, rheumatology, or nephrology, depending on underlying etiology.
- Coordinate care transitions, ensuring the patient receives comprehensive support at home or in community settings.
Special Considerations
Chronic Kidney Disease
Patients with chronic kidney disease are at increased risk for metastatic calcification due to imbalances in calcium and phosphate metabolism. Nurses should:
- Monitor for vascular and soft tissue calcifications.
- Educate patients on the importance of phosphate binders and dietary restrictions.
- Work with nephrologists to optimize dialysis and medical management.
Autoimmune Disorders
In conditions like scleroderma or dermatomyositis, calcinosis cutis is a common manifestation. Nursing care includes:
- Monitoring for painful skin nodules and ulcerations.
- Supporting wound care and pain management.
- Facilitating access to specialty care for immunosuppressive therapies when indicated.
Psychosocial and Emotional Support
Calcium deposits can have a significant psychological impact, causing anxiety, embarrassment, or depression due to visible changes and functional limitations. Nurses should:
- Provide emotional support and empathetic listening.
- Encourage participation in support groups or counseling services.
- Promote body positivity and coping strategies.
Evaluation and Documentation
Continuous evaluation and accurate documentation ensure quality care:
- Assess the effectiveness of interventions regularly (pain relief, skin integrity, mobility improvements).
- Document all assessments, interventions, patient responses, and education provided.
- Revise the care plan as needed based on patient progress and changing needs.
REFERENCES
- Breastcancer.org. Understanding Breast Calcifications. https://www.breastcancer.org/symptoms/testing/types/mammograms/mamm_show/calcifications.
- Jiang SW, Petty AJ, Nicholas MW. Innate immunity in calcinosis cutis. Immuno. 2022;2(3):443-59. doi:10.3390/immuno2030027
- Le C, Bedocs PM. Calcinosis Cutis. https://pubmed.ncbi.nlm.nih.gov/28846311/. In: StatPearls. Treasure Island (FL): StatPearls Publishing; July 17, 2021.
- Dube P, DeRiso A, Patel M, et al. Vascular calcification in chronic kidney disease: diversity in the vessel wall. Biomedicines. 2021;9(4):404. doi:10.3390/biomedicines9040404
- MedlinePlus. Calcification. https://medlineplus.gov/ency/article/002321.htm.
- Dickson FJ, Sayer JA. Nephrocalcinosis: a review of monogenic causes and insights they provide into this heterogeneous condition. Int J Mol Sci. 2020;21(1):369. doi:10.3390/ijms21010369
- Mohan J, Bhatti K, Tawney A, et al. Coronary Artery Calcification. https://www.ncbi.nlm.nih.gov/books/NBK519037/. [Updated 2021 Sep 24]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-.
- Chen Y, Zhao X, Wu H. Arterial stiffness: a focus on vascular calcification and its link to bone mineralization. Arterioscler Thromb Vasc Biol. 2020;40(5):1078-1093. doi:10.1161/ATVBAHA.120.313131
- National Organization for Rare Disorders. Primary Familial Brain Calcification. https://rarediseases.org/rare-diseases/primary-familial-brain-calcification/.
- Nowaczyk J, Zawistowski M, Fiedor P. Local, non-systemic, and minimally invasive therapies for calcinosis cutis: a systematic review. Arch Dermatol Res. 2022;314(6):515-525. doi:10.1007/s00403-021-02264-5
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





