Introduction
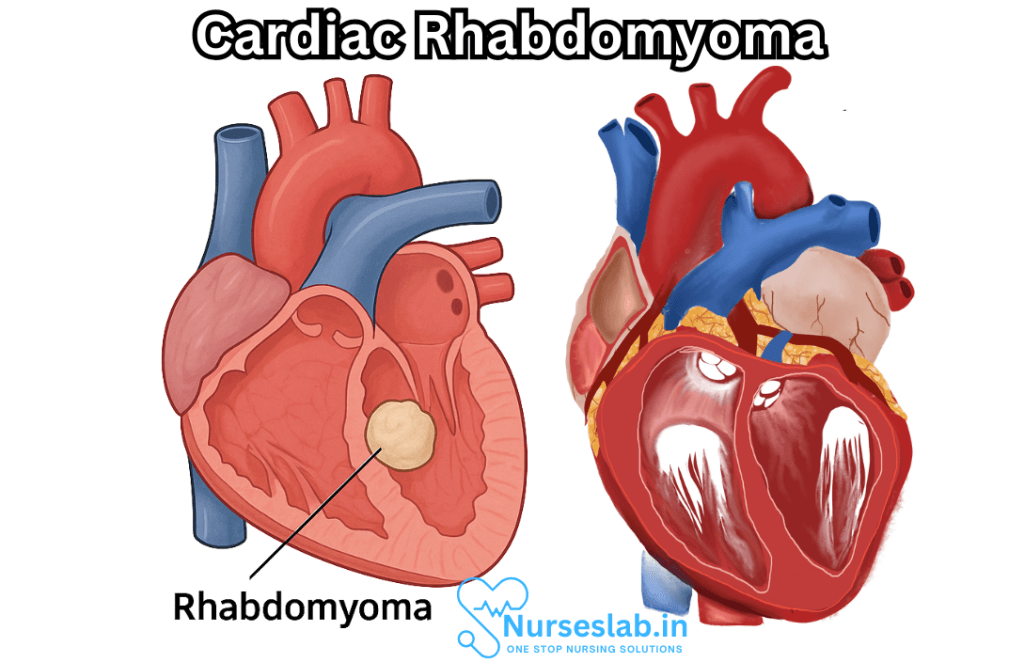
Cardiac rhabdomyoma is a benign tumor of the heart, most frequently encountered in infants and young children. It stands as the most prevalent primary cardiac tumor in the pediatric population, and although non-cancerous, its presence can have significant clinical implications depending on size, number, and location within the cardiac structure.
Epidemiology
Cardiac tumors in general are rare, with cardiac rhabdomyoma constituting the majority in the pediatric age group. Studies suggest an incidence rate ranging from 0.02% to 0.08% for primary cardiac tumors in children. Among these, rhabdomyomas account for approximately 45% of cases, followed by fibromas, teratomas, and myxomas. Most cases are diagnosed before the age of two, and a significant proportion are detected prenatally or in neonates owing to advances in fetal echocardiography.
Pathogenesis and Genetic Associations
Rhabdomyomas are hamartomatous growths arising from cardiac muscle cells, specifically myocytes. Unlike neoplasms that are proliferative and invasive, hamartomas such as rhabdomyomas represent disorganized overgrowths of normal tissue components. The pathogenesis of cardiac rhabdomyoma is closely tied to genetic mutations affecting cellular proliferation and differentiation.
Tuberous Sclerosis Complex (TSC)
The strongest association exists between cardiac rhabdomyoma and tuberous sclerosis complex, a multisystem genetic disorder caused by mutations in either the TSC1 or TSC2 genes, encoding hamartin and tuberin, respectively. These proteins act as tumor suppressors, regulating cell growth. When mutated, abnormal cell proliferation ensues, manifesting as hamartomas in various organs, including the brain, skin, kidneys, and heart.
It is estimated that up to 50-90% of children with cardiac rhabdomyoma have underlying tuberous sclerosis. Conversely, 40-60% of patients with tuberous sclerosis develop cardiac rhabdomyomas at some point in their lives. The identification of these tumors often prompts further investigation for TSC, especially in neonates.
Clinical Presentation
The clinical spectrum of cardiac rhabdomyoma is broad, ranging from asymptomatic cases to life-threatening cardiac compromise. The impact on cardiac function depends on the following factors:
- Size of the tumors: Larger lesions are more likely to impede blood flow or disrupt electrical conduction.
- Number: Multiple tumors often occur, especially in the setting of tuberous sclerosis.
- Location: Common sites include the ventricular walls, particularly the left ventricle, and the interventricular septum. Tumors in the outflow tracts or near valves carry greater clinical significance.
Symptoms
While many rhabdomyomas are discovered incidentally, possible symptoms include:
- Arrhythmias: Tumors involving the conduction system can precipitate various arrhythmias, notably ventricular tachycardia and Wolff-Parkinson-White syndrome.
- Obstructive symptoms: Lesions within the outflow tract or near valves may cause obstruction, resulting in cyanosis, congestive heart failure, or sudden collapse.
- Heart murmurs: Turbulent blood flow due to mass effect may generate a murmur detectable on auscultation.
- Heart failure: Severe cases may present with signs of heart failure, such as tachypnea, poor feeding, hepatomegaly, and peripheral edema.
- Sudden death: Rarely, large tumors or those interfering with cardiac conduction can cause sudden cardiac death.
Diagnosis
The diagnosis of cardiac rhabdomyoma involves a combination of clinical assessment and imaging modalities. The following approaches are commonly employed:
Echocardiography
Transthoracic echocardiography is the initial imaging technique of choice. Rhabdomyomas typically appear as homogeneous, well-demarcated, hyperechoic masses within the myocardium. The non-invasive nature and real-time visualization of cardiac function make echocardiography ideal for both diagnosis and follow-up.
Fetal Echocardiography
With the advent of prenatal ultrasound, many cases of cardiac rhabdomyoma are detected in utero, especially during the third trimester. The identification of a cardiac mass prenatally often raises suspicion for tuberous sclerosis, guiding further genetic evaluation.
Magnetic Resonance Imaging (MRI)
Cardiac MRI can provide detailed anatomical information and help distinguish rhabdomyomas from other cardiac masses. It is particularly useful when echocardiographic findings are inconclusive or when surgical planning is required.
Other Investigations
Electrocardiography (ECG) may reveal arrhythmias or conduction disturbances. In cases with suspected tuberous sclerosis, additional investigations such as brain MRI, renal ultrasound, and dermatological assessment are warranted.
Differential Diagnosis
Other cardiac tumors that may present similarly include:
- Cardiac fibroma: Typically larger, solitary, and located in the ventricular septum.
- Teratoma: Often found in the pericardial cavity and may contain cystic and solid components.
- Myxoma: More common in adults and usually located in the left atrium.
- Hemangioma: Vascular tumors, rare in children.
Distinguishing between these entities relies on imaging characteristics and, in rare cases, histological confirmation.
Management
The management of cardiac rhabdomyoma is largely dictated by the severity of symptoms and the risk to cardiac function.
Conservative Approach
Most rhabdomyomas regress spontaneously over time, especially during early childhood. This phenomenon is attributed to the natural maturation and involution of the cells involved. Asymptomatic patients are typically monitored with periodic echocardiography to assess tumor size and cardiac function. Intervention is reserved for those with significant obstruction, progressive heart failure, or refractory arrhythmias.
Medical Management
Arrhythmias may be managed with antiarrhythmic medications, and heart failure symptoms can be treated with standard pediatric heart failure protocols. In select cases, mTOR inhibitors (e.g., sirolimus or everolimus) have shown promise in reducing tumor size, particularly in patients with tuberous sclerosis complex.
Surgical Intervention
Surgery is rarely required but may be necessary in cases of life-threatening obstruction or refractory arrhythmias. Surgical excision carries risks, especially when tumors are located near vital cardiac structures.
Interventional Procedures
Catheter-based interventions may be considered for arrhythmias associated with accessory conduction pathways.
Prognosis
The overall prognosis for children with cardiac rhabdomyoma is favorable, particularly in cases without significant cardiac compromise. Spontaneous regression is common, and the majority of children experience resolution of symptoms as the tumors involute. Nevertheless, the presence of arrhythmias or severe heart failure may impact survival in rare cases.
Tuberous Sclerosis Complex Implications
Because rhabdomyomas are often the first manifestation of tuberous sclerosis, the diagnosis carries implications for long-term management of the multisystem disorder. Early diagnosis and multidisciplinary care are essential for optimal outcomes.
Nursing Care of Patients with Cardiac Rhabdomyoma
Due to its unique presentation and potential complications, the nursing care of patients with cardiac rhabdomyoma requires a thorough understanding of the disease process, vigilant monitoring, multidisciplinary collaboration, and compassionate family support.
Nursing Assessment
The cornerstone of effective nursing care is a comprehensive assessment, which includes:
- History Taking: Assess for family history of tuberous sclerosis, prenatal history, onset and progression of symptoms, and previous cardiac evaluations.
- Physical Examination:
- Vital signs: monitor for tachycardia, tachypnea, hypoxemia, or hypotension.
- Cardiac auscultation: detect murmurs, irregular rhythms, or gallops.
- Signs of heart failure: observe for edema, hepatomegaly, and respiratory distress.
- Skin examination: look for hypopigmented macules, facial angiofibromas, shagreen patches, or other signs of TSC.
Diagnostic Evaluation:
- Electrocardiogram (ECG): detect arrhythmias or conduction abnormalities.
- Echocardiography: assess size, number, and location of rhabdomyomas; evaluate cardiac function and blood flow.
- Imaging: Cardiac MRI or CT may be used for detailed anatomy.
- Genetic testing: for diagnosis of tuberous sclerosis complex.
Nursing Diagnosis
Based on the assessment, common nursing diagnoses may include:
- Ineffective tissue perfusion related to obstruction of cardiac blood flow.
- Decreased cardiac output related to arrhythmias or compromised contractility.
- Ineffective breathing pattern related to heart failure or pulmonary congestion.
- Risk for fluid volume overload related to impaired cardiac function.
- Anxiety or fear related to diagnosis and prognosis (patient and family).
- Knowledge deficit regarding disease process and management.
Nursing Interventions
1. Cardiorespiratory Monitoring and Support
- Continuous monitoring of vital signs: heart rate, respiratory rate, blood pressure, and oxygen saturation.
- Monitor for signs of cardiac decompensation: increased work of breathing, cyanosis, diaphoresis, poor perfusion.
- Supplemental oxygen as prescribed for hypoxemia.
- Prepare for emergency interventions if arrhythmias or sudden deterioration occur (e.g., advanced cardiac life support protocols).
- Ensure emergency medications and equipment are readily available.
2. Fluid and Nutrition Management
- Monitor intake and output closely to assess for fluid overload.
- Administer diuretics as prescribed to manage heart failure symptoms, and monitor electrolyte balance.
- Provide nutrition support: frequent small feeds may help infants with poor feeding due to cardiac compromise.
- Monitor weight daily for changes indicating fluid status or nutritional decline.
3. Medication Administration and Monitoring
- Administer antiarrhythmic medications as prescribed and observe for therapeutic and adverse effects.
- Administer medications to treat heart failure (e.g., digoxin, ACE inhibitors, diuretics) as per physician orders.
- Monitor laboratory values: electrolytes, renal function, and medication levels as indicated.
4. Family Support and Education
- Provide emotional support and counseling to the patient and family, acknowledging their fears and concerns.
- Educate on the nature of cardiac rhabdomyoma, its association with tuberous sclerosis, prognosis, and potential complications.
- Teach the family to recognize signs of cardiac distress or arrhythmias and when to seek immediate medical attention.
- Offer information about support groups and genetic counseling if appropriate.
5. Multidisciplinary Collaboration
- Collaborate with pediatric cardiologists, cardiac surgeons, geneticists, neurologists, and other relevant healthcare professionals.
- Coordinate care for associated conditions, especially if the patient has tuberous sclerosis (neurological assessment, dermatology, nephrology, etc.).
- Participate in case conferences and care planning meetings as necessary.
Special Considerations
Expectant Management:
- In many cases, cardiac rhabdomyomas regress spontaneously, particularly in infants. The focus may be on careful observation and supportive care rather than immediate surgical intervention.
Surgical Intervention:
- Reserved for cases with severe obstruction, intractable arrhythmias, or heart failure unresponsive to medical management.
- Nurses play a vital role in pre- and post-operative care, including preparation, monitoring for complications (bleeding, infection, arrhythmias), and facilitating recovery.
Long-term Follow-up:
- Regular cardiac evaluations (echocardiograms, ECGs) to monitor tumor size and cardiac function.
- Ongoing surveillance for complications related to cardiac or extracardiac manifestations of tuberous sclerosis.
- Developmental assessment and early intervention as needed.
Patient and Family Education
- Explain the usual course of cardiac rhabdomyoma, including the high likelihood of spontaneous regression in infants but the need for ongoing monitoring.
- Discuss signs and symptoms that should prompt urgent medical review: worsening breathlessness, cyanosis, syncope, or palpitations.
- Provide information on lifestyle modifications and safe activity levels according to the patient’s cardiac status.
- If associated with tuberous sclerosis, discuss the implications for other organ systems and the importance of comprehensive care.
Psychosocial Considerations
- Address anxiety, stress, and uncertainty in both patient and family through compassionate communication, reassurance, and facilitating access to counseling services if needed.
- Provide resources for peer support, such as support groups or connections with families experiencing similar challenges.
- Encourage participation in care and decision-making, empowering families to feel confident managing the patient’s condition.
Discharge Planning
- Ensure clear instructions for medication administration, monitoring of symptoms, and follow-up appointments.
- Arrange for home health nursing support if necessary.
- Provide emergency contacts and reinforce when to seek urgent help.
- Coordinate with community resources and specialty clinics for ongoing support.
REFERENCES
- American Academy of Family Physicians. Tuberous Sclerosis. https://familydoctor.org/condition/tuberous-sclerosis/?adfree=true.
- Fetal Imaging. https://accessmedicine-mhmedical-com.ccmain.ohionet.org/content.aspx?bookid=1918§ionid=185047433. In: Cunningham F, Leveno KJ, Bloom SL, Dashe JS, Hoffman BL, Casey BM, Spong CY. eds. Williams Obstetrics, 25e. McGraw Hill; 2018.
- Ekmekci E, Ozkan BO, Yildiz MS, Kocakaya B. Prenatal diagnosis of fetal cardiac rhabdomyoma associated with tuberous sclerosis: A case report. Case Rep Womens Health. 2018 Jun 20;19:e00070. doi: 10.1016/j.crwh.2018.e00070. PMID: 30094198; PMCID: PMC6071374.
- Merck Manual. Overview of Heart Tumors. https://www.merckmanuals.com/home/heart-and-blood-vessel-disorders/heart-tumors/overview-of-heart-tumors.
- Tamirat M, Ayalew B. Cardiac Rhabdomyoma: A Surrogate Diagnosis of Tuberous Sclerosis Complex in a Newborn Baby: Case Report from Tikur Anbessa University Hospital. Ethiop J Health Sci. 2020 Jul 1;30(4):639-642. doi: 10.4314/ejhs.v30i4.19. PMID: 33897224; PMCID: PMC8054458.
- Yıldırım S, Aypar E, Aydın B, Akyüz C, Aykan HH, Ertuğrul İ, Karagöz T, Alehan D. Cardiac rhabdomyomas: clinical progression, efficacy and safety of everolimus treatment. Turk J Pediatr. 2023;65(3):479-488. doi: 10.24953/turkjped.2022.922. PMID: 37395967.
- Reejhsinghani RS, Redberg RF. Cardiac tumors.. https://accessmedicine-mhmedical-com.ccmain.ohionet.org/content.aspx?bookid=2040§ionid=152997304. In: Crawford MH. eds. CURRENT Diagnosis & Treatment: Cardiology, 5e. McGraw Hill; 2017.
- Rosset C, Netto CBO, Ashton-Prolla P. TSC1 and TSC2 gene mutations and their implications for treatment in Tuberous Sclerosis Complex: A review. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5409767/. Genet Mol Biol. 2017 Jan-Mar;40(1):69-79.
- StatPearls. Cardiac Rhabdomyoma . https://www.statpearls.com/articlelibrary/viewarticle/70099.
- Sarkar S, Siddiqui WJ. Cardiac Rhabdomyoma. 2022 Nov 14. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan–. PMID: 32809444.
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





