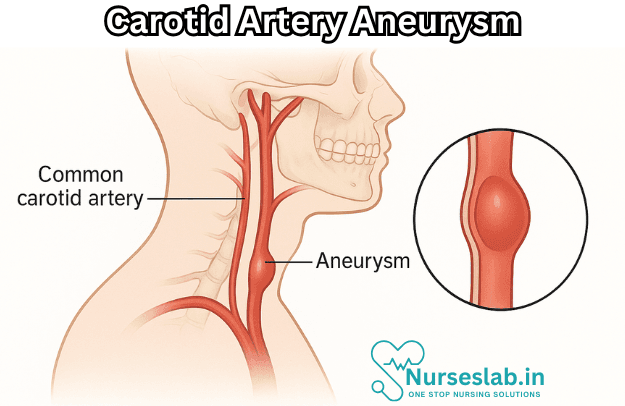
A carotid artery aneurysm is a bulge in one of the arteries supplying blood to your brain and nearby structures. Atherosclerosis is a common cause. Some people have no symptoms, but others have facial swelling, hoarseness or a throbbing lump they can feel in their neck. A carotid artery aneurysm may lead to a TIA (mini stroke) or stroke
Introduction
Carotid artery aneurysm disease represents a rare but clinically significant vascular pathology with potential for severe neurological complications. Defined by the abnormal dilatation of the carotid artery wall, this condition can lead to life-threatening events such as stroke, rupture, or thromboembolic phenomena. While aneurysms are more commonly associated with the aorta or intracranial vessels, carotid artery aneurysms warrant attention due to their proximity to the brain and potential for devastating consequences.
Pathophysiology of Carotid Artery Aneurysm
Aneurysms are defined as focal dilatations of a blood vessel wall exceeding 50% of the vessel’s normal diameter. In the context of the carotid artery, aneurysms are classified into three main types:
- True aneurysms: Involve all three arterial wall layers (intima, media, adventitia).
- False (pseudo) aneurysms: Result from a breach in the arterial wall, with blood contained by the surrounding tissues, forming a pulsatile haematoma.
- Dissecting aneurysms: Occur when blood enters the vessel wall through an intimal tear, creating a false lumen between the wall layers.
The underlying mechanisms involve structural weakening of the arterial wall due to degenerative, inflammatory, or traumatic processes. Aneurysm formation is often facilitated by chronic haemodynamic stress, enzymatic degradation of extracellular matrix components (e.g., elastin, collagen), and inflammatory cell infiltration. Genetic predispositions and acquired risk factors further modulate susceptibility.
Etiology and Risk Factors
Carotid artery aneurysms are uncommon, comprising less than 1% of all arterial aneurysms, but their aetiology is diverse. Key causes and risk factors include:
- Atherosclerosis: The most frequent cause, especially in older adults. Plaque formation weakens the arterial wall.
- Trauma: Blunt or penetrating neck injuries can disrupt the arterial wall, leading to pseudoaneurysm formation.
- Infection: Mycotic aneurysms arise from bacterial invasion (e.g., Staphylococcus aureus, Salmonella species), especially in immunocompromised individuals.
- Connective tissue disorders: Conditions like Ehlers-Danlos syndrome, Marfan syndrome, and fibromuscular dysplasia predispose to aneurysm due to inherent vessel wall weakness.
- Iatrogenic causes: Medical procedures involving the neck, such as carotid endarterectomy, catheterisation, or central line insertion, may inadvertently injure the vessel.
- Congenital defects: Rarely, developmental defects in the arterial wall structure may lead to aneurysm formation.
- Hypertension and smoking: Both contribute to arterial wall stress and degeneration.
Additional risk factors include advanced age, male gender, hyperlipidaemia, chronic inflammatory states (e.g., vasculitis), and a family history of aneurysms or vascular disease.
Clinical Presentation
The clinical manifestations of carotid artery aneurysms are highly variable, ranging from asymptomatic incidental findings to acute neurological emergencies. Common presentations include:
- Pulsatile neck mass: The most frequent sign, often accompanied by a bruit on auscultation.
- Cranial nerve palsies: Compression of adjacent nerves (e.g., hypoglossal, vagus, glossopharyngeal) may result in dysphagia, hoarseness, tongue deviation, or facial weakness.
- Ischaemic symptoms: Transient ischaemic attacks (TIAs), strokes, or amaurosis fugax due to embolisation of thrombotic material from the aneurysm.
- Pain: Localised neck pain or headache, sometimes radiating to the face or ear.
- Rupture: Rare but catastrophic, leading to rapidly expanding neck haematoma, airway compromise, or haemorrhagic shock.
- Other complications: Infection, fistula formation with adjacent structures (e.g., pharynx, trachea), or skin ulceration in advanced cases.
It is noteworthy that small aneurysms may remain clinically silent, detected incidentally during imaging for unrelated reasons.
Diagnostic Methods
Timely and accurate diagnosis is crucial for optimal management. The diagnostic approach typically includes:
- Physical examination: Inspection and palpation may reveal a pulsatile mass, while auscultation detects bruits.
- Duplex ultrasonography: A non-invasive, first-line imaging technique that assesses vessel anatomy, aneurysm size, flow characteristics, and thrombus presence.
- Computed Tomography Angiography (CTA): Provides high-resolution, three-dimensional images of vascular anatomy, aiding in preoperative planning. CTA is especially useful for visualising the aneurysm’s relationship to adjacent structures.
- Magnetic Resonance Angiography (MRA): Offers detailed vessel imaging without ionising radiation. MRA is valuable in patients with contrast allergies or renal impairment.
- Digital Subtraction Angiography (DSA): Considered the gold standard for vascular imaging, DSA allows precise assessment of aneurysm morphology and collateral circulation. It is, however, invasive and reserved for complex cases or endovascular planning.
In select cases, laboratory investigations (e.g., markers of infection, connective tissue disorder workup) may be warranted.
Treatment Options
The management of carotid artery aneurysm disease is highly individualised, considering factors such as aneurysm type, size, location, symptomatology, patient comorbidities, and risk of rupture or embolisation. Treatment modalities can be broadly categorised into medical management, surgical intervention, and endovascular techniques.
Medical Management
Medical therapy is generally reserved for asymptomatic, small, or surgically inoperable aneurysms. Key components include:
- Antiplatelet agents (e.g., aspirin) to reduce thromboembolic risk.
- Blood pressure control to minimise haemodynamic stress.
- Statins and lipid-lowering therapy to address atherosclerosis.
- Smoking cessation and lifestyle modification.
- Regular imaging surveillance to monitor aneurysm progression.
Medical therapy alone is seldom curative but may be appropriate in select patients with stable, low-risk lesions.
Surgical Intervention
Surgery remains the gold standard for symptomatic, large, or expanding aneurysms, and when there is evidence of embolisation or risk of rupture. Surgical options include:
- Aneurysmectomy with reconstruction: Resection of the aneurysmal segment followed by primary anastomosis or interposition grafting (using autologous vein or synthetic graft).
- Ligation: Tying off the carotid artery proximal and distal to the aneurysm, occasionally performed when reconstruction is not feasible. However, this carries a risk of cerebral ischaemia, especially if collateral circulation is inadequate.
- Bypass procedures: Creating an alternative pathway for blood flow, such as a subclavian-to-carotid bypass, in complex cases.
Surgical management requires meticulous planning to minimise the risk of stroke, cranial nerve injury, and perioperative complications. Intraoperative neurophysiological monitoring and cerebral protection strategies are often employed.
Endovascular Techniques
Endovascular approaches have gained popularity in recent years, particularly for high-risk surgical candidates. Techniques include:
- Stent-graft placement: Deploying a covered stent across the aneurysm to exclude it from circulation while maintaining vessel patency.
- Coil embolisation: Inserting coils into the aneurysm sac to promote thrombosis and occlusion, used mainly for pseudoaneurysms or when preserving the parent artery is not essential.
Endovascular therapy offers reduced morbidity, shorter recovery times, and the possibility of treating anatomically challenging lesions. However, it may not be suitable for all aneurysm locations or morphologies, and long-term data on durability are still evolving.
Prognosis and Outcomes
The prognosis of carotid artery aneurysm disease is influenced by several factors, including aneurysm size, location, symptomatology, and treatment modality. Key considerations include:
- Untreated, symptomatic aneurysms carry a high risk of stroke, rupture, or death.
- Surgical and endovascular interventions offer good long-term outcomes, with reported survival rates exceeding 85% at five years for appropriately selected patients.
- Complications include perioperative stroke (3–10%), cranial nerve injury (5–15%), infection, and graft occlusion.
- Long-term follow-up with imaging is essential to detect recurrence, graft failure, or new aneurysm formation.
Overall, early diagnosis and intervention are associated with improved neurological outcomes and survival.
Prevention Strategies
Given the potentially devastating consequences of carotid artery aneurysms, preventive strategies focus on modifiable risk factors and early detection:
- Lifestyle modification: Smoking cessation, regular exercise, healthy diet, and weight management.
- Blood pressure and lipid control: Optimising management of hypertension and hyperlipidaemia through pharmacotherapy and lifestyle changes.
- Screening: Targeted screening in high-risk populations (e.g., those with connective tissue disorders, strong family history, or previous aneurysms) using non-invasive imaging.
- Infection control: Prompt treatment of systemic infections to reduce the risk of mycotic aneurysms.
- Trauma prevention: Use of protective equipment in high-risk occupations or activities.
Patient education and regular health check-ups play a vital role in early identification and management of risk factors.
Nursing Care of Patients with Carotid Artery Aneurysm
Nurses play a crucial role in the assessment, monitoring, and care of these patients, both in preoperative and postoperative settings. This document provides an extensive overview of the nursing care required for patients with carotid artery aneurysms, encompassing assessment, planning, interventions, and education.
Nursing Assessment
Nursing assessment for patients with carotid artery aneurysm is critical for early identification of complications and to guide ongoing care. The assessment includes:
- History Taking: Collect detailed medical and surgical history, including risk factors like hypertension, smoking, family history, previous vascular disease, and trauma.
- Physical Examination: Assess for a pulsatile mass in the neck, presence of bruit, signs of cerebral hypoperfusion (confusion, weakness, numbness, visual changes), and cranial nerve deficits.
- Vital Signs Monitoring: Monitor blood pressure and heart rate closely, as hypertension may predispose to aneurysm rupture.
- Neurological Assessment: Perform frequent neurological checks using standardized scales (e.g., Glasgow Coma Scale), monitor for changes in level of consciousness, speech, motor or sensory deficits.
- Pain Assessment: Evaluate for neck pain or headache, which may indicate aneurysm expansion or impending rupture.
- Assessment for Infection: Observe for signs of infection at or near the aneurysm site, especially in post-surgical patients.
Nursing Diagnoses
Common nursing diagnoses for patients with carotid artery aneurysm may include:
- Risk for impaired cerebral tissue perfusion related to altered carotid blood flow
- Acute pain related to aneurysm expansion or post-surgical incision
- Risk for bleeding related to aneurysm rupture or anticoagulation therapy
- Risk for infection related to invasive procedures or surgical intervention
- Anxiety related to diagnosis, risk of rupture, and potential for neurological deficits
- Deficient knowledge regarding disease process and treatment plan
Nursing Interventions
Nursing interventions are designed to manage symptoms, prevent complications, and promote recovery.
1. Monitoring and Assessment
- Monitor vital signs regularly, with special attention to blood pressure. Maintain blood pressure within the target range to reduce risk of rupture.
- Perform frequent neurological assessments, noting any changes as these may be early indicators of cerebral ischemia or stroke.
- Monitor for signs of aneurysm rupture, such as sudden onset of severe neck pain, hypotension, tachycardia, loss of consciousness, or expanding neck hematoma. Initiate emergency protocols if rupture is suspected.
2. Pain Management
- Administer prescribed analgesics and evaluate pain relief regularly.
- Employ non-pharmacological pain management strategies such as positioning, cold compresses, and relaxation techniques.
3. Prevention of Bleeding
- Monitor for signs of bleeding (e.g., bruising, hematoma, decreased hemoglobin or hematocrit).
- Educate the patient on avoiding activities that may increase intra-abdominal or thoracic pressure (e.g., heavy lifting, straining).
- If on anticoagulant therapy, closely monitor coagulation parameters and report abnormalities to the physician.
4. Infection Control
- Practice strict aseptic technique during all invasive procedures or dressing changes.
- Monitor incision or puncture sites for redness, swelling, discharge, or other signs of infection.
- Administer prescribed antibiotics as ordered, and monitor for adverse reactions.
- Encourage hand hygiene for staff, patients, and visitors.
5. Preoperative and Postoperative Care
- Preoperative: Assess baseline neurological status, explain the surgical procedure, obtain informed consent, and ensure preoperative tests are completed. Provide emotional support and address anxiety.
- Postoperative: Monitor neurological status and vital signs closely. Assess surgical site for bleeding or hematoma. Maintain prescribed head elevation. Ensure patency of airway, especially if neck swelling is present. Monitor for complications such as stroke, cranial nerve injury, or infection.
6. Patient and Family Education
- Educate on signs and symptoms of aneurysm rupture, stroke, and infection, and instruct when to seek immediate medical attention.
- Teach the importance of blood pressure control and medication adherence.
- Discuss lifestyle modifications to reduce risk factors, such as smoking cessation, healthy diet, and regular exercise.
- Provide information about the disease process, surgical or interventional procedures, and postoperative expectations.
- Support coping mechanisms for anxiety and fear related to the diagnosis and potential complications.
Multidisciplinary Collaboration
Nursing care requires close collaboration with the multidisciplinary team, including vascular surgeons, neurologists, radiologists, physiotherapists, and social workers. Nurses should participate in care conferences, communicate changes in patient status promptly, and coordinate post-discharge care and follow-up.
Complication Management
- Stroke: Monitor for new neurological deficits and report immediately. Prepare for rapid intervention as per stroke protocol.
- Rupture: Initiate emergency measures if rupture is suspected; maintain airway, support circulation with IV fluids, and prepare for immediate surgical intervention.
- Thromboembolism: Monitor for signs of distal embolization (limb ischemia, pain, pallor, pulselessness) and report findings.
- Cranial Nerve Injury: Assess for changes in swallowing, speech, tongue movement, and facial symmetry. Support rehabilitation as needed.
Discharge Planning and Follow-up
Effective discharge planning is essential to ensure continuity of care and prevent recurrence or complications.
- Arrange for follow-up appointments with vascular specialists and neurologists.
- Ensure patients understand the importance of medication adherence, symptom monitoring, and lifestyle changes.
- Provide written instructions and contact information for questions or emergency situations.
- Refer to rehabilitation services if neurological deficits are present.
REFERENCES
- American Association of Neurological Surgeons. Cerebral Aneurysm. https://www.aans.org/en/Patients/Neurosurgical-Conditions-and-Treatments/Cerebral-Aneurysm.
- Galyfos G, Eleftheriou M, Theodoropoulos C, et al. Open versus endovascular repair for extracranial carotid aneurysms. https://pubmed.ncbi.nlm.nih.gov/33940071/. J Vasc Surg. 2021;74(3):1017-1023.e5.
- Kraemer CJK, Zhou W. Carotid Aneurysm Review. Int J Angiol. 2019 Mar;28(1):17-19. doi: 10.1055/s-0039-1677675. Epub 2019 Feb 27. PMID: 30880886; PMCID: PMC6417903.
- Giannopoulos S, Trinidad E, Aronow H, Soukas P, Armstrong EJ. Εndovascular Repair of Extracranial Carotid Artery Aneurysms: A Systematic Review. https://pubmed.ncbi.nlm.nih.gov/31894734/. Vasc Endovascular Surg. 2020;54(3):254-263.
- Pourier VE, De Borst GJ. Which carotid artery aneurysms need to be treated (and how)? J Cardiovasc Surg (Torino). 2016 Apr;57(2):152-7. Epub 2015 Nov 24. PMID: 26603291.
- Sriamornrattanakul K, Sakarunchai I, Surgical treatment of large and giant cavernous carotid aneurysms. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5532919/. Asian J Neurosurg. 2017 Jul-Sep;12(3):382-388.
- Kejriwal S, Bulosan H, Nelken NA, Lim JH. Multidisciplinary Management of an Internal Carotid Artery Aneurysm Near the Skull Base. Cureus. 2024 Jun 10;16(6):e62086. doi: 10.7759/cureus.62086. PMID: 38989364; PMCID: PMC11236212.
- Vijaywargiya M, Deopujari R, Athavale SA. Anatomical study of petrous and cavernous parts of internal carotid artery. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5639169/. Anat Cell Biol. 2017 Sep;50(3):163-170.
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





