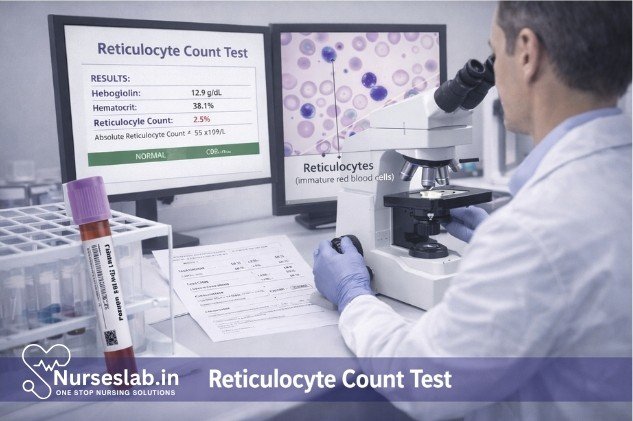
A reticulocyte count evaluates the number of immature red blood cells in circulation, helping assess bone marrow function, anemia types, and response to therapy. It is essential in hematology, diagnostics, and clinical decision‑making.
Introduction
The reticulocyte count is a fundamental haematological test that provides valuable information regarding erythropoiesis—the process of red blood cell (RBC) production—in the bone marrow. By quantifying the number of reticulocytes, which are immature RBCs recently released from the marrow, clinicians can assess the marrow’s response to anaemia, evaluate bone marrow function, and monitor the effectiveness of therapy in various haematological disorders. pretation, potential errors, and clinical applications.
Definition and Physiology
What Are Reticulocytes?
Reticulocytes are young, non-nucleated erythrocytes that still contain remnants of ribosomal RNA, which appear as reticular (network-like) material when stained with specific dyes. They represent the transitional stage between nucleated erythroid precursors in the bone marrow and mature erythrocytes circulating in the peripheral blood.
Role in Erythropoiesis
Erythropoiesis is the process through which new RBCs are produced. Reticulocytes are released from the bone marrow into the bloodstream, where they mature into erythrocytes within 1–2 days. The presence and quantity of reticulocytes reflect the bone marrow’s capacity to produce and release RBCs in response to physiological demands or pathological conditions.
Clinical Significance
The reticulocyte count serves as a direct indicator of bone marrow activity and erythropoietic response. It is particularly useful in distinguishing between different types of anaemia and in monitoring the regenerative capacity of the marrow after therapeutic interventions. A high reticulocyte count typically signifies a robust marrow response, whereas a low count indicates inadequate production or failure of erythropoiesis.
Indications for Reticulocyte Count
The reticulocyte count is ordered in various clinical scenarios, including:
- Evaluation of unexplained anaemia
- Assessment of bone marrow recovery after chemotherapy, radiotherapy, or bone marrow transplantation
- Monitoring response to treatment in patients with nutritional or haemolytic anaemias
- Distinguishing between hypoproliferative and hyperproliferative anaemias
- Investigation of suspected haemolytic disorders
- Assessment of erythropoietic activity in chronic kidney disease and other marrow-suppressive conditions
Sample Collection
Blood Sample Requirements
A peripheral venous blood sample is required for the reticulocyte count. The sample is usually collected in an ethylenediaminetetraacetic acid (EDTA) anticoagulated tube to prevent clotting.
Precautions
- Ensure proper mixing of the blood sample with the anticoagulant to avoid clot formation.
- Process the sample promptly, preferably within 6 hours of collection, to prevent artefactual changes in reticulocyte morphology or count.
- Avoid haemolysed or clotted samples, as these may yield inaccurate results.
Laboratory Methods
Manual Techniques
Traditionally, the reticulocyte count was performed manually using supravital stains such as new methylene blue or brilliant cresyl blue. The procedure involves mixing an aliquot of blood with the stain, incubating for a specified period, and preparing a blood smear. Reticulocytes are then identified under a microscope by their characteristic reticular network of RNA.
- Staining Procedure: Mix equal parts of blood and supravital stain, incubate at room temperature (25–30°C) for 10–15 minutes, prepare a thin smear, and examine under oil immersion (1000x magnification).
- Counting: Count the number of reticulocytes per 1000 RBCs in multiple fields and calculate the percentage.
Automated Techniques
Modern laboratories predominantly use automated haematology analysers equipped with flow cytometry capabilities for reticulocyte enumeration. These instruments employ fluorescent dyes that bind to RNA, allowing precise and rapid quantification of reticulocytes, and often provide additional parameters such as immature reticulocyte fraction (IRF) and mean reticulocyte volume (MRV).
- Advantages: Enhanced accuracy, reduced observer bias, ability to analyse large numbers of cells, and provision of additional indices.
- Limitations: Cost, maintenance requirements, and need for technical expertise.
Calculation and Reporting
The reticulocyte count is typically reported as a percentage of total RBCs or as an absolute count (reticulocytes per microlitre of blood). The calculation involves the following steps:
- Manual Count:
- Reticulocyte % = (Number of reticulocytes / Number of RBCs counted) × 100
- Absolute Reticulocyte Count:
- Absolute reticulocyte count = Reticulocyte % × RBC count (in millions/μL) × 10
- Corrected Reticulocyte Count:
- Corrected reticulocyte % = Reticulocyte % × (Patient’s haematocrit / Normal haematocrit)
- Reticulocyte Production Index (RPI):
- RPI = Corrected reticulocyte % / Maturation time (in days, depending on haematocrit level)
Automated analysers typically provide both percentage and absolute counts, along with additional indices relevant to clinical interpretation.
Interpretation of Results
Normal Ranges
- Reticulocyte percentage (adults): 0.5% – 2.5% of total RBCs
- Absolute reticulocyte count: 25,000 – 100,000/μL
- Reference ranges may vary by laboratory and patient age
High Reticulocyte Count (Reticulocytosis)
An elevated reticulocyte count suggests increased erythropoietic activity, commonly seen in:
- Haemolytic anaemias (autoimmune, hereditary spherocytosis, G6PD deficiency, etc.)
- Acute or chronic blood loss
- Response to treatment for nutritional anaemias (iron, vitamin B12, folate)
- Following bone marrow recovery post-chemotherapy or transplantation
Low Reticulocyte Count (Reticulocytopenia)
A decreased reticulocyte count indicates inadequate marrow production or suppression, as seen in:
- Aplastic anaemia
- Marrow infiltration (leukaemia, metastatic cancer)
- Chronic renal failure (due to erythropoietin deficiency)
- Iron, vitamin B12, or folate deficiency (prior to therapy initiation)
- Chronic infections or inflammatory states
Clinical Implications
Interpretation must consider the clinical context, patient’s haematocrit, and absolute reticulocyte count. A high reticulocyte count in anaemia suggests a regenerative process, whereas a low count points towards hypoproliferative anaemia or marrow failure. The reticulocyte production index (RPI) further refines interpretation by correcting for premature reticulocyte release in severe anaemia.
Sources of Error
Pre-analytical Errors
- Incorrect sample collection or handling (e.g., delayed processing, haemolysis, clotting)
- Improper anticoagulant use
- Inadequate mixing, leading to non-representative samples
Analytical Errors
- Poor staining technique or use of expired reagents in manual methods
- Observer bias and inter-observer variability in manual counting
- Instrument calibration errors or technical faults in automated analysers
- Presence of Howell-Jolly bodies, Heinz bodies, or other inclusions mimicking reticulocytes
Post-analytical Errors
- Incorrect calculation or transcription of results
- Failure to adjust for haematocrit in cases of anaemia
- Misinterpretation due to lack of clinical correlation
Clinical Applications
The reticulocyte count has diverse clinical applications, including:
- Diagnosis of Anaemia: Differentiates between hypoproliferative (e.g., aplastic) and hyperproliferative (e.g., haemolytic) anaemias.
- Monitoring Therapy: Assesses response to treatment in iron, vitamin B12, or folate deficiency, and in haemolytic anaemias.
- Bone Marrow Function: Evaluates marrow recovery post-chemotherapy, transplantation, or after acute blood loss.
- Assessment of Erythropoietic Activity: Monitors the effect of erythropoiesis-stimulating agents in chronic kidney disease.
- Prognostication: Helps in predicting outcomes in marrow failure syndromes and in monitoring disease progression or remission.
Limitations
Although invaluable, the reticulocyte count has certain limitations:
- May be falsely elevated in the presence of artefacts or interfering substances (e.g., high white cell count, hyperbilirubinaemia)
- Manual methods are labour-intensive and subject to observer bias
- Requires adjustment for haematocrit in anaemic patients for meaningful interpretation
- Automated analysers, though more accurate, may not be universally available, especially in resource-limited settings
- Does not provide information about the cause of anaemia; must be interpreted alongside clinical and laboratory data
Nursing Care of Patients Undergoing Reticulocyte Count Procedure
This procedure provides vital information about bone marrow function and erythropoietic activity, helping to diagnose and monitor conditions such as anemia, bone marrow disorders, and response to therapy. Nurses play a crucial role in ensuring the accuracy of the procedure, patient safety, and the delivery of holistic care throughout the process.
Pre-Procedure Nursing Responsibilities
1. Patient Assessment
The nurse should begin with a thorough assessment of the patient, including:
- Reviewing the patient’s medical history, especially for hematologic disorders, recent transfusions, or ongoing therapies that may affect erythropoiesis.
- Assessing for signs and symptoms of anemia (fatigue, pallor, tachycardia, shortness of breath), bleeding, or infection.
- Checking the patient’s medication list for drugs that may affect reticulocyte production or interfere with the test results.
2. Patient Education
Clear communication is vital to alleviate anxiety and ensure cooperation. The nurse should:
- Explain the purpose of the reticulocyte count and how it helps guide diagnosis and treatment.
- Describe the procedure, including the blood sample collection, expected sensations (e.g., slight discomfort from venipuncture), and the duration (usually a few minutes).
- Inform the patient about any preparation needed, such as fasting (usually not required for this test), and advise on the continuation of regular medications unless otherwise instructed by the physician.
- Address any questions or concerns, emphasizing the safety and routine nature of the procedure.
3. Preparation of Equipment and Environment
- Ensure all necessary supplies are available: tourniquet, sterile needles, syringes or vacutainers, antiseptic swabs, gauze, adhesive bandages, specimen tubes (with appropriate anticoagulant, often EDTA), gloves, and labels.
- Verify patient identity using at least two identifiers (e.g., name and date of birth).
- Prepare the blood specimen request form, ensuring all details are accurate and complete.
- Prepare a clean, well-lit workspace to minimize the risk of contamination and errors.
During the Procedure: Nursing Care
1. Infection Control and Safety
- Perform hand hygiene before and after the procedure.
- Wear gloves and follow standard precautions to prevent bloodborne pathogen exposure.
- Use sterile technique when handling needles and collecting blood samples.
2. Blood Sample Collection
The nurse should:
- Position the patient comfortably, ensuring the chosen vein (usually in the antecubital fossa) is accessible.
- Apply a tourniquet above the venipuncture site and select a suitable vein.
- Cleanse the site with an antiseptic swab and allow it to dry.
- Insert the needle smoothly to minimize discomfort and anxiety.
- Draw the required volume of blood into the appropriate tube, ensuring the correct anticoagulant is used.
- Remove the needle promptly, apply pressure with gauze to the puncture site, and secure with a bandage once bleeding stops.
- Label the specimen tube accurately at the bedside to prevent misidentification.
3. Patient Support and Monitoring
- Observe the patient for any signs of vasovagal reaction (dizziness, fainting, pallor, sweating) during or after the blood draw.
- Provide reassurance and emotional support, especially for anxious or needle-phobic patients.
- Monitor for complications such as hematoma formation, continued bleeding, or localized infection at the puncture site.
Post-Procedure Nursing Care
1. Specimen Handling and Documentation
- Ensure prompt and correct transport of the blood specimen to the laboratory to avoid cell deterioration and inaccurate results.
- Document the date and time of collection, the site used, any difficulties encountered, and the patient’s response to the procedure.
- Record any relevant observations (e.g., bleeding tendency, bruising, or fainting episodes) in the patient’s chart.
2. Patient Observation and Aftercare
- Check the puncture site for bleeding or hematoma after the procedure.
- Instruct the patient to keep the site clean and dry, and to report any unusual pain, swelling, or redness.
- Advise patients on anticoagulants or with bleeding disorders to apply pressure for a longer period and monitor for delayed bleeding.
3. Communication and Follow-Up
- Inform the patient when results are expected and who will discuss them.
- Report any abnormal findings (e.g., excessive bleeding, fainting) to the physician immediately.
- Arrange follow-up tests or appointments as indicated by the care plan.
Special Considerations
- Pediatric Patients: Use smaller gauge needles and provide age-appropriate explanations. Engage parents for support.
- Elderly Patients: Veins may be fragile; use gentle technique and monitor closely for hematoma formation.
- Patients with Bleeding Disorders: Take extra precautions to prevent and monitor for bleeding. Use pressure dressings as needed.
- Immunocompromised Patients: Maintain strict aseptic technique to prevent infection.
Interpretation of Results
While nurses do not interpret laboratory results independently, understanding the clinical significance of reticulocyte counts helps anticipate care needs and patient education:
- Increased Reticulocyte Count: May indicate active red cell production as seen in hemolytic anemia, acute blood loss, or response to therapy.
- Decreased Reticulocyte Count: Suggests bone marrow suppression or failure, as in aplastic anemia or untreated iron deficiency.
- False Results: Can occur due to delayed sample processing, improper anticoagulant, or specimen handling errors—highlighting the importance of nursing vigilance.
Patient Education and Counseling
Nurses are key educators for patients undergoing reticulocyte count procedures. Essential teaching points include:
- Purpose and importance of the test for their diagnosis and treatment monitoring.
- Reassurance about the safety and routine nature of blood sampling.
- Signs and symptoms to report after the procedure (e.g., excessive bleeding, bruising, infection).
- Information about follow-up appointments and continuity of care.
Documentation
Accurate and thorough documentation is an integral part of nursing care. Record the following:
- Date and time of specimen collection
- Site of venipuncture and any complications
- Patient’s tolerance of the procedure
- Instructions given to the patient
- Communication with the healthcare team regarding abnormal findings
REFERENCES
- American Society of Hematologists. Blood Basics https://www.hematology.org/education/patients/blood-basics.
- Gauer M, Sehgal T. Reticulocyte Count: A Simple Test But Tricky Interpretation. (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8490160/) Pan Afr Med J. 2021;40:3. 2021 Sep 2.
- Merck Manuals. Laboratory Tests for Blood Disorders https://www.merckmanuals.com/home/blood-disorders/symptoms-and-diagnosis-of-blood-disorders/laboratory-tests-for-blood-disorders?query=reticul.
- Neumours KidsHealth. Blood Test: Reticulocytes https://kidshealth.org/en/parents/reticulocyte.html.
- Gaur M, Sehgal T. Reticulocyte count: a simple test but tricky interpretation! Pan Afr Med J. 2021 Sep 2;40:3. doi: 10.11604/pamj.2021.40.3.31316. PMID: 34650653; PMCID: PMC8490160.
- Skverchinskaya E, Levdarovich N, Ivanov A, Mindukshev I, Bukatin A. Anticancer drugs paclitaxel, carboplatin, doxorubicin, and cyclophosphamide alter the biophysical characteristics of red blood cells, in vitro. Biology (Basel). 2023;12(2):230. doi:10.3390/biology12020230
- Rai D, Willson A, Moosavi L. Histology, Reticulocytes (https://www.ncbi.nlm.nih.gov/books/NBK542172/#_NBK542172_pubdet_). [Updated 2022 Feb. 17.] In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-.
- Froissart A, Rossi B, Ranque B, et al. Effect of a Red Blood Cell Transfusion on Biological Markers Used to Determine the Cause of Anemia: A Prospective Study. Am J Med. 2018;131(3):319-322. doi:10.1016/j.amjmed.2017.10.005
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





