Explore the stages of wound healing: from clot formation and immune response to tissue regeneration and scar remodeling. Understanding hemostasis, inflammation, proliferation, and maturation phases is key to promoting recovery, preventing complications, and optimizing wound care in clinical and surgical settings.
Introduction
Wound healing is a vital process in clinical practice and a cornerstone of nursing care. Effective wound management not only prevents complications but also restores patient health and quality of life. For nurses, a robust understanding of the pathology and genetics underlying wound healing is essential, enabling evidence-based interventions and holistic patient care. Integrating perspectives from pathology and genetics offers a deeper comprehension of why wounds heal differently in individuals and how personalised approaches can optimise outcomes.
Basics of Wound Healing
Definition and Types of Wounds
A wound is defined as a disruption of the normal anatomical structure and function of the skin or underlying tissues. Wounds may result from trauma, surgery, burns, or disease processes. They are broadly classified as:
- Acute wounds: Typically follow a predictable course of healing, such as surgical incisions or accidental cuts.
- Chronic wounds: Fail to progress through the normal stages of healing, often persisting for weeks or months. Examples include pressure ulcers, diabetic foot ulcers, and venous leg ulcers.
Understanding the type of wound is crucial for selecting appropriate interventions and predicting healing trajectories.
Physiological Stages of Wound Healing
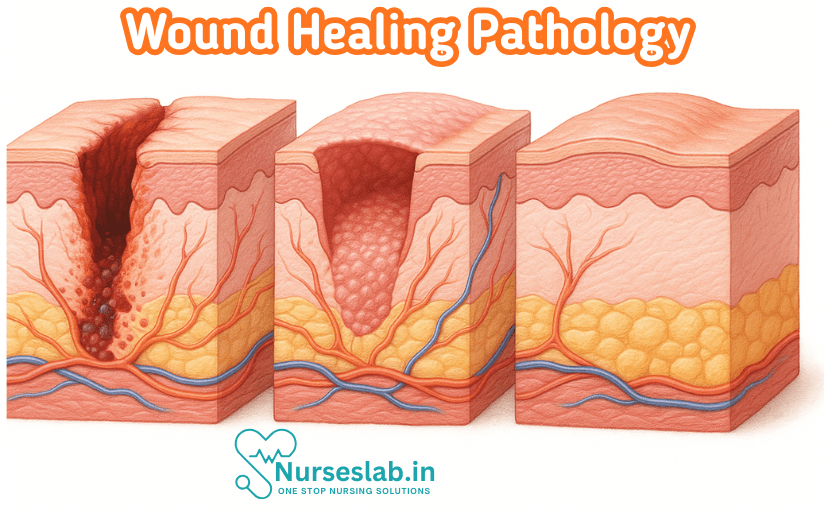
Wound healing is a complex, coordinated process comprising four overlapping stages:
- Hemostasis: Immediately following injury, blood vessels constrict to minimise blood loss. Platelets aggregate and form a clot, providing a temporary matrix for cell migration.
- Inflammation: Within hours, vasodilation occurs, and immune cells (neutrophils, macrophages) migrate to the site. They clear debris, pathogens, and release cytokines that orchestrate subsequent healing events.
- Proliferation: New tissue forms through angiogenesis (development of new blood vessels), fibroblast proliferation, collagen deposition, and epithelialisation. Granulation tissue fills the wound bed, and the wound contracts.
- Remodeling: Over weeks to months, collagen fibres are reorganised, and the wound gains tensile strength. Scar tissue matures, although it rarely achieves the full strength of uninjured skin.
Each stage is regulated by a cascade of cellular and molecular signals, and disruption at any point can impair healing.
Pathological Aspects of Wound Healing
Factors Affecting Wound Healing
Several pathological factors can influence the efficiency and outcome of wound healing:
- Infection: Microbial contamination impedes healing by prolonging inflammation and tissue destruction. Nurses play a pivotal role in infection prevention through aseptic techniques and wound surveillance.
- Chronic Diseases: Conditions such as diabetes mellitus, vascular disease, and immunosuppression compromise healing by impairing blood flow, nutrient delivery, and immune response.
- Nutrition: Adequate protein, vitamins (especially C and A), and minerals (zinc, iron) are essential for cellular repair, collagen synthesis, and immune function. Malnutrition delays healing and increases susceptibility to infection.
- Age: Elderly patients often experience slower healing due to reduced cellular activity, comorbidities, and diminished skin integrity.
- Medications: Corticosteroids, cytotoxic drugs, and anticoagulants can interfere with various stages of healing.
Complications in Wound Healing
Pathological influences can lead to complications such as:
- Delayed Healing: Prolonged inflammatory phase, persistent infection, or inadequate blood supply can stall healing.
- Chronic Wounds: Non-healing wounds may result from repeated trauma, pressure, or underlying disease, requiring specialist management.
- Dehiscence: Premature separation of wound edges, often seen post-operatively, may be due to infection or mechanical stress.
- Excessive Scarring: Hypertrophic scars or keloids develop from abnormal collagen deposition, more common in genetically predisposed individuals.
Recognising and addressing these complications is a critical aspect of nursing care.
Genetic Influences on Wound Healing
Role of Genetics in Tissue Repair
Genetic factors play a significant role in determining the speed, quality, and outcome of wound healing. Genes regulate the production of growth factors, cytokines, collagen, and enzymes involved in tissue repair. Variations in these genes can affect cellular migration, proliferation, and matrix remodelling, influencing individual healing responses.
Genetic Disorders Affecting Wound Healing
- Ehlers-Danlos Syndrome (EDS): A group of inheritable connective tissue disorders marked by defective collagen synthesis, leading to fragile skin, poor wound healing, and abnormal scarring.
- Marfan Syndrome: Another connective tissue disorder affecting skin elasticity and wound tensile strength.
- Genetic Variants: Single nucleotide polymorphisms (SNPs) in genes encoding for growth factors (e.g., VEGF, TGF-β) influence angiogenesis and repair processes.
Nurses should be aware of these disorders, as patients may require tailored wound care and multidisciplinary management.
Molecular Mechanisms
At the molecular level, wound healing involves gene expression changes that drive cell activation, migration, and proliferation. Key molecules include:
- Growth Factors: Platelet-derived growth factor (PDGF), transforming growth factor-beta (TGF-β), and vascular endothelial growth factor (VEGF) stimulate cell division and new tissue formation.
- Matrix Metalloproteinases (MMPs): Enzymes that remodel extracellular matrix, regulated by genetic and environmental factors.
- Cytokines: Interleukins and tumour necrosis factor-alpha (TNF-α) mediate inflammation and cellular communication.
Genetic mutations or dysregulation of these molecules can manifest as impaired wound healing or abnormal scarring.
Clinical Implications: Assessment and Diagnosis
Thorough assessment is the foundation of effective wound management. Nurses should evaluate:
- Wound type, location, size, and depth
- Presence of infection, necrosis, or foreign bodies
- Patient’s medical history, including chronic diseases and genetic predispositions
- Nutritional status and medication use
- Signs of delayed healing or complications
Diagnostic tools may include wound swabs for microbiology, blood tests for nutritional markers, and genetic screening in select cases. Understanding how pathology and genetics influence healing guides the development of personalised treatment plans.
Nursing Interventions
Evidence-Based Wound Care
Nurses are at the forefront of wound care, employing interventions grounded in current research and best practice guidelines:
- Cleansing and Debridement: Removal of dead tissue and debris promotes healthy granulation and reduces infection risk.
- Dressing Selection: Choice depends on wound type, exudate level, and underlying pathology. Advanced dressings (hydrocolloid, alginate, foam) may be used for chronic wounds.
- Moist Wound Healing: Maintaining an optimal moisture balance accelerates healing and minimises pain.
- Infection Control: Use of antiseptics, antibiotics, and strict aseptic technique.
- Pressure Relief: Positioning and use of support surfaces to prevent pressure ulcers.
Patient Education
Empowering patients with knowledge about wound care is essential. Nurses should educate on:
- Importance of nutrition and hydration
- Signs of infection or delayed healing
- Medication adherence and wound care techniques
- Lifestyle modifications to support healing
Monitoring and Documentation
Regular monitoring and meticulous documentation are critical for tracking progress, identifying complications, and facilitating communication among the healthcare team. Nurses should record wound measurements, appearance, interventions, and patient responses.
Case Studies
Case 1: Diabetic Foot Ulcer
A 55-year-old male with poorly controlled diabetes presents with a non-healing foot ulcer. Assessment reveals neuropathy, poor peripheral circulation, and signs of infection. Pathological factors (chronic disease, infection) and possible genetic predisposition to poor healing are considered. Nursing interventions include wound debridement, infection control, pressure offloading, and patient education on glycaemic control. Multidisciplinary collaboration with endocrinology and podiatry is essential.
Case 2: Ehlers-Danlos Syndrome
A young female with Ehlers-Danlos syndrome undergoes elective surgery. Postoperatively, she experiences wound dehiscence and delayed healing. Her genetic condition necessitates gentle wound handling, specialised dressings, and close monitoring. Collaboration with genetics specialists and physiotherapists ensures optimal recovery.
Case 3: Elderly Patient with Venous Leg Ulcer
An 80-year-old woman develops a chronic venous leg ulcer. Contributing factors include advanced age, poor mobility, and nutritional deficiencies. Pathological and age-related influences are addressed through compression therapy, nutritional support, and regular wound assessment. Patient education focuses on mobility exercises and skin care.
Future Directions
Advances in Genetic Research
Genetic research is rapidly expanding our understanding of wound healing. Identification of gene variants associated with impaired healing is paving the way for targeted therapies and personalised wound care. Technologies such as gene editing and stem cell therapy hold promise for enhancing tissue repair in patients with genetic disorders.
Personalised Medicine in Wound Care
Personalised medicine involves tailoring treatment to the individual’s genetic and pathological profile. In wound care, this may include genetic screening for risk assessment, customising interventions based on molecular markers, and the development of novel therapeutics. Nurses must stay abreast of emerging evidence to integrate these advances into practice.
Conclusion
Wound healing is a multifaceted process influenced by pathological and genetic factors. A sound understanding of these dynamics enables nurses to deliver comprehensive, patient-centred care, anticipate complications, and adopt evidence-based interventions. As genetic research and personalised medicine evolve, nurses will play an increasingly critical role in translating scientific advances into improved patient outcomes. By fostering continual learning and interdisciplinary collaboration, the nursing profession can remain at the forefront of wound care excellence.
In summary, wound healing demands an integrated approach that considers both pathology and genetics. The implications for nursing practice are profound, requiring skill, knowledge, and compassion to support patients through every stage of recovery.
REFERENCES
- Ramadas Nayak, Textbook of Pathology and Genetics for Nurses, 2nd Edition,2024, Jaypee Publishers, ISBN: 978-93-5270-031-8.
- Suresh Sharma, Textbook of Pharmacology, Pathology & Genetics for Nurses II, 2nd Edition, 31 August 2022, Jaypee Publishers, ISBN: 978-9354655692.
- Kumar, V., Abbas, A.K., & Aster, J.C. (2020). Robbins and Cotran Pathologic Basis of Disease. 10th Edition. Elsevier.
- McCance, K.L., & Huether, S.E. (2018). Pathophysiology: The Biologic Basis for Disease in Adults and Children. 8th Edition. Elsevier.
- Wilkinson HN, Hardman MJ. Wound healing: cellular mechanisms and pathological outcomes. Open Biol. 2020 Sep;10(9):200223.
- Vachhrajani, V., Khakhkhar, P. (2020). Pathophysiology of Wound Healing. In: Science of Wound Healing and Dressing Materials. Springer, Singapore. https://doi.org/10.1007/978-981-32-9236-9_2
- Mills, Stuart & Hofma, Ben & Cowin, Allison. (2020). Pathophysiology of Wound Healing. 10.1007/978-3-030-43683-4_25.
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





