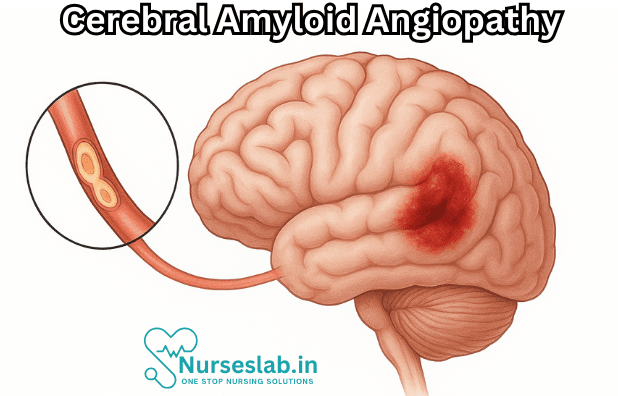
Cerebral Amyloid Angiopathy (CAA) is a progressive cerebrovascular disorder characterised by the deposition of amyloid beta (Aβ) peptides in the walls of small- to medium-sized cerebral vessels. This condition is a significant cause of spontaneous lobar intracerebral haemorrhage in the elderly and has profound implications for cognitive decline and dementia.
Introduction
Cerebral Amyloid Angiopathy (CAA) represents a spectrum of cerebrovascular disorders primarily marked by amyloid beta protein deposition within the walls of cortical and leptomeningeal blood vessels. First described in the early 20th century, CAA has since emerged as a central factor in age-related vascular cognitive impairment and spontaneous intracerebral haemorrhage.
The recognition of CAA’s role in neurological morbidity has grown with advances in neuroimaging and neuropathology. The disease is particularly significant due to its association with Alzheimer’s disease and its contribution to the growing burden of cognitive disorders in ageing populations.
Epidemiology
Prevalence
CAA is predominantly a disease of the elderly. Autopsy studies indicate that mild to moderate amyloid angiopathy is present in up to 30% of individuals over the age of 60 years, with severe cases identified in approximately 5–10% of this population. The prevalence is even higher among those with Alzheimer’s disease, where up to 90% may exhibit some degree of vascular amyloid deposition.
Risk Factors
Age is the most significant risk factor for CAA, with prevalence increasing sharply after the sixth decade of life. Other identified risk factors include:
- Genetic predisposition, particularly the presence of the apolipoprotein E (APOE) ε2 and ε4 alleles
- History of Alzheimer’s disease or other neurodegenerative disorders
- Hypertension, although its role is less pronounced compared to hypertensive arteriopathy
- Family history of cerebral haemorrhage or dementia
Demographic Distribution
CAA occurs globally, with no marked predilection for ethnicity or sex, though some studies suggest a slightly higher prevalence among women. The condition is rare in individuals below 55 years unless associated with hereditary forms.
Pathophysiology
Amyloid Beta Deposition
At the core of CAA pathology is the accumulation of amyloid beta (Aβ) peptides, primarily Aβ40, within the tunica media and adventitia of small- and medium-sized cortical and leptomeningeal arteries, arterioles, and capillaries. The deposition process disrupts vascular integrity, leading to weakening of vessel walls and a propensity for rupture.
Unlike Alzheimer’s disease, where Aβ42 is predominant in parenchymal plaques, CAA is characterised by the dominance of Aβ40 in vascular deposits. This distinction is relevant for understanding the pathobiology and potential therapeutic targets for both disorders.
Vascular Changes
Amyloid deposition initiates a cascade of vascular changes:
- Loss of smooth muscle cells in the vessel wall
- Thickening and splitting of the basement membrane
- Microaneurysm formation
- Fibrinoid necrosis and vessel fragility
These changes compromise the vessel’s structural integrity, increasing susceptibility to leakage, microhaemorrhages, and large lobar haemorrhages.
Genetic Factors
Genetic influences play a substantial role in the pathogenesis of CAA. The APOE ε2 and ε4 alleles are strongly associated with increased risk and severity. Hereditary forms, such as the Dutch type hereditary CAA, result from mutations in the Aβ precursor protein gene (APP), leading to early-onset disease with recurrent haemorrhages.
Clinical Features
Symptoms
The clinical spectrum of CAA ranges from asymptomatic cases identified at autopsy to catastrophic intracerebral haemorrhage. Common presentations include:
- Spontaneous, non-traumatic lobar intracerebral haemorrhages, often recurrent
- Cognitive impairment, particularly executive dysfunction and memory loss
- Transient focal neurological episodes (TFNEs), sometimes described as “amyloid spells”, which mimic transient ischaemic attacks
- Headache and seizures, less commonly
Types of Presentations
CAA typically presents in one of the following forms:
- Lobar Intracerebral Haemorrhage: Most characteristic, often affecting the occipital and parietal lobes. Haemorrhages are usually superficial, sparing the deep structures.
- Cognitive Decline: Gradual onset of dementia-like symptoms, particularly in elderly patients.
- Reversible Encephalopathy: Rarely, patients may develop an inflammatory response to vascular amyloid, resulting in subacute cognitive, behavioural, or focal deficits.
Associated Conditions
CAA is commonly associated with Alzheimer’s disease, sharing overlapping pathogenic mechanisms. It may also coexist with other small vessel diseases, such as hypertensive arteriopathy, and contribute to mixed dementia syndromes. In rare cases, CAA-related inflammation (CAA-ri) can mimic central nervous system vasculitis.
Diagnosis
Imaging Techniques
Neuroimaging plays a pivotal role in the diagnosis of CAA. The following modalities are most utilised:
- Magnetic Resonance Imaging (MRI): Susceptibility-weighted imaging (SWI) and gradient-recalled echo (GRE) sequences are highly sensitive for detecting cerebral microbleeds, which are characteristic of CAA.
- Computed Tomography (CT): Useful for identifying acute lobar haemorrhages, but less sensitive for chronic changes.
- Positron Emission Tomography (PET): Amyloid PET imaging can demonstrate amyloid deposition, though not yet a routine clinical tool.
The Boston Criteria, updated in 2022, provides a framework for the probable and possible diagnosis of CAA based on clinical, imaging, and pathological findings.
Laboratory Tests
There are currently no specific blood or cerebrospinal fluid biomarkers for CAA diagnosis in clinical practice. Research is ongoing to identify amyloid-related markers that could facilitate non-invasive diagnosis and monitoring.
Differential Diagnosis
CAA must be distinguished from other causes of intracerebral haemorrhage and cognitive decline, including:
- Hypertensive arteriopathy
- Vascular malformations
- Neoplasms
- Coagulopathies
- Primary and secondary CNS vasculitis
Careful clinical assessment and neuroimaging are essential for accurate diagnosis.
Management
Medical and Supportive Treatments
There is currently no cure for CAA, and management focuses on symptomatic treatment, prevention of complications, and supportive care.
- Acute Management: In cases of acute lobar haemorrhage, standard protocols for intracerebral haemorrhage are followed, including blood pressure control, reversal of anticoagulation, and neurosurgical intervention if indicated.
- Antithrombotic Therapy: The use of antiplatelet and anticoagulant medications is controversial due to the increased risk of haemorrhage. Decisions must be individualised, weighing the risks of ischaemic events against haemorrhagic complications.
- Seizure Management: Antiepileptic drugs are prescribed for patients with seizures, often following lobar haemorrhage.
- Cognitive and Supportive Care: Multidisciplinary approaches, including neuropsychological support, physiotherapy, and occupational therapy, are essential for improving quality of life and functional outcomes.
Prevention of Complications
Efforts to prevent recurrent haemorrhages and cognitive decline include:
- Strict blood pressure management
- Avoidance of unnecessary anticoagulation or antiplatelet therapy
- Patient education regarding symptom recognition and risk mitigation
Prognosis
Disease Progression
CAA is a chronic, progressive disorder. The risk of recurrent intracerebral haemorrhage is significant, particularly in patients with multiple prior haemorrhages and advanced age. Cognitive decline may progress over months to years, leading to substantial disability.
Outcomes and Quality of Life
Outcomes in CAA are variable and depend on the severity and frequency of haemorrhages, as well as the extent of cognitive impairment. Many patients experience reduced independence and increased care needs. Quality of life is often compromised due to recurrent neurological events, physical disability, and neuropsychiatric symptoms.
Nursing Care of Patients with Cerebral Amyloid Angiopathy
Effective nursing care for patients with CAA requires a nuanced understanding of the disease, its complications, and the comprehensive needs of affected individuals. This document provides a detailed guideline for nurses involved in the care of patients with CAA, spanning acute management, chronic care, patient education, and interdisciplinary collaboration.
Assessment and Monitoring
Nurses play a fundamental role in the early identification, ongoing assessment, and monitoring of patients with CAA.
- Neurological Assessment: Conduct frequent and thorough neurological checks, including assessment of level of consciousness, orientation, cranial nerve function, motor strength, sensory responses, speech, and gait. Document changes promptly and report significant findings.
- Vital Signs Monitoring: Monitor blood pressure, heart rate, temperature, and oxygen saturation regularly. Hypertension is a risk factor for hemorrhage and must be closely managed.
- Bleeding Risk Evaluation: Observe for signs of acute neurological deterioration (e.g., sudden headache, vomiting, focal deficits), which may indicate new bleeding. Monitor for signs of increased intracranial pressure, such as altered mental status, bradycardia, hypertension, and irregular respiration.
- Cognitive Function: Regularly evaluate cognitive status using standardized tools like the Mini-Mental State Examination (MMSE) or Montreal Cognitive Assessment (MoCA). Document changes in memory, judgment, language, and executive function.
- Seizure Surveillance: Be alert for signs of seizure activity, as CAA can increase seizure risk. Document and report any episodes of abnormal movements, altered awareness, or postictal confusion.
Acute Care Management
Patients may present acutely with cerebral hemorrhage or other neurological emergencies.
- Hemorrhagic Stroke Support: Administer care according to stroke protocols. Ensure airway patency, breathing, and circulation are stable. Position the patient to optimize cerebral perfusion and minimize aspiration risk if consciousness is impaired.
- Medication Safety: Avoid antithrombotic and anticoagulant medications unless specifically indicated by the medical team, as these can increase bleeding risk in CAA patients.
- Blood Pressure Control: Implement physician-directed protocols for blood pressure management. Maintain blood pressure within safe parameters to decrease the risk of rebleeding.
- Seizure Management: Administer antiepileptic drugs as prescribed. Observe for side effects and therapeutic response. Protect the patient during seizures and minimize injury risk.
- Intracranial Pressure Monitoring: In severe cases, collaborate with the medical team to monitor and manage intracranial pressure (ICP). Apply appropriate interventions such as head elevation, minimizing stimulation, and avoiding factors that increase ICP.
Chronic Care and Rehabilitation
Due to the chronic and progressive nature of CAA, long-term nursing care focuses on maximizing independence, preventing complications, and supporting cognitive and emotional well-being.
- Fall Prevention: Assess risk for falls frequently. Implement safety measures such as bed alarms, non-slip footwear, assistive devices, and environmental modifications.
- Mobility Support: Encourage participation in physical therapy and occupational therapy. Assist with safe transfers and ambulation while promoting patient autonomy.
- Pressure Ulcer Prevention: Regularly reposition patients with impaired mobility. Assess skin integrity, provide appropriate mattresses and cushions, and maintain good nutrition and hydration.
- Cognitive and Emotional Support: Provide cognitive stimulation and reality orientation. Engage the patient in activities that support memory and executive function. Offer emotional support and monitor for depression, anxiety, and behavioral changes.
- Nutrition and Hydration: Monitor nutritional status, especially in patients with dysphagia or reduced ability to self-feed. Collaborate with dietitians to provide appropriate diets, and monitor for signs of malnutrition or dehydration.
- Medication Adherence: Educate the patient and caregivers about prescribed medications, their purposes, and possible side effects. Establish routines and reminders to enhance compliance.
Patient and Family Education
Education is vital for empowering patients and their families to manage the challenges associated with CAA:
- Disease Understanding: Explain the nature of CAA, its symptoms, and potential complications in simple, jargon-free language.
- Warning Signs: Teach patients and families to recognize symptoms of acute hemorrhage (e.g., sudden headache, weakness, speech changes), seizure activity, and cognitive decline. Provide clear instructions for seeking emergency help.
- Lifestyle Modifications: Advise on maintaining a healthy lifestyle, including a balanced diet, regular exercise, blood pressure management, and avoidance of smoking or excess alcohol.
- Adherence to Follow-up: Stress the importance of regular follow-up appointments, neuroimaging (as ordered), and ongoing assessment by the healthcare team.
- Home Safety: Provide guidance on making the home environment safer to prevent falls and accidents.
- Support Resources: Connect families to support groups, counseling services, and community resources for practical and emotional support.
Interdisciplinary Collaboration
Optimal care for CAA patients involves teamwork among nurses, physicians, neurologists, rehabilitation specialists, dietitians, social workers, and pharmacists.
- Communication: Maintain open, timely communication with all healthcare providers regarding the patient’s status, concerns, and changes in condition.
- Care Coordination: Participate in multidisciplinary rounds and care planning meetings to ensure a comprehensive, individualized approach.
- Discharge Planning: Begin planning for discharge early, involving the patient and family in setting goals and addressing long-term needs.
Ethical and End-of-Life Considerations
Due to the progressive and incurable nature of CAA, nurses should address ethical challenges and end-of-life care.
- Advance Care Planning: Encourage discussions about advance directives, living wills, and the patient’s preferences for care in the event of severe disability or recurrent hemorrhage.
- Palliative Care: Initiate referrals to palliative care services as appropriate. Focus on symptom management, comfort, dignity, and quality of life.
- Support for Caregivers: Acknowledge the emotional burden on caregivers. Offer resources for respite care and counseling.
Summary and Key Points
- Cerebral Amyloid Angiopathy is a chronic, progressive disorder with significant risks for hemorrhagic stroke and cognitive decline.
- Nursing care must be comprehensive, integrating acute management, rehabilitation, education, and emotional support.
- Patient safety, prevention of complications, and quality of life are central to care planning.
- Collaboration with families and the interdisciplinary team is essential for optimal outcomes.
Nurses, as frontline caregivers, have a unique and powerful role in supporting patients with CAA and helping them navigate the complex challenges of this condition with compassion, expertise, and advocacy.
REFERENCES
- Kozberg MG, Perosa V, Gurol ME, van Veluw SJ. A practical approach to the management of cerebral amyloid angiopathy. Int J Stroke. 2021 Jun;16(4):356-369.
- Kuhn J, Sharman T. Cerebral Amyloid Angiopathy. [Updated 2023 Jun 5]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK556105/
- Banerjee G, Collinge J, Fox NC. Clinical considerations in early-onset cerebral amyloid angiopathy. https://pubmed.ncbi.nlm.nih.gov/37280119/. Brain. 2023 Oct 3;146(10):3991-4014.
- Charidimou A, Boulouis G, Frosch MP, et al. The Boston criteria version 2.0 for cerebral amyloid angiopathy: a multicentre, retrospective, MRI-neuropathology diagnostic accuracy study. https://pubmed.ncbi.nlm.nih.gov/35841910/. Lancet Neurol. 2022 Aug;21(8):714-725.
- Cozza M, Amadori L, Boccardi V. Exploring cerebral amyloid angiopathy: Insights into pathogenesis, diagnosis, and treatment. (https://pubmed.ncbi.nlm.nih.gov/37931443/) J Neurol Sci. 2023 Nov 15;454:120866.
- Inoue Y, Ando Y, Misumi Y, et. al. Current Management and Therapeutic Strategies for Cerebral Amyloid Angiopathy.. .h ttps://pubmed.ncbi.nlm.nih.gov/33918041/ Int J Mol Sci. 2021 Apr 8;22(8):3869.
- Cordonnier C, Klijn C, Smith EE, et al. Diagnosis and management of cerebral amyloid angiopathy: a scientific statement from the International CAA Association and the World Stroke Organization. International Journal of Stroke. 2025;20(8):949-967. doi:10.1177/17474930251365861
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





