The lymphatic system is a vital, yet often underappreciated, component of human anatomy and physiology. For nurses, a thorough understanding of the lymphatic system is essential for effective patient care, especially in areas related to immunity, fluid balance, and disease management.
Introduction
Nursing practice demands a holistic grasp of the human body, with the lymphatic system playing a crucial role in maintaining health. The lymphatic system not only supports immune function but also facilitates fluid balance and the absorption of dietary fats. Nurses frequently encounter patients with lymphatic disorders, such as lymphedema, infections, or cancers like lymphoma.
Definition
The lymphatic system is a network of vessels, organs, and tissues responsible for transporting lymph—a clear, protein-rich fluid—throughout the body. It serves as a secondary circulatory system, complementing the cardiovascular system, and plays a pivotal role in immune defence and fluid regulation.
Historical Background
The study of the lymphatic system dates back to ancient times, with early descriptions found in the works of Hippocrates and Galen. However, it was not until the 17th century that Italian anatomist Gaspare Aselli discovered the lacteals (lymphatic vessels in the intestines), marking a significant advancement in understanding this system.
General Functions
- Maintaining fluid balance: Returns excess interstitial fluid to the bloodstream.
- Immune response: Filters pathogens and presents them to immune cells.
- Absorption of fats: Transports dietary lipids from the digestive tract to the blood.
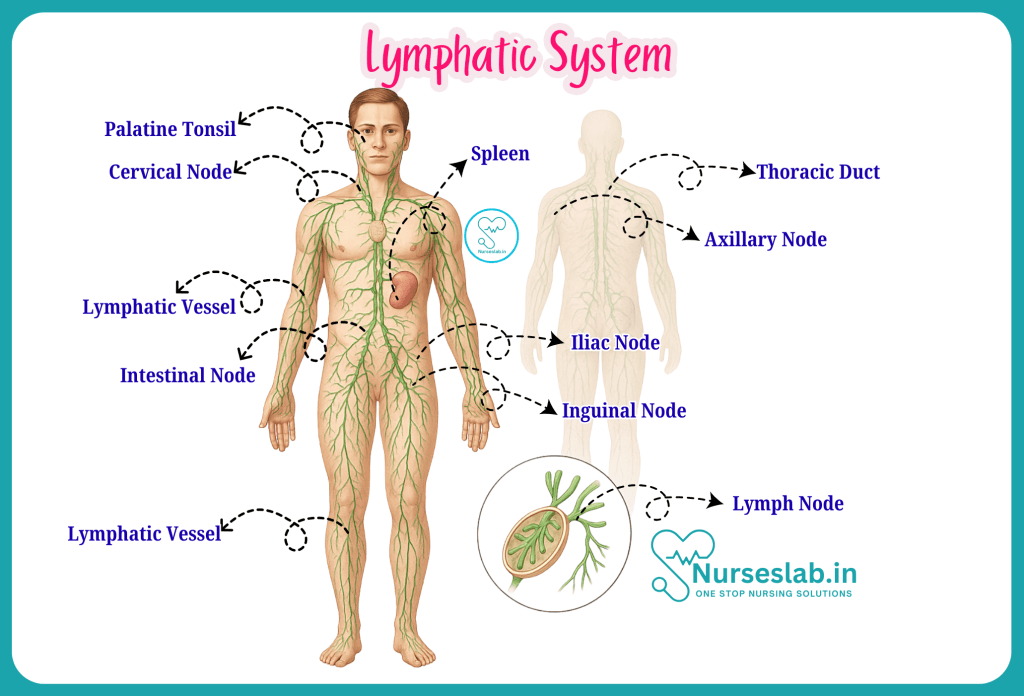
Anatomical Structures of the Lymphatic System
Lymphatic Vessels
Lymphatic vessels form an extensive network throughout the body, similar to blood vessels but distinct in structure and function. These vessels begin as microscopic capillaries in tissues, merging to form larger lymphatic vessels, and eventually draining into the circulatory system via lymphatic ducts.
Lymph
Lymph is a clear fluid derived from interstitial (tissue) fluid. It contains water, proteins, waste products, immune cells (mainly lymphocytes), and occasionally bacteria or foreign particles. Lymph acts as a transport medium for immune surveillance and waste removal.
Lymphatic Capillaries
Lymphatic capillaries are the smallest vessels, found near blood capillaries in most tissues. Their walls are thin and highly permeable, allowing the entry of large molecules and cells. This permeability is crucial for collecting excess tissue fluid and transporting immune cells.
Lymph Nodes
Lymph nodes are small, bean-shaped structures distributed along lymphatic vessels. They filter lymph, trapping pathogens, cancer cells, and debris. Each node contains lymphocytes and macrophages, which identify and destroy harmful substances. Common clusters of lymph nodes are found in the neck, armpits, groin, and abdomen.
Lymphatic Ducts
- Thoracic duct: The largest lymphatic vessel, draining lymph from most of the body into the left subclavian vein.
- Right lymphatic duct: Drains lymph from the right upper limb, right side of the thorax, and right side of the head and neck into the right subclavian vein.
Lymphatic Organs and Tissues
Thymus
Located in the upper chest, behind the sternum, the thymus is most active during childhood. It is essential for the development and maturation of T-lymphocytes (T-cells), which are critical for adaptive immunity. The thymus shrinks (involutes) after puberty but continues to produce immune cells throughout life.
Spleen
The spleen, situated in the upper left abdomen, functions as the largest lymphatic organ. It filters blood, removes old or damaged red blood cells, and stores platelets. The spleen also initiates immune responses to blood-borne pathogens and serves as a reservoir for white blood cells.
Tonsils
Tonsils are masses of lymphatic tissue located in the pharynx (throat). They act as the first line of defence against inhaled or ingested pathogens, containing immune cells that detect and respond to antigens entering through the mouth and nose.
Peyer’s Patches
Peyer’s patches are clusters of lymphoid tissue found in the lining of the small intestine, particularly the ileum. They monitor intestinal bacteria populations and contribute to the immune response against pathogens in the gut.
Bone Marrow
Bone marrow, found in the hollow centres of certain bones, is the primary site for the production of blood cells, including lymphocytes. It is a vital component of both the lymphatic and haematopoietic (blood-forming) systems.
Physiology and Functions of the Lymphatic System
Fluid Balance
The lymphatic system maintains fluid homeostasis by returning excess interstitial fluid to the bloodstream. Approximately 20 litres of plasma filter into tissues from capillaries daily; about 17 litres re-enter the blood directly, while 3 litres are returned via the lymphatic system. Without this return, tissues would swell (oedema), and blood volume would decrease.
Immune Response
Lymphatic organs and tissues are sites where immune responses are initiated. Lymph nodes filter out pathogens and present them to lymphocytes, which then mount an immune response. The thymus educates T-cells to distinguish between self and non-self, while the spleen responds to blood-borne antigens.
Absorption of Fats
Specialised lymphatic capillaries called lacteals, found in the small intestine, absorb dietary fats and fat-soluble vitamins. These nutrients are transported as chyle (a milky fluid) via the lymphatic system before entering the bloodstream.
Lymph Circulation Pathway
Flow of Lymph
Lymph begins as interstitial fluid collected by lymphatic capillaries. It then travels through progressively larger vessels and lymph nodes, eventually reaching the lymphatic ducts, which drain into the subclavian veins.
Mechanisms of Movement
- Muscle contraction: Skeletal muscle activity compresses lymphatic vessels, pushing lymph forward.
- Valves: One-way valves in lymphatic vessels prevent backflow, ensuring unidirectional movement.
- Respiratory movements: Changes in thoracic pressure during breathing facilitate lymph flow.
Drainage Areas
- Thoracic duct: Drains lymph from both lower limbs, abdomen, left thorax, left upper limb, and left side of the head and neck.
- Right lymphatic duct: Drains lymph from the right upper limb, right thorax, and right side of the head and neck.
Role in Immunity
Interaction with Immune Cells
Lymphatic tissues and organs are rich in lymphocytes (T-cells and B-cells) and macrophages. As lymph passes through the nodes, immune cells detect and destroy pathogens, abnormal cells, and foreign particles. The thymus and bone marrow are primary lymphoid organs responsible for the maturation of lymphocytes, while secondary organs (lymph nodes, spleen, tonsils, Peyer’s patches) provide sites for immune responses.
Defence Mechanisms
- Filtration: Lymph nodes act as filters, trapping bacteria, viruses, and debris.
- Antigen presentation: Dendritic cells and macrophages present antigens to lymphocytes, initiating adaptive immunity.
- Production of antibodies: B-cells, upon activation, differentiate into plasma cells that produce antibodies targeting specific pathogens.
Clinical Significance of the Lymphatic System
Importance in Disease
The lymphatic system is central to the body’s defence against infection and disease. It is also involved in the spread (metastasis) of cancers, especially those originating in lymphatic tissues. Lymph nodes are commonly assessed in clinical practice to detect infection, inflammation, or malignancy.
Infection and Inflammation
Lymph nodes often enlarge in response to infection (lymphadenopathy) as they filter pathogens and mount immune responses. The lymphatic system can also be a route for the spread of infections, such as in cellulitis or tuberculosis.
Cancer Metastasis
Many cancers, including breast and prostate cancer, spread via the lymphatic system. The presence of cancer cells in lymph nodes often influences staging, prognosis, and treatment decisions.
Common Disorders of the Lymphatic System
Lymphedema
Lymphedema is the swelling of tissues due to impaired lymphatic drainage. It may be congenital (primary) or secondary to surgery, radiation, infection, or trauma. Commonly seen after lymph node removal in cancer treatment, lymphedema can significantly impact quality of life, requiring ongoing management.
Lymphadenopathy
Lymphadenopathy refers to the abnormal enlargement of lymph nodes. Causes include infections (viral, bacterial, fungal), immune disorders (such as lupus), and malignancies (such as lymphoma or metastatic cancer). Assessment of lymph node size, consistency, and tenderness provides valuable diagnostic information.
Lymphoma
Lymphoma is a group of cancers arising from lymphocytes. The two main types are Hodgkin lymphoma and non-Hodgkin lymphoma. Symptoms include painless lymph node swelling, fever, night sweats, and weight loss. Diagnosis involves biopsy, imaging, and laboratory tests; treatment may include chemotherapy, radiotherapy, or stem cell transplantation.
Infections
The lymphatic system may be involved in various infections, such as:
- Lymphangitis: Inflammation of lymphatic vessels, often due to bacterial infection. Presents as red streaks on the skin, fever, and tenderness.
- Filariasis: Parasitic infection causing severe lymphedema, prevalent in tropical regions.
Nursing Considerations
Assessment
- Palpation of lymph nodes for size, tenderness, and mobility.
- Observation for signs of lymphedema (swelling, skin changes).
- Monitoring for symptoms such as fever, night sweats, or unexplained weight loss.
- Assessment of wound healing and risk of infection in patients with lymphatic impairment.
Patient Education
- Instruct patients on the importance of limb care to prevent lymphedema, especially after lymph node removal.
- Educate about early signs of infection and the need for prompt medical attention.
- Promote strategies for infection prevention, such as skin hygiene and avoiding injuries.
Care Implications
- Implement compression therapy and physiotherapy for lymphedema management.
- Coordinate with multidisciplinary teams for comprehensive care in lymphoma or metastatic cancer.
- Provide psychological support for patients coping with chronic lymphatic disorders.
REFERENCES
- Ross and Wilson, Anatomy and Physiology in Health and Illness, Fourteenth Edition, 1 July 2022, ISBN-13: 978-0323834612.
- Roger Watson, Anatomy and Physiology for Nurses, 14th Edition, 12-06-2018, ISBN: 9780702077418
- P.R Asha Latha, Text Book of Applied Anatomy & Physiology for Nurses, 7th Edition,3 January 2024, ISBN-13: 978-9356968622.
- Bryan H. Derikson, Tortora’s Principles of Anatomy and Physiology, 16th Edition, August 2023, ISBN: 978- 1119400066.
- Standring S, ed. Gray’s Anatomy: The Anatomical Basis of Clinical Practice. 42nd ed. London: Elsevier; 2020. pp. 75–102. ISBN 978-0702077050.
- Rohen JW, Yokochi C, Lutjen-Drecoll E. Color Atlas of Anatomy: A Photographic Study of the Human Body. 9th ed. Philadelphia: Lippincott Williams & Wilkins; 2021. pp. 14–34. ISBN 978-1975151346.
- Anatomy.co.uk, Lymphatic System, Last updated on April 24, 2025, https://anatomy.co.uk/lymphatic-system
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.