Chronic sinusitis is persistent inflammation of the sinuses lasting more than 12 weeks, leading to congestion, facial pain, and impaired drainage. Understanding its causes, symptoms, diagnosis, and management is essential in ENT, nursing, and clinical practice.
Introduction
It is also known as chronic rhinosinusitis (CRS), is a prevalent and often debilitating condition characterised by persistent inflammation of the paranasal sinuses and nasal passages for a duration of at least 12 weeks. Unlike acute sinusitis, which is typically short-lived and resolves with or without treatment, chronic sinusitis is marked by recurrent or continuous symptoms that can significantly impair an individual’s quality of life.
Anatomy and Physiology of the Sinuses
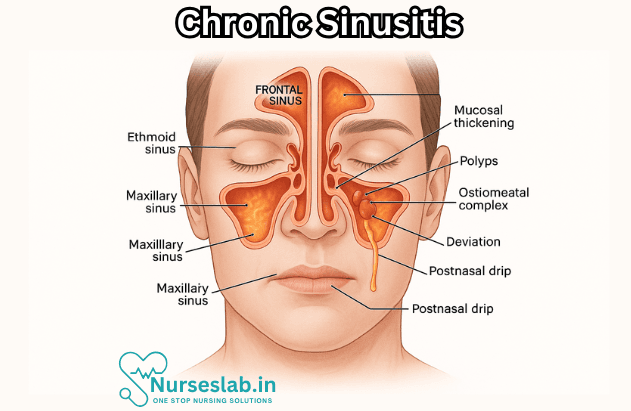
The paranasal sinuses are air-filled cavities located within the bones of the skull and face, closely associated with the nasal cavity. There are four paired sinuses: the maxillary, frontal, ethmoid, and sphenoid sinuses. These structures are lined with mucous membranes and play several roles, including humidifying inspired air, enhancing voice resonance, reducing the weight of the skull, and acting as a buffer against facial trauma.
The mucociliary clearance system is vital for sinus health. Cilia, or tiny hair-like structures, propel mucus produced by the sinus lining toward the natural sinus openings (ostia) and into the nasal cavity. This mechanism helps trap and expel pathogens, allergens, and debris. When this system is disrupted, mucus stasis and infection can ensue, setting the stage for sinusitis.
Etiology and Risk Factors
It is a multifactorial condition resulting from a complex interplay of infectious, inflammatory, anatomical, and environmental factors. Understanding these contributors is crucial for effective management and prevention.
Infectious Causes
Although viral upper respiratory tract infections (such as the common cold) are the most frequent precipitating events, chronic sinusitis is often associated with persistent bacterial or, less commonly, fungal infections. The most common bacteria implicated include Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis. Fungal sinusitis is more likely in immunocompromised individuals or those with specific environmental exposures.
Allergic Factors
Allergic rhinitis, commonly known as hay fever, is a significant risk factor for chronic sinusitis. This reactions cause inflammation and swelling of the nasal mucosa, leading to blockage of the sinus ostia and impaired mucus drainage. This creates a favourable environment for infection and chronic inflammation.
Anatomical Abnormalities
Structural factors such as deviated nasal septum, nasal polyps, hypertrophy of the turbinates, and congenital malformations can impede sinus drainage. These anatomical variations can predispose individuals to recurrent or persistent sinus infections.
Environmental and Lifestyle Factors
Exposure to environmental pollutants, cigarette smoke, occupational irritants, and extremes of humidity or temperature can damage the nasal mucosa and impair mucociliary function. Additionally, frequent air travel and swimming in chlorinated pools have been implicated as risk factors.
Other Medical Conditions
In Chronic sinusitis is more prevalent in individuals with certain medical conditions, such as asthma, cystic fibrosis, primary ciliary dyskinesia, and immunodeficiency disorders. Gastro-oesophageal reflux disease (GERD) has also been associated with increased risk, possibly due to the reflux of stomach acids into the upper airway.
Pathophysiology
The pathogenesis of chronic sinusitis involves persistent inflammation of the sinus mucosa, leading to mucosal thickening, polyp formation, and impaired mucociliary clearance. The cycle often begins with an initial insult—such as a viral infection or allergen exposure—that causes mucosal oedema and ostial obstruction. This blockage hinders normal mucus drainage, promoting retention of secretions and secondary bacterial or fungal colonisation.
Chronic inflammation is perpetuated by a complex cascade of immunological responses, including the recruitment of inflammatory cells (neutrophils, eosinophils, lymphocytes) and the release of cytokines and mediators. Over time, these processes can result in tissue remodelling, fibrosis, and the development of nasal polyps. In some cases, chronic sinusitis may occur without an identifiable infectious agent, highlighting the role of non-infectious inflammation.
Clinical Presentation
In this disease typically presents with a constellation of symptoms that persist for at least 12 weeks, distinguishing it from acute sinusitis, which usually resolves within four weeks. The hallmark features include:
- Nasal obstruction or congestion: Persistent blockage or stuffiness of the nasal passages.
- Facial pain or pressure: Discomfort, tenderness, or a feeling of fullness over the affected sinuses (often the cheeks, forehead, or around the eyes).
- Purulent nasal discharge: Thick, discoloured mucus draining from the nose or down the back of the throat (postnasal drip).
- Reduced or lost sense of smell (hyposmia or anosmia): Frequently reported, especially in cases with nasal polyps.
Other associated symptoms may include headache, fatigue, cough (particularly at night), sore throat, ear pain or fullness, halitosis, and dental pain. The severity and combination of symptoms can vary widely among individuals.
It is important to differentiate chronic sinusitis from acute sinusitis and other causes of facial pain, such as migraine, dental infections, or temporomandibular joint disorders. Chronic sinusitis is diagnosed based on the duration and persistence of symptoms, typically lasting 12 weeks or longer despite appropriate therapy.
Diagnosis
A thorough clinical evaluation is essential for the diagnosis of chronic sinusitis. The diagnostic process generally includes:
History and Physical Examination
- Detailed symptom assessment: Duration, severity, and nature of symptoms, as well as any history of allergies, asthma, or previous sinusitis episodes.
- Physical examination: Inspection of the nasal cavity using an otoscope or nasal speculum to assess for mucosal oedema, purulent discharge, polyps, or structural abnormalities.
Imaging Studies
- Computed Tomography (CT) Scan: The most sensitive imaging modality for evaluating sinus anatomy, extent of disease, and presence of complications. CT scans reveal mucosal thickening, opacification, and anatomical variations.
- Magnetic Resonance Imaging (MRI): Reserved for cases where malignancy or fungal infection is suspected, or when intracranial or orbital complications are considered.
Endoscopic Evaluation
Nasal endoscopy allows direct visualisation of the nasal passages and sinus openings. It helps identify polyps, purulent secretions, and anatomical obstructions. Tissue samples may be obtained for culture or histopathological analysis in select cases.
Laboratory Tests
- Microbiological cultures: Useful in refractory cases to identify causative organisms and guide antibiotic therapy.
- Allergy testing: Indicated when allergic rhinitis is suspected as a contributing factor.
- Immunological workup: In patients with recurrent or atypical infections, to detect underlying immunodeficiencies.
Treatment and Management
The management of chronic sinusitis is multifaceted, aiming to reduce mucosal inflammation, restore normal sinus drainage, treat underlying infections or allergies, and prevent recurrence. Treatment strategies are individualised based on the severity of symptoms, underlying causes, and presence of complications.
Medical Therapies
- Intranasal corticosteroids: First-line therapy for reducing inflammation and polyp size. Examples include fluticasone, mometasone, and budesonide. These sprays are generally well tolerated and can be used long-term.
- Saline nasal irrigation: Regular rinsing of the nasal passages with saline solution helps clear mucus, allergens, and pathogens, improving symptoms and mucociliary function.
- Antibiotics: Reserved for cases with evidence of bacterial infection or acute exacerbations. Prolonged courses (3–6 weeks) may be required, guided by culture results when possible.
- Oral corticosteroids: Short courses may be prescribed in severe cases or when nasal polyps are present. Long-term use is avoided due to potential side effects.
- Antihistamines and leukotriene modifiers: Beneficial in patients with underlying allergic rhinitis.
- Decongestants: May provide temporary relief of nasal congestion but are not recommended for long-term use due to rebound effects.
Surgical Options
Surgery is considered when medical therapy fails or in the presence of anatomical obstructions that cannot be managed conservatively. The primary surgical procedure is functional endoscopic sinus surgery (FESS), which involves using minimally invasive techniques to remove obstructions, restore sinus drainage, and improve ventilation. Other procedures may include polypectomy (removal of nasal polyps), septoplasty (correction of septal deviation), or turbinate reduction.
Postoperative care includes continued use of nasal corticosteroids, saline irrigation, and regular follow-up to monitor for recurrence or complications.
Lifestyle Modifications
- Avoidance of known allergens and irritants.
- Smoking cessation and minimising exposure to second-hand smoke.
- Maintaining optimal humidity levels in living and working environments.
- Regular hand hygiene to reduce the risk of respiratory infections.
Complications
If left untreated or inadequately managed, chronic sinusitis can lead to significant complications, some of which may be life-threatening:
- Orbital complications: Spread of infection to the eye socket can cause orbital cellulitis, abscess formation, or vision loss.
- Intracranial complications: Rare but serious, including meningitis, brain abscess, or cavernous sinus thrombosis.
- Osteomyelitis: Infection of the bones surrounding the sinuses, particularly in children.
- Asthma exacerbation: Chronic sinusitis can worsen asthma control and increase the frequency of attacks.
- Chronic headache and facial pain: Persistent inflammation may contribute to ongoing discomfort and reduced quality of life.
Prevention Strategies
Several measures can help reduce the risk of developing chronic sinusitis or prevent recurrence in susceptible individuals:
- Manage and treat allergic rhinitis promptly and effectively.
- Avoid exposure to environmental pollutants, smoke, and occupational irritants.
- Use saline nasal irrigation regularly, especially during periods of increased risk (e.g., cold and flu season).
- Address structural abnormalities of the nasal cavity and sinuses when clinically indicated.
- Maintain good personal hygiene and handwashing practices to limit the spread of infections.
- Seek prompt treatment for acute sinusitis to prevent progression to chronic disease.
Impact on Quality of Life
This condition is more than a simple nuisance; it can profoundly affect an individual’s physical, emotional, and social well-being. Persistent symptoms such as nasal congestion, facial pain, and sleep disturbances can lead to chronic fatigue, impaired concentration, and reduced productivity at work or school. Many patients report difficulties in performing daily activities, engaging in social interactions, and maintaining relationships.
The psychological impact is also significant, with higher rates of anxiety, depression, and decreased overall life satisfaction observed among individuals with chronic sinusitis. Sleep disturbances, including obstructive sleep apnoea, are common and further aggravate fatigue and mood disorders. The burden of frequent medical visits, medication use, and potential surgeries adds to the overall stress and financial strain.
For those with coexisting conditions such as asthma or allergic rhinitis, the interplay of symptoms can complicate management and further diminish quality of life. Effective treatment and support can help mitigate these effects and restore a greater sense of well-being.
Nursing Care of Patients with Chronic Sinusitis
Effective nursing care plays a pivotal role in the management, symptom relief, and overall recovery of patients with chronic sinusitis.
Nursing Assessment
A thorough assessment is the foundation for appropriate nursing care. Nurses should gather a detailed history and perform a physical examination focused on identifying the severity and triggers of chronic sinusitis.
- History Taking: Document onset, duration, frequency, and progression of symptoms. Assess for history of allergies, previous sinus infections, surgical interventions, and occupational/environmental exposures.
- Physical Examination: Inspect for nasal discharge, swelling, redness, tenderness over sinuses, and any anatomical abnormalities.
- Subjective Complaints: Encourage patients to describe their symptoms, including pain location and severity, nasal blockage, and any changes in smell or taste.
- Diagnostic Tests: Support physicians in obtaining and interpreting results from nasal endoscopy, imaging studies (CT scan, MRI), and allergy testing as ordered.
Nursing Diagnosis
Based on assessment data, the following nursing diagnoses may be appropriate for patients with chronic sinusitis:
- Ineffective airway clearance related to increased nasal secretions and inflammation.
- Acute or chronic pain related to sinus pressure and inflammation.
- Disturbed sleep pattern related to nasal congestion and discomfort.
- Impaired mucous membrane integrity related to ongoing infection and inflammation.
- Deficient knowledge regarding disease process, triggers, and self-care strategies.
- Risk for infection related to impaired sinus drainage and mucosal defenses.
Nursing Interventions
Effective nursing care focuses on symptom relief, prevention of complications, education, and emotional support for the patient.
1. Airway Clearance
- Encourage Adequate Hydration: Promote fluid intake to help thin mucus and facilitate drainage.
- Facilitate Nasal Irrigation: Teach patients the use of saline nasal sprays or washes to clear nasal passages and reduce congestion.
- Steam Inhalation: Recommend safe methods of inhaling steam to soothe irritated mucosa and aid mucus clearance.
- Positioning: Advise patients to sleep with their head elevated to promote sinus drainage.
- Monitor for Signs of Complications: Observe for worsening symptoms, fever, or signs of orbital or intracranial involvement, and report promptly.
2. Pain Management
- Assessment of Pain: Regularly assess pain intensity, location, and characteristics. Use pain scales to monitor changes over time.
- Pharmacological Interventions: Administer prescribed analgesics, decongestants, or nasal corticosteroids as directed.
- Non-Pharmacological Techniques: Suggest use of warm compresses over the sinuses, relaxation techniques, and avoidance of triggers that worsen pain.
3. Infection Prevention
- Hand Hygiene: Educate patient about frequent handwashing to prevent spread or introduction of infections.
- Avoidance of Irritants: Counsel patient to avoid exposure to environmental irritants such as smoke, strong odors, and allergens.
- Medication Adherence: Reinforce the importance of completing prescribed antibiotics or antifungal therapy, if indicated.
- Recognizing Signs of Secondary Infection: Teach patients to recognize and promptly report increased fever, severe headache, vision changes, or swelling around the eyes.
4. Patient Education
- Understanding the Condition: Provide information on the chronic nature of sinusitis, triggers, and the importance of ongoing management.
- Medication Use: Instruct patient on the proper administration of nasal sprays, antibiotics, corticosteroids, and other prescribed medications.
- Nasal Care Techniques: Demonstrate safe and hygienic nasal irrigation methods, stressing the use of sterile or distilled water.
- Lifestyle Modifications: Advise on strategies to avoid known triggers, such as using air purifiers, controlling indoor humidity, and limiting exposure to allergens.
- Follow-Up Care: Emphasize the importance of regular follow-up visits to monitor progress and manage recurrent or persistent symptoms.
5. Addressing Sleep Disturbance
- Encourage Regular Sleep Patterns: Suggest a consistent bedtime routine to promote restful sleep.
- Reducing Nasal Congestion at Night: Advise on use of humidifiers, elevated head positioning, and avoidance of late-night allergens.
- Pain and Symptom Control: Ensure pain and congestion are managed effectively prior to sleep.
6. Psychological and Emotional Support
- Active Listening: Provide an empathetic ear to patient concerns about chronic symptoms and daily impact.
- Stress Reduction: Encourage stress management techniques, such as deep breathing, gentle exercise, or counseling.
- Support Groups: Provide resources or referrals to local or online support groups for patients with chronic sinus issues.
Collaborative Care
Nurses work as part of a multidisciplinary team, collaborating with physicians, allergists, ENT specialists, pharmacists, and other allied health professionals. Coordination may include:
- Referral for allergy testing if atopy is suspected.
- Preparation for surgical interventions such as functional endoscopic sinus surgery (FESS) in refractory cases.
- Coordinating with dietitians for nutritional advice if allergies or intolerances are involved.
Monitoring and Evaluation
Regular evaluation of the patient’s progress is essential. Nurses should monitor:
- Symptom improvement or worsening.
- Adherence to medication and home care routines.
- Occurrence of complications, such as orbital cellulitis or meningitis.
- Patient understanding of their condition and confidence in self-management.
Discharge Planning and Home Care
Before discharge, ensure the patient and family are well-informed about ongoing care:
- Provide written and verbal instructions for sinus care at home.
- Review warning signs that require urgent medical attention.
- Arrange follow-up appointments and discuss how to access additional support if needed.
REFERENCES
- Holbrook EH. Chronic rhinosinusitis: Clinical manifestations, pathophysiology, and diagnosis. Chronic rhinosinusitis: Clinical manifestations, pathophysiology, and diagnosis – UpToDate
- ENThealth. Sinusitis. https://www.enthealth.org/conditions/sinusitis/. Updated 8/2018
- Bennett JE, et al., eds. Sinusitis. In: Mandell, Douglas, and Bennett’s Principles and Practice of Infectious Diseases. 9th ed. Elsevier; 2020. https://www.clinicalkey.com.
- JAMA Network. Adult Chronic Sinusitis. https://jamanetwork.com/journals/jama/fullarticle/2432165. Updated 9/1/2015..
- Asthma and Allergy Foundation of America. Rhinitis (Nasal Allergies).. http://www.aafa.org/page/rhinitis-nasal-allergy-hayfever.aspx. Updated 10/2015.
- Hong P, Pereyra CA, Guo U, Breslin A, Melville L. Evaluating Complications of Chronic Sinusiti. http://downloads.hindawi.com/journals/criem/2017/8743828.pdf. Case Rep Emerg Med. 2017;2017:8743828.
- Fokkens WJ, et al. European position paper on rhinosinusitis and nasal polyps 2020. Rhinology. 2020; doi:10.4193/Rhin20.600.
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





