Chronic Myeloid Leukemia (CML) is a slow‑progressing blood cancer linked to the Philadelphia chromosome, leading to uncontrolled myeloid cell growth. Understanding its symptoms, phases, diagnosis, and targeted treatments is essential in hematology, oncology, and nursing practice.
Introduction
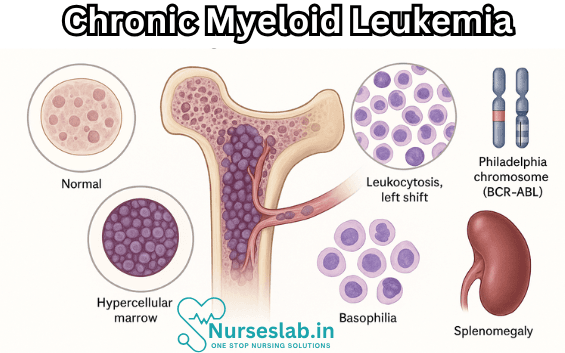
Chronic Myeloid Leukemia (CML) is a clonal myeloproliferative neoplasm of the haematopoietic stem cell, primarily characterised by uncontrolled proliferation of myeloid cells in the bone marrow and their accumulation in the blood. It is distinguished by the presence of the Philadelphia chromosome, resulting from a reciprocal translocation between chromosomes 9 and 22.
This genetic abnormality leads to the formation of the BCR-ABL fusion gene, a constitutively active tyrosine kinase driving the pathogenesis of CML. The disease typically progresses through three phases: chronic, accelerated, and blast crisis, each with distinct clinical and laboratory features. CML has become a paradigm for targeted cancer therapy, with the development of tyrosine kinase inhibitors (TKIs) revolutionising its management and prognosis.
Epidemiology
CML represents approximately 15-20% of all leukaemias in adults. The annual incidence is estimated at 1-2 cases per 1 lakh population globally, with a slightly higher prevalence in males compared to females. The median age at diagnosis is around 55 years, though it can occur at any age, including in children and adolescents, albeit rarely.
Geographically, CML incidence is relatively uniform worldwide, with minor variations attributable to reporting differences and population demographics. There is no strong evidence of ethnic or racial predilection. In India, the incidence of CML appears consistent with global figures, although underreporting and limited access to specialised healthcare in rural areas may affect precise estimates.
The only well-established risk factor for CML is exposure to high-dose ionising radiation, as observed in atomic bomb survivors. Other potential risk factors, such as exposure to chemicals (e.g., benzene), have not been conclusively linked to the disease. Unlike acute leukaemias, familial clustering and hereditary predisposition to CML are exceedingly rare.
Etiology and Pathogenesis
The hallmark of CML is the presence of the Philadelphia chromosome, a shortened chromosome 22 created by a balanced translocation t(9;22)(q34;q11). This chromosomal rearrangement juxtaposes the breakpoint cluster region (BCR) gene on chromosome 22 with the Abelson murine leukaemia viral oncogene homolog 1 (ABL1) gene on chromosome 9, resulting in the BCR-ABL fusion gene.
The BCR-ABL gene encodes a constitutively active tyrosine kinase protein, which continuously stimulates the RAS, PI3K/AKT, and JAK/STAT signalling pathways. This persistent activation leads to increased proliferation of myeloid cells, inhibition of apoptosis, and altered adhesion properties, culminating in the accumulation of mature and immature granulocytes in the bone marrow and peripheral blood.
The pathogenesis of CML is a multi-step process. The BCR-ABL kinase is necessary and sufficient for the development of CML, but disease progression from the indolent chronic phase to the aggressive blast crisis often involves additional genetic and epigenetic alterations. These may include mutations in tumour suppressor genes (e.g., p53), activation of other oncogenes, and genomic instability.
Clinical Features
CML typically presents in three distinct phases, each with characteristic clinical and laboratory findings:
- Chronic Phase: This initial phase accounts for approximately 85% of cases at diagnosis. Patients may be asymptomatic or exhibit non-specific symptoms such as fatigue, weight loss, night sweats, and malaise. Splenomegaly is common and may cause left upper quadrant discomfort or early satiety. Laboratory findings show marked leukocytosis, often exceeding 1 lakh/cu mm, with a left shift (increased immature granulocytes), basophilia, and eosinophilia. Anaemia and thrombocytosis may also be present.
- Accelerated Phase: This intermediate stage is characterised by increasing symptoms, progressive splenomegaly, rising white cell counts unresponsive to therapy, and worsening anaemia or thrombocytopenia. Blasts account for 10–19% of peripheral blood or bone marrow cells. Additional cytogenetic abnormalities may develop.
- Blast Crisis: Representing disease transformation to acute leukaemia (usually myeloid, occasionally lymphoid), this phase is defined by ≥20% blasts in the blood or marrow, or by extramedullary blast proliferation. Patients present with severe constitutional symptoms, bleeding, infections, and rapidly progressive organomegaly. Prognosis is poor at this stage.
Other clinical manifestations may include bone pain, fever, infections, and, rarely, priapism or visual disturbances due to hyperleukocytosis. The disease course is variable, but without effective therapy, most patients progress from the chronic phase to blast crisis within 3–5 years.
Diagnosis
The diagnosis of CML is based on a combination of clinical, haematological, cytogenetic, and molecular findings.
- Complete Blood Count (CBC) and Peripheral Blood Film: The CBC typically reveals marked leukocytosis with a full spectrum of myeloid precursors. The peripheral smear shows mature and immature granulocytes, basophilia, and eosinophilia. Anaemia and variable platelet counts may be observed.
- Bone Marrow Aspiration and Biopsy: Bone marrow examination demonstrates hypercellularity, granulocytic hyperplasia, and varying degrees of fibrosis. Blasts are <10% in chronic phase, increasing in accelerated and blast phases.
- Cytogenetic Analysis: Conventional karyotyping identifies the Philadelphia chromosome in more than 90% of cases. Fluorescence in situ hybridisation (FISH) can detect the BCR-ABL fusion gene with high sensitivity.
- Molecular Diagnostics: Reverse transcription polymerase chain reaction (RT-PCR) detects BCR-ABL transcripts, confirming the diagnosis and allowing for sensitive monitoring of minimal residual disease (MRD).
- Other Investigations: Biochemical tests may reveal elevated lactate dehydrogenase (LDH) and uric acid due to high cell turnover. Imaging (ultrasound, CT) may be used to assess splenomegaly and extramedullary disease.
Diagnostic criteria for CML require the demonstration of the BCR-ABL fusion gene or Philadelphia chromosome in the context of a compatible clinical and haematological picture.
Treatment
The management of CML has evolved dramatically over the past two decades, with the advent of targeted therapies transforming patient outcomes.
Tyrosine Kinase Inhibitors (TKIs)
TKIs are the mainstay of CML treatment. Imatinib mesylate, the first-generation TKI, selectively inhibits the BCR-ABL kinase, leading to profound and durable remissions in most patients. Second-generation TKIs such as dasatinib, nilotinib, and bosutinib offer increased potency and efficacy, particularly in imatinib-resistant cases. Third-generation TKIs like ponatinib are reserved for patients with specific mutations (e.g., T315I) conferring resistance to earlier agents.
Treatment is usually initiated at diagnosis, with the choice of TKI influenced by patient age, comorbidities, risk profile, and mutation status. Regular molecular monitoring (quantitative PCR for BCR-ABL transcripts) guides therapy and detects treatment failure or resistance.
Chemotherapy
Conventional chemotherapeutic agents, such as hydroxyurea and busulfan, were historically used to control leukocytosis and symptoms, but have largely been supplanted by TKIs. Chemotherapy may still play a role in advanced or blast phase CML, often in combination with TKIs or as a bridge to stem cell transplantation.
Allogeneic Stem Cell Transplantation (SCT)
Allogeneic haematopoietic stem cell transplantation remains the only known curative modality for CML. It is primarily considered in younger patients with high-risk disease, TKI resistance, or progression to advanced phases. SCT carries significant risks, including graft-versus-host disease (GVHD), infection, and transplant-related mortality, limiting its use to selected patients.
Supportive Care
Supportive care measures are crucial, particularly during advanced disease or treatment complications. These include management of anaemia, infections, bleeding, hyperuricaemia, and psychosocial support. Vaccinations, growth factors, and transfusions may be required in specific settings.
Other Modalities
Interferon-alpha, once a mainstay of therapy, is now rarely used except in selected populations (e.g., pregnant women or those intolerant to TKIs). Emerging therapies are being explored for patients with refractory disease.
Prognosis
The prognosis of CML has improved remarkably in the era of TKIs. With optimal therapy, the 10-year survival rate approaches 80-90%, and many patients achieve near-normal life expectancy. The chronic phase, when diagnosed and treated early, is associated with excellent outcomes.
Several factors influence prognosis in CML:
- Phase at Diagnosis: Patients diagnosed in the chronic phase fare significantly better than those in accelerated or blast crisis.
- Response to Therapy: Early and deep molecular responses predict durable remissions and improved survival.
- Age and Comorbidities: Advanced age and coexisting illnesses may limit treatment options and increase risk.
- Additional Cytogenetic Abnormalities: The presence of secondary chromosomal changes can indicate a higher risk of progression.
- TKI Resistance: Mutations in the BCR-ABL kinase domain may confer resistance to therapy, necessitating alternative approaches.
Prognostic scoring systems such as the Sokal, Hasford, and EUTOS scores integrate clinical and laboratory parameters to stratify patients and guide management decisions.
Nursing Care of Patients with Chronic Myeloid Leukemia (CML)
Nurses play a pivotal role in supporting patients through the diagnosis, treatment, and long-term management of Chronic Myeloid Leukemia.
Assessment and Initial Evaluation
Effective nursing care begins with a thorough assessment:
- History Taking: Explore presenting symptoms, such as fatigue, weight loss, night sweats, bone pain, abdominal discomfort, and recurrent infections or bleeding.
- Physical Examination: Assess for splenomegaly, hepatomegaly, pallor, bruising, and signs of infection.
- Laboratory and Diagnostic Studies: Monitor complete blood counts, bone marrow biopsy results, cytogenetic and molecular analyses (BCR-ABL gene), and liver/renal function tests.
Nurses should develop a baseline understanding of the patient’s physical, psychological, and social status to tailor individualized care plans.
Core Nursing Diagnoses
Common nursing diagnoses for patients with CML include:
- Risk for infection related to immunosuppression
- Fatigue related to anemia and disease process
- Risk for bleeding related to thrombocytopenia
- Impaired comfort related to treatment side effects and disease symptoms
- Knowledge deficit related to disease process and medication regimen
- Disturbed body image and anxiety related to chronic illness
Planning and Implementation of Care
1. Infection Prevention and Control
- Implement strict hand hygiene practices for staff, patients, and visitors.
- Encourage patients to avoid crowded places and individuals with infections.
- Monitor for signs of infection: fever, chills, cough, sore throat, urinary symptoms, and skin changes.
- Administer prophylactic antibiotics or antivirals as per physician orders.
- Educate on proper oral care to prevent mucositis and dental infections.
- Maintain aseptic technique for all invasive procedures.
2. Management of Fatigue
- Assess the degree and impact of fatigue on daily activities.
- Encourage energy conservation techniques: prioritizing activities, taking rest periods, and delegating tasks.
- Promote a balanced diet rich in iron and proteins to address anemia.
- Involve physiotherapy for light exercises to enhance stamina and overall well-being.
- Provide emotional support, validate feelings of exhaustion, and encourage social support networks.
3. Bleeding Precautions
- Monitor platelet counts and observe for signs of bleeding: petechiae, bruising, gum bleeding, hematuria, or gastrointestinal bleeding.
- Teach patients to avoid activities that increase bleeding risk, such as contact sports or using sharp objects.
- Use soft toothbrushes and electric razors.
- Apply pressure after blood draws or injections.
- Promptly report any unusual bleeding to the healthcare team.
4. Comfort and Symptom Management
- Assess and manage pain using appropriate pharmacological and non-pharmacological methods.
- Monitor for side effects of therapies, such as tyrosine kinase inhibitors (TKIs)—including nausea, diarrhea, muscle cramps, edema, and skin rashes.
- Administer antiemetics and antidiarrheals as ordered.
- Promote relaxation techniques: deep breathing exercises, guided imagery, or meditation.
- Provide a calm, restful environment to enhance comfort.
5. Patient Education and Support
- Explain the nature and chronicity of CML, emphasizing the importance of long-term follow-up and adherence to therapy.
- Educate about medication regimens, especially the correct administration of oral TKIs, possible side effects, and the necessity of not missing doses.
- Encourage regular laboratory monitoring and clinic visits.
- Discuss fertility concerns and family planning, as some treatments may affect reproductive health.
- Provide information about community resources, support groups, and counseling services.
6. Psychological and Social Support
- Assess for emotional responses, including anxiety, depression, or fear of relapse.
- Offer opportunities for patients to express concerns and fears about their diagnosis and prognosis.
- Refer to mental health professionals when appropriate.
- Facilitate communication among patients, families, and the healthcare team.
- Encourage engagement with support groups for patients with leukemia or chronic illnesses.
Monitoring and Ongoing Evaluation
Ongoing assessment is essential to adjust care plans in response to the patient’s needs:
- Monitor complete blood counts, BCR-ABL transcript levels, and side effects of therapy at regular intervals.
- Assess for response to treatment: reduction in white blood cell counts and improvement in symptoms.
- Track adverse reactions, medication adherence, and psychological well-being.
- Maintain open lines of communication with the entire healthcare team, updating them on any changes in the patient’s condition.
Interdisciplinary Collaboration
Successful management of CML involves a multidisciplinary approach:
- Physicians—Direct overall care, prescribe and adjust therapy.
- Nurses—Coordinate care, monitor status, educate, and provide support.
- Pharmacists—Assist with medication management and side effect mitigation.
- Social Workers—Aid in accessing community resources and navigating insurance or financial concerns.
- Dietitians—Advise on nutritional needs, especially in the context of anemia or gastrointestinal side effects.
- Mental Health Professionals—Support psychological health and adjustment to chronic illness.
Special Considerations in CML Nursing Care
- Pediatric Patients: Require age-appropriate communication and family involvement in care planning.
- Pregnant Patients: Must be managed carefully to balance maternal and fetal health; certain therapies may be contraindicated.
- Elderly Patients: May have comorbidities and polypharmacy concerns that complicate treatment.
- Financial Toxicity: Cost of TKIs can be high—assist patients in accessing financial assistance programs if needed.
Palliative and End-of-Life Care
While many CML patients now experience long-term remission, some may progress to advanced phases or develop resistance to therapy. At this point, focus shifts to palliative care:
- Provide symptom relief and comfort measures.
- Address goals of care, advance directives, and end-of-life wishes.
- Support family members through anticipatory grief and bereavement.
- Coordinate hospice care when appropriate.
REFERENCES
- Nassar AK, et al. The Spleen. In: Sabiston Textbook of Surgery. 21st ed. Elsevier; 2022. https://www.clinicalkey.com.
- Kaushansky K, et al., eds. Chronic myelogenous leukemia and related disorders. In: Williams Hematology. 10th ed. McGraw Hill; 2021. https://accessmedicine.mhmedical.com.
- Cancer Support Community. Chronic Myeloid Leukemia. https://www.cancersupportcommunity.org/chronic-myeloid-leukemia.
- Cerveira N, Bizarro S, Teixeira MR, Mariz JM. When to Stop TKIs in Patients with Chronic Myeloid Leukemia and How to Follow Them Subsequently. https://pubmed.ncbi.nlm.nih.gov/33866455/) Curr Treat Options Oncol. 2021 Apr 17;22(6):49.
- National Cancer Institute. Stopping TKI Treatment is Safe, Improves Quality of Life for Some with CML.. https://www.cancer.gov/news-events/cancer-currents-blog/2020/cml-stopping-tki-treatment-improves-quality-of-life
- Rea D, Cayuela JM. Treatment-free remission in patients with chronic myeloid leukemia.. https://pubmed.ncbi.nlm.nih.gov/28689264/Int J Hematol. 2018 Oct;108(4):355-364.
- Yassin MA, et al. Ophthalmologic manifestations as the initial presentation of chronic myeloid leukemia: A review. Survey of Ophthalmology. 2022; doi:10.1016/j.survophthal.2021.07.001.
- Shanmuganathan N, Hiwase DK, Ross DM. Treatment of chronic myeloid leukemia: assessing risk, monitoring response, and optimizing outcome.. https://pubmed.ncbi.nlm.nih.gov/28482729/ Leuk Lymphoma. 2017 Dec;58(12):2799-2810.
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





