Syndrome of inappropriate antidiuretic hormone (SIADH) occurs when the body releases excessive amounts of antidiuretic hormone (ADH), resulting in the retention of excess water in the body, causing hyponatremia.
ADH is a hormone produced by the hypothalamus and stored and released by the pituitary gland. It plays an essential role in various processes in the body, including the balance of salt and water in the blood, kidney function, and blood pressure regulation.
Causes of SIADH
Common causes of SIADH include the following:
- Medications
- Surgery under general anesthesia
- Stroke
- Brain injury
- Cancer
- Chronic infections
- Tuberculosis and other lung disorders
- Disorders affecting the hypothalamus and pituitary glands
- Substance abuse
Clinical manifestations of SIADH typically involve hyponatremia which causes nausea and vomiting, muscle cramps, muscle weakness, headache, problems with balance, mental changes, and seizures or coma in severe cases.
There is no single test that can diagnose SIADH. Physical examination and fluid status are assessed as they are integral in confirming the possibility of dehydration or overhydration. In addition, healthcare providers may order tests that can help confirm hyponatremia, such as a comprehensive metabolic panel, urine osmolality test, osmolality blood test, and urine sodium and potassium tests.
Nursing Process
Since different conditions may cause SIADH, its treatment will vary. However, the initial steps in the treatment process will be to limit fluid intake to prevent further accumulation of excess water in the body. Nurses are key in implementing strict fluid restrictions, fluid status monitoring, accurate patient education on the disease process, and treatment adherence.
Nursing Assessment
Effective nursing assessment and intervention are crucial in managing SIADH to prevent complications and promote patient well-being.
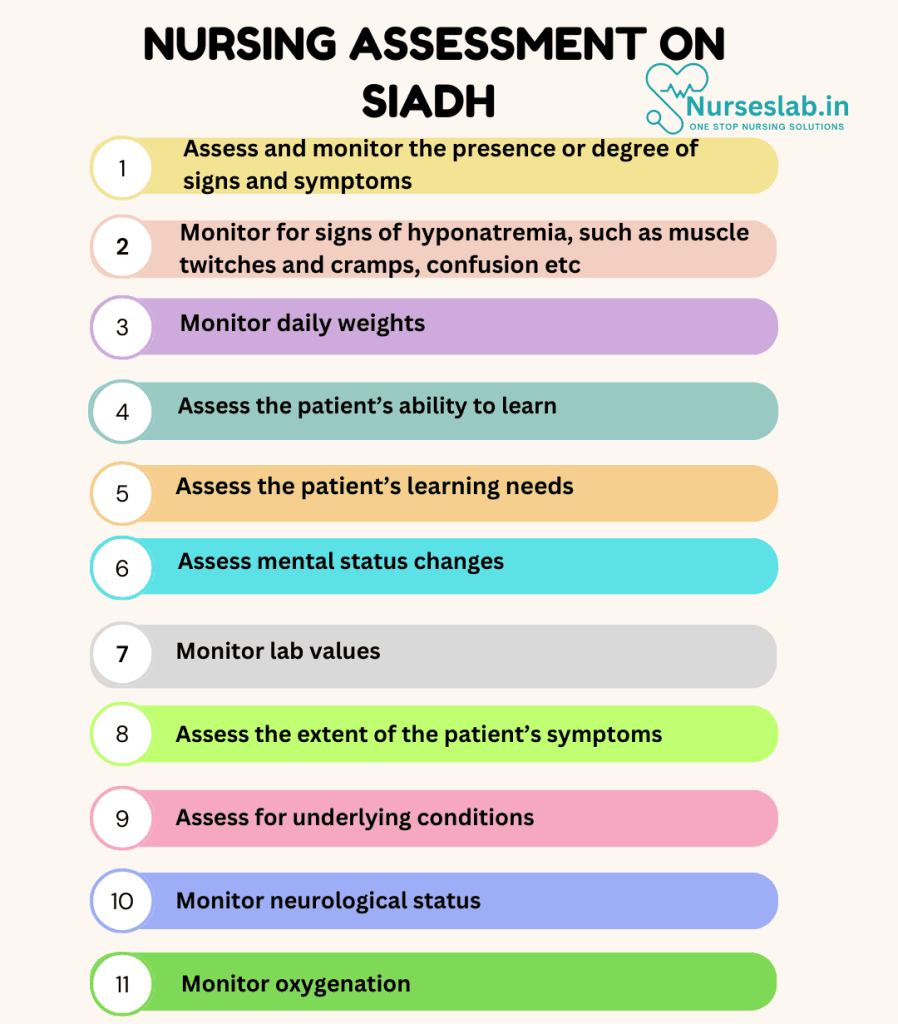
Initial Evaluation
The initial evaluation of a patient with suspected SIADH involves a thorough medical history and physical examination. Key aspects to assess include:
- Medical History: Review the patient’s history for risk factors such as recent surgeries, infections, or medications that may contribute to SIADH. Also, inquire about symptoms such as fatigue, headaches, nausea, and confusion, which are common in SIADH.
- Physical Examination: Perform a comprehensive physical examination focusing on signs of fluid retention, such as peripheral edema, weight gain, and decreased urine output.
- Laboratory Tests: Obtain baseline laboratory tests, including serum sodium, osmolality, urine sodium, and urine osmolality. Hyponatremia is a hallmark of SIADH, and these tests help confirm the diagnosis.
Ongoing Monitoring
Ongoing monitoring is essential to track the patient’s response to treatment and detect any potential complications. Nurses should:
- Vital Signs: Regularly monitor blood pressure, heart rate, and respiratory rate.
- Fluid Balance: Strictly monitor intake and output (I&O) to ensure appropriate fluid management.
- Neurological Status: Assess for changes in mental status, as hyponatremia can lead to confusion, seizures, and even coma.
- Laboratory Values: Continuously monitor serum sodium and osmolality levels to assess the effectiveness of interventions and adjust the treatment plan as needed.
Nursing Intervention
Dedication and expertise, nurses ensure that patients with SIADH receive comprehensive, compassionate, and person-centered care. By adopting a holistic approach, nurses can significantly impact the management of SIADH, helping patients achieve better control over their condition and ultimately reducing the risk of severe health complications. The synergy of thorough assessment, effective intervention, and continuous support underscores the vital role nurses play in managing this condition.
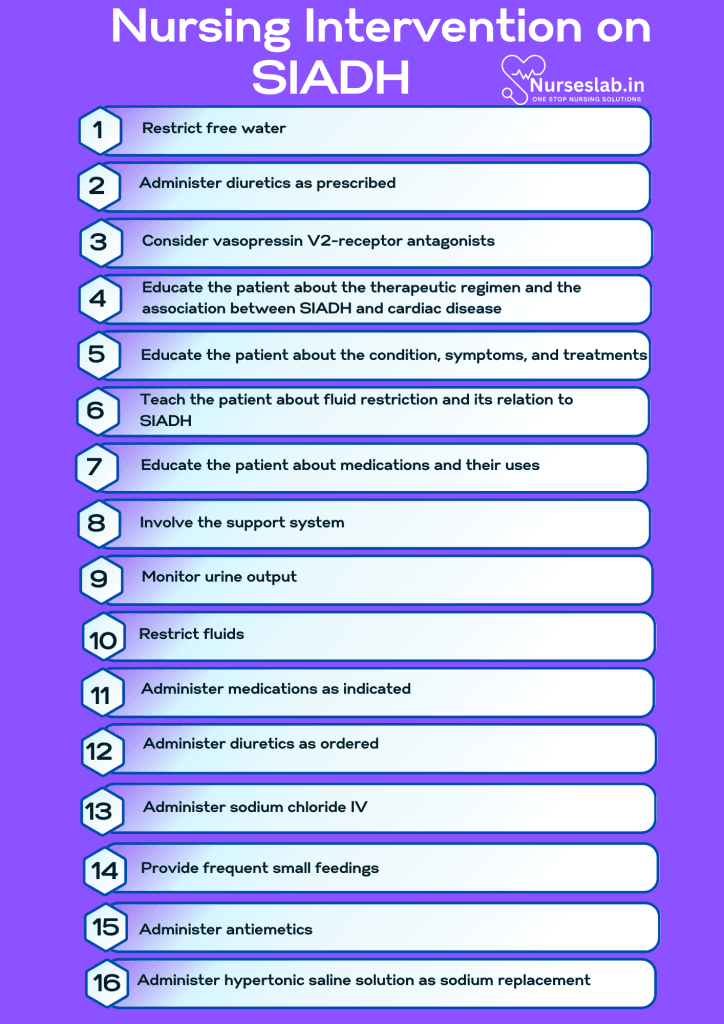
Fluid Restriction
Fluid restriction is a cornerstone of SIADH management. Nurses play a crucial role in educating patients about the importance of adhering to fluid restrictions and developing strategies to minimize discomfort and maintain compliance.
Medication Administration
Medications are often prescribed to manage SIADH and correct hyponatremia:
- Vasopressin Antagonists: These medications, such as tolvaptan, help block the effects of ADH and promote water excretion without significant loss of sodium.
- Diuretics: Loop diuretics may be used to promote urine output and manage fluid retention.
- Salt Tablets: In some cases, salt tablets may be prescribed to increase serum sodium levels.
Nurses are responsible for administering these medications, monitoring for adverse effects, and adjusting doses as necessary.
Electrolyte Management
Correcting electrolyte imbalances is critical in SIADH management. Nurses should:
- Administer Hypertonic Saline: In cases of severe hyponatremia, hypertonic saline may be administered under close monitoring to correct sodium levels safely.
- Monitor Electrolytes: Regularly monitor serum electrolytes, paying close attention to sodium and potassium levels, to ensure appropriate management and prevent complications.
Patient Education and Support
Educating patients about SIADH and providing support is essential for effective management. Nurses should:
- Provide Information: Educate patients about the causes, symptoms, and treatment of SIADH.
- Teach Self-Monitoring: Instruct patients on recognizing symptoms of hyponatremia and the importance of seeking medical attention if symptoms worsen.
- Discuss Medication Adherence: Emphasize the importance of adhering to prescribed medications and fluid restrictions.
- Address Concerns: Provide emotional support and address any concerns or anxieties the patient may have about their condition.
Nursing Care Plans
Once the nurse identifies nursing diagnoses for syndrome of inappropriate antidiuretic hormone, nursing care plans help prioritize assessments and interventions for both short and long-term goals of care. In the following section, you will find nursing care plan examples for syndrome of inappropriate antidiuretic hormone.
Decreased Cardiac Output
Inadequate blood is pumped by the heart due to the massive fluid overload caused by excessive vasopressin secretion.
Nursing Diagnosis: Decreased Cardiac Output
Related to:
- Increased antidiuretic hormone release
- Aggravating fluid overload
- Impaired contractility
- Increased ventricular filling
- Decreased myocardial oxygenation
- Increased myocardial oxygenation demand
As evidenced by:
- Shortness of breath
- Chest pain
- Palpitations
- Anorexia
- Fatigue
- Orthopnea
- Alteration in mentation
- Crackles
Expected outcomes:
- Patient will manifest adequate cardiac output as evidenced by the following:
- Blood pressure: Systolic BP >90 to <140; Diastolic BP >60 to <90
- Heart rate: 60 to 100 beats/min with a regular rhythm
- Respiratory rate: 12 to 20 breaths/min
- Strong peripheral pulses
- Absence of chest pain/discomfort
- Patient will not experience any changes in mentation.
- Patient will be normovolemic, as evidenced by the following:
- Urine output 0.5 to 1.5 cc/kg/hour
- Balanced intake and output
- Stable weight
- Maintained absence or reduction of edema
Assessment:
1. Assess and monitor the presence or degree of signs and symptoms such as:
- Exertional dyspnea
- Orthopnea
- Activity intolerance
- Paroxysmal nocturnal dyspnea
- Nocturnal cough
- Distended abdomen
- Fatigue
- Jugular vein distension
- Pulmonary rales
- S3 gallop
- Crackles
- Cool extremities
- Irregular heartbeat
These are signs and symptoms of heart failure and decreased cardiac output in which exertional dyspnea, activity intolerance, and orthopnea are the three most important symptoms.
2. Monitor for signs of hyponatremia, such as muscle twitches and cramps, confusion, nausea and vomiting, headache, etc.
In patients with congestive heart failure, there is an evident decrease in cardiac output and circulating volume, stimulating fluid and sodium retention. However, the uncontrolled release of AVP in SIADH promotes hyponatremia and aggravates the underlying cardiac dysfunction by causing systolic and diastolic myocardial wall stress and hypertrophy. Detection and early management of hyponatremia are crucial in managing concomitant heart disease.
3. Monitor daily weights.
Decreased cardiac output may lead to compromised regulatory mechanisms that result in fluid retention. A sudden weight gain of 2.2 lbs (1 kg) may indicate a liter of fluid retention. Patients with SIADH can retain 3 to 5 L. Monitoring body weight provides sensitive information on fluid balance.
Interventions:
1. Restrict free water.
Patients with heart failure and SIADH should restrict their water intake as first-line therapy. Guidelines recommend restricting water intake to 500-1500 mL/day.
2. Administer diuretics as prescribed.
Loop diuretics such as furosemide aid in eliminating excess water. Patients with heart failure and signs of fluid overload are treated with loop diuretics to reduce morbidity and mortality.
3. Consider vasopressin V2-receptor antagonists.
Tolvaptan is shown to be beneficial for patients with hyponatremia associated with CHF and SIADH. This medication is indicated for patients who are hypervolemic with less severe hyponatremia but who haven’t responded to fluid restriction.
4. Educate the patient about the therapeutic regimen and the association between SIADH and cardiac disease.
A thorough understanding of the therapeutic regimen and the nature of the disease aids in increasing adherence to the plan of care. Patients must understand the connection between fluid overload, sodium, symptoms, and cardiac workload.
Deficient Knowledge
Patient education is an essential part of the management of Syndrome of Inappropriate Antidiuretic Hormone to prevent complications and symptoms.
Nursing Diagnosis: Deficient Knowledge
Related to:
- Misinformation
- Inadequate access to resources
- Inadequate awareness of resources
- Inadequate commitment to learning
- Inadequate information
- Inadequate interest in learning
As evidenced by:
- Inaccurate follow-through of instructions
- Inaccurate statements about a topic
- Development of symptoms
- Worsening lab values
- Development of seizures or coma
Expected outcomes:
- Patient will verbalize an understanding of the disease, prognosis, and treatments.
- Patient will not develop preventable complications.
Assessment:
1. Assess the patient’s ability to learn.
Since SIADH is usually related to another cause (cancer, stroke, infection), ensure the patient is competent and capable of carrying out learned concepts.
2. Assess the patient’s learning needs.
It is important to determine the patient’s learning needs as this can help formulate the best approach to provide accurate information.
Interventions:
1. Educate the patient about the condition, symptoms, and treatments.
Provide accurate information about the condition, symptoms, and treatments in layperson’s terms that the patient can understand.
2. Teach the patient about fluid restriction and its relation to SIADH.
Fluid restriction is a priority in the management of SIADH, as the main issue with this disease is fluid excess and hyponatremia.
3. Educate the patient about medications and their uses.
Providing accurate information about medications and how they work as part of the SIADH treatment regimen to ensure better adherence.
4. Involve the support system.
The patient may require the assistance of a support person in managing this condition, monitoring for symptoms, and communicating with the healthcare team.
Excess Fluid Volume
Fluid volume excess is the main problem in patients with Syndrome of Inappropriate Antidiuretic Hormone.
Nursing Diagnosis: Excess Fluid Volume
Related to:
- Disease process
- Excessive fluid intake
- Compromised regulatory mechanism
- Endocrine regulatory dysfunction
- Renal dysfunction
As evidenced by:
- Intake exceeds output
- Concentrated urine
- Oliguria
- Low sodium levels
- Decreased hematocrit
Expected outcomes:
- Patient will maintain electrolytes within acceptable ranges.
- Patient will maintain balanced intake and output.
Assessment:
1. Assess mental status changes.
Low sodium can result in confusion, delirium, and seizures in severe causes, which can lead to coma and death. Subtle changes in mental status must be monitored for prompt intervention.
2. Monitor lab values.
SIADH primarily affects the patient’s ability to eliminate water effectively. This can cause low sodium levels, low serum osmolality, and alterations in kidney values.
Interventions:
1. Monitor urine output.
Urinalysis is often ordered to measure the patient’s urine concentration, sodium, and osmolality levels. Water retention may cause poor urine output.
2. Restrict fluids.
Fluid restriction is vital in SIADH as this can prevent further fluid retention in the body.
3. Administer medications as indicated.
Vasopressin antagonist medications like tolvaptan and conivaptan are given to block the action of ADH.
4. Administer diuretics as ordered.
Furosemide can be given to decrease urine concentration and increase water excretion.
Imbalanced Nutrition: Less than Body Requirements
Hyponatremia is a significant complication of Syndrome of Inappropriate Antidiuretic Hormone. This causes symptoms like cramping, loss of appetite, nausea, and vomiting. With frequent nausea and vomiting, imbalanced nutrition can occur.
Nursing Diagnosis: Imbalanced Nutrition
Related to:
- Food aversion
- Altered taste perception
- Nausea and vomiting
- Disease Process
- Misinformation
As evidenced by:
- Electrolyte imbalances
- Food intake less than recommended daily allowance
- Hypoglycemia
Expected outcomes:
- Patient will maintain laboratory values within expected limits.
- Patient will verbalize how their disease process affects nutrition.
Assessment:
1. Assess the extent of the patient’s symptoms.
Nausea and vomiting may occur with SIADH and can cause problems with nutrition. Vomiting is a serious symptom that can further worsen their condition.
2. Assess for underlying conditions.
SIADH is a complication of a condition. Cancers, lung diseases, brain injuries, and more can cause SIADH and may also affect intake and appetite.
Interventions:
1. Administer sodium chloride IV.
Though free water may be restricted to prevent fluid overload, IV sodium chloride may be ordered to treat hyponatremia.
2. Provide frequent small feedings.
This will help the patients stabilize blood sugar levels, improve satiety, and reduce the incidence of nausea and vomiting.
3. Administer salt tablets.
Especially if receiving diuretics, prescribed salt tablets can be administered to treat hyponatremia.
4. Administer antiemetics.
Vomiting is a concerning symptom related to SIADH that can worsen hyponatremia. The nurse can administer antiemetics to prevent further imbalance of electrolytes.
Ineffective Tissue Perfusion
Excessive ADH secretion leads to hyponatremia, affecting tissue and organ perfusion.
Nursing Diagnosis: Ineffective Tissue Perfusion
Related to:
- Impaired oxygen transport
- Compromised blood flow
- Hyper or hypovolemia
- Hyponatremia
- Insufficient knowledge of SIADH and its management
As evidenced by:
- Weak or absent peripheral pulses
- Numbness
- Muscle weakness
- Prolonged capillary refill
- Headache
- Seizures
- Change in level of consciousness
- Confusion
- Tremors
- Decreased reflexes
- Ataxia
- Coma
Expected outcomes:
- Patient will maintain optimal tissue perfusion as evidenced by the following:
- Strong, palpable pulses
- Absence of tremors or muscle weakness
- Capillary refill time of <2 secs
- Patient will not experience neurological complications such as seizures or coma.
Assessment:
1. Monitor neurological status:
- Headache
- Delirium
- Lethargy
- Restlessness
- Disorientation
- Depressed reflexes
- Seizures
- Dysarthria
Hyponatremia associated with SIADH causes cerebral edema through the osmotic movement of water from the extracellular compartment to the brain. Cerebral edema compromises cerebral tissue perfusion, leading to various neurologic signs and symptoms.
2. Monitor oxygenation.
Changes in oxygenation affect tissue perfusion. This is especially important to monitor in patients with decreasing neurologic status.
Interventions:
1. Do not correct hyponatremia rapidly.
Rapid correction of hyponatremia can result in permanent neurologic deficits. The goal is to raise sodium levels by 0.5-1 mEq/hour (not to exceed 10-12 mEq within 24 hours) to reach a maximum sodium level of 125-130 mEq/L.
2. Administer hypertonic saline solution as sodium replacement.
Hypertonic saline infusions are given for patients with neurological symptoms and severe hyponatremia (Na < 110 mEq/L).
3. Restrict fluids as ordered.
Restriction of fluid prevents further fluid overload and sodium dilution. This intervention alone may be adequate to correct hyponatremia.
4. Redraw sodium levels as ordered.
Close monitoring of sodium levels is warranted when correcting hyponatremia in SIADH.
Nursing Diagnoses and Rationales for Syndrome of Inappropriate Antidiuretic Hormone (SIADH)
1. Fluid Volume Excess
Rationale: SIADH results in excessive release of antidiuretic hormone, leading to water retention and dilutional hyponatremia. Monitoring fluid intake and output, daily weights, and assessing for signs of fluid overload (e.g., edema, crackles in lungs) are crucial. Implementing fluid restriction and administering diuretics as prescribed helps manage fluid balance.
2. Risk for Electrolyte Imbalance
Rationale: Dilutional hyponatremia due to water retention is a hallmark of SIADH. Regularly monitoring serum sodium levels and other electrolytes is essential. Educating patients on the importance of adhering to fluid restrictions and recognizing signs of electrolyte imbalances (e.g., confusion, muscle weakness) can prevent complications.
3. Risk for Confusion
Rationale: Hyponatremia can lead to neurological symptoms, including confusion, seizures, and coma. Monitoring the patient’s level of consciousness and cognitive function, and promptly addressing changes to prevent injury, is critical. Ensuring a safe environment and providing orientation cues can help manage confusion.
4. Imbalanced Nutrition: Less than Body Requirements
Rationale: Fluid retention and nausea associated with SIADH can reduce appetite and nutrient intake. Assessing dietary intake, monitoring weight, and providing nutritional support, such as nutrient-dense meals and supplements, are important. Collaborating with a dietitian to develop an individualized nutrition plan can improve patient outcomes.
5. Anxiety
Rationale: The diagnosis and management of SIADH can cause significant anxiety and distress. Providing psychological support, educating patients about the condition and its treatment, and involving them in care planning can help manage anxiety. Reassuring patients and addressing their concerns about symptoms and treatment can reduce stress.
6. Risk for Injury
Rationale: Hyponatremia-related confusion and muscle weakness increase the risk of falls and injuries. Implementing fall precautions, such as providing assistive devices and ensuring a clutter-free environment, is essential. Monitoring the patient’s mobility and strength, and providing interventions to prevent falls, can enhance safety.
REFERENCES
- Ackley, B.J., Ladwig, G.B.,& Makic, M.B.F. (2017). Nursing diagnosis handbook: An evidence-based guide to planning care (11th ed.). Elsevier.
- Abraham, W.T. (2008). Managing Hyponatremia in Heart Failure. US Cardiology, 5(1):57–60. https://doi.org/10.15420/usc.2008.5.1.57
- ACCN Essentials of Critical Care Nursing. 3rd Edition. Suzanne M. Burns, MSN, RRT, ACNP, CCRN, FAAN, FCCM, FAANP. 2014. McGraw Hill Education.
- Carpenito, L.J. (2013). Nursing diagnosis: Application to clinical practice (14th ed.). Lippincott Williams & Wilkins.
- Doenges, M.E., Moorhouse, M.F., & Murr, A.C. (2019). Nursing care plans: Guidelines for individualizing client care across the life span (10th ed.). F.A. Davis Company.
- Gulanick, M. & Myers, J.L. (2014). Nursing care plans: Diagnoses, interventions, and outcomes (8th ed.). Elsevier.
- Huxel, C., Raja, A.,& Ollivierre-Lawrence, M.D. (2022). Loop diuretics. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK546656/
- Malik, A., Brito, D., Vaqar, S., et al (2022). Congestive heart failure. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK430873/
- Medical-Surgical Nursing: Concepts for Interprofessional Collaborative Care. 9th Edition. Donna D. Ignatavicius, MS, RN, CNE, ANEF. 2018. Elsevier, Inc.
- Syndrome of Inappropriate Antidiuretic Hormone (SIADH). Ann Pietrangelo. Reviewed by Graham Rogers, M.D. Updated June 6, 2017. From: https://www.healthline.com/health/syndrome-of-inappropriate-antidiuretic-hormone
- Syndrome of Inappropriate Antidiuretic Hormone Secretion (SIADH). Children’s Hospital of Philadelphia. 2022. From: https://www.chop.edu/conditions-diseases/syndrome-inappropriate-antidiuretic-hormone-secretion-siadh
- Syndrome of inappropriate antidiuretic hormone secretion. Medline Plus Trusted Healthcare Information for You. Updated by Brent Wisse, MD, Board Certified in Metabolism/Endocrinology, Seattle, WA. Reviewed May 1, 2021. From: https://medlineplus.gov/ency/article/000314.htm
- Syndrome of Inappropriate Antidiuretic Hormone Secretion. Yasir M, Mechanic OJ. [Updated 2022 May 9]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507777/
- Thomas, C. P. (2023, July 12). Syndrome of Inappropriate Antidiuretic Hormone Secretion (SIADH) Treatment & Management: Approach Considerations, Emergent Care, Acute Setting. Medscape Reference. https://emedicine.medscape.com/article/246650-treatment#showall
- Yasir, M.& Mechanic, O.J. (2022). Syndrome of inappropriate antidiuretic hormone secretion. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK507777/
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.







