A nursing care plan on smoking includes assessment of tobacco use, readiness to quit, and respiratory status. Interventions focus on education, nicotine replacement, coping strategies, and support systems—promoting cessation and reducing health risks.
Introduction
Cigarette smoking, a leading cause of preventable death all over the world, affects nearly all organs in the body, results in various diseases, and reduces overall well-being.
Smoking can cause the following adverse health effects:
- Gum disease
- Vision problems
- Cancer development
- Persistent cough
- COPD
- Heart disease
- Angina
- Stroke
- Infertility
- Pregnancy complications
- Erectile dysfunction
- Weakened immune system
- Blood clots
- Premature skin aging
Tobacco, which is the primary material used in cigarettes, contains toxic substances including carbon dioxide, nicotine, and tar. Carbon dioxide is fatal when inhaled in large doses as it will decrease oxygen concentrations in the blood. Without oxygen, organs cannot function properly. Nicotine is a highly addictive substance in cigarettes that temporarily improves behavior and mood. Tar is a sticky brown substance that damages the lungs and causes breathing problems.
Nursing Process
Smoking cessation is difficult to achieve. Nurses play an important role in providing counseling and education on medications as these are proven effective methods in smoking cessation.
Nicotine replacement therapy products contain varying amounts of nicotine and are effective in reducing nicotine cravings as well as withdrawal symptoms. Behavioral therapy and support are essential in helping smokers develop skills to give up cigarette smoking for good.
Nursing Assessment
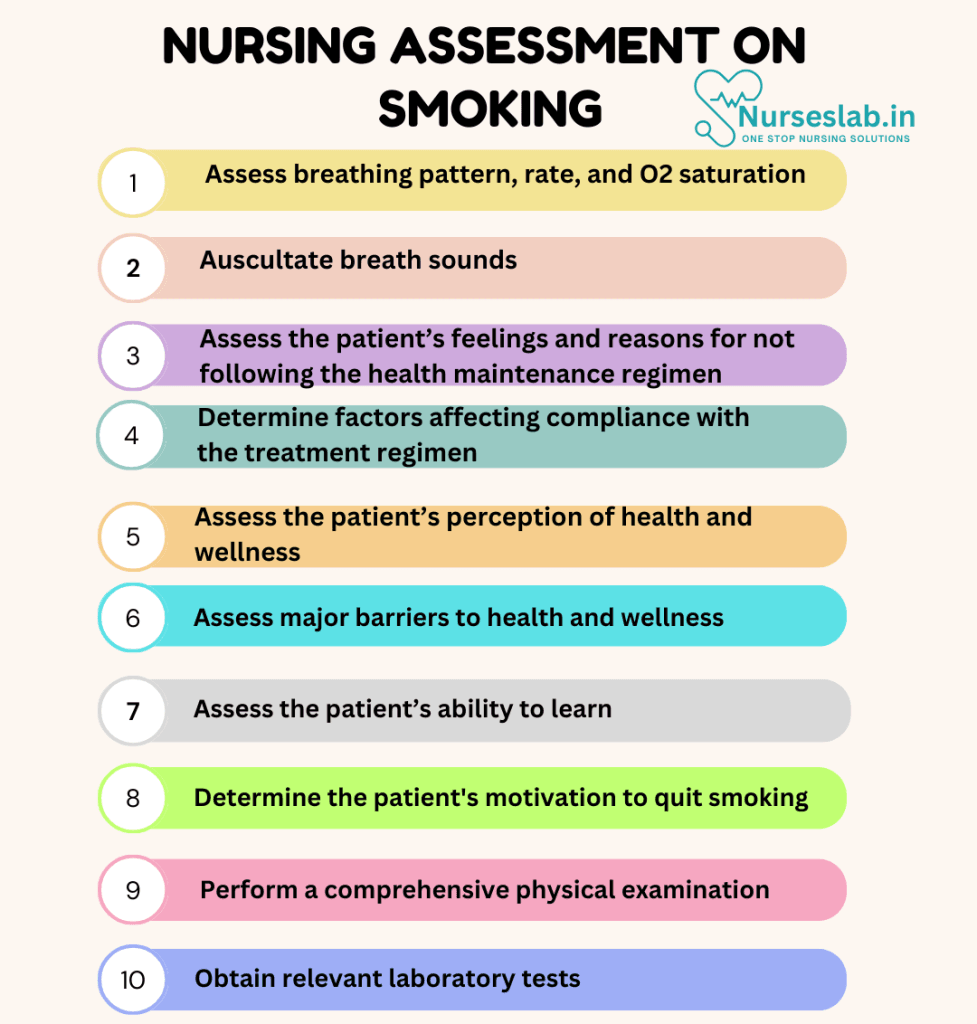
The initial evaluation of a patient who smokes involves a detailed medical history, physical examination, and assessment of smoking habits. Key aspects to assess include:
- Medical History: Review the patient’s medical history for conditions that may be exacerbated by smoking, such as chronic obstructive pulmonary disease (COPD), asthma, cardiovascular diseases, and cancers. Inquire about previous attempts to quit smoking, any withdrawal symptoms experienced, and the methods used.
- Smoking Habits: Assess the patient’s smoking history, including the age of initiation, the number of cigarettes smoked per day, the duration of smoking, and the presence of any smoking triggers or patterns.
- Motivation and Readiness to Quit: Determine the patient’s motivation to quit smoking and their readiness to engage in a cessation program. Use tools such as the Stages of Change model to identify where the patient is in their journey towards quitting.
- Physical Examination: Perform a comprehensive physical examination, focusing on signs and symptoms of smoking-related diseases, such as chronic cough, wheezing, shortness of breath, and cyanosis. Measure vital signs, including blood pressure, heart rate, and oxygen saturation.
- Laboratory Tests: Obtain relevant laboratory tests to evaluate the impact of smoking on the patient’s health. These may include lung function tests (spirometry), complete blood count (CBC), lipid profile, and carbon monoxide (CO) levels in the blood.
Nursing Interventions
Nursing interventions are pivotal in the effective management of smoking cessation. By conducting thorough evaluations, implementing evidence-based interventions, and providing comprehensive patient education, nurses can significantly improve patient outcomes and quality of life.

Patient Education
Educating patients about the harmful effects of smoking and the benefits of quitting is a fundamental nursing intervention. Key points to cover include:
- Health Risks: Explain the various health risks associated with smoking, including respiratory diseases, cardiovascular conditions, cancers, and the impact on overall health and longevity.
- Benefits of Quitting: Highlight the immediate and long-term benefits of quitting smoking, such as improved lung function, reduced risk of heart disease, increased life expectancy, and enhanced quality of life.
- Withdrawal Symptoms: Inform patients about common withdrawal symptoms, such as irritability, anxiety, difficulty concentrating, and increased appetite. Reassure them that these symptoms are temporary and can be managed.
- Resources and Support: Provide information on available resources and support systems, including quitlines, smoking cessation programs, support groups, and online resources.
Behavioural Interventions
Behavioral interventions play a crucial role in helping patients quit smoking. Effective strategies include:
- Cognitive-Behavioral Therapy (CBT): Use CBT techniques to help patients identify and change negative thought patterns and behaviors associated with smoking. Teach coping skills to manage stress and cravings.
- Motivational Interviewing (MI): Employ MI techniques to enhance patients’ motivation and commitment to quitting. Use open-ended questions, reflective listening, and affirmations to support patients in their decision-making process.
- Stress Management: Teach patients stress management techniques, such as deep breathing exercises, progressive muscle relaxation, and mindfulness meditation, to help them cope with triggers and reduce the urge to smoke.
- Relapse Prevention: Prepare patients for potential relapse scenarios and develop strategies to prevent them. Encourage patients to identify and avoid triggers, seek support, and maintain a positive mindset.
Pharmacological Interventions
Pharmacological interventions can support patients in quitting smoking by reducing withdrawal symptoms and cravings. Common options include:
- Nicotine Replacement Therapy (NRT): Offer NRT products, such as nicotine patches, gum, lozenges, inhalers, and nasal sprays, to help patients gradually reduce their nicotine dependence.
- Prescription Medications: Prescribe medications such as bupropion (Zyban) and varenicline (Chantix) to aid smoking cessation. Monitor patients for potential side effects and provide guidance on proper usage.
Involving Family Members
Engaging the patient’s family in the smoking cessation process can enhance support and improve outcomes. Strategies include:
- Family Education: Educate family members about the dangers of smoking and the benefits of quitting. Provide guidance on how they can support their loved one’s cessation efforts.
- Family Therapy: Offer family therapy sessions to address relational issues and improve dynamics that may contribute to smoking behavior.
- Participation in Care: Encourage family members to participate in the patient’s care plan and attend smoking cessation sessions together.
Community Integration
Facilitating community integration helps patients access resources and maintain a sense of normalcy. Key actions include:
- Access to Resources: Assist patients in accessing community resources, such as smoking cessation programs, support groups, vocational training, and recreational activities.
- Collaboration with Social Workers: Collaborate with social workers to provide financial assistance and connect patients with appropriate community services.
Nursing Care Plans
Once the nurse identifies nursing diagnoses related to smoking, nursing care plans help prioritize assessments and interventions for both short and long-term goals of care. In the following section, you will find nursing care plan examples related to smoking.
Ineffective Breathing Pattern
Cigarette smoking is associated with acute changes in respiratory function, including coughing, airway irritation, and impaired airflow resistance. It can cause health conditions like COPD, chronic bronchitis, and emphysema.
Over time, the toxins from cigarette smoke will start to build up and cause thinning of the alveoli. When this happens, the air sacs in the lungs will become less efficient, making it difficult to breathe in oxygen and expel carbon dioxide.
Nursing Diagnosis: Ineffective Breathing Pattern
Related to:
- Smoking
- Impaired gas exchange
- Complications of cigarette smoking
As evidenced by:
- Decreased expiratory pressure
- Decreased inspiratory pressure
- Hypoxemia
- Hypoxia
- Coughing
- Nasal flaring
- Tachypnea
- Bradypnea
- Hyperventilation
- Hypoventilation
Expected Outcomes:
- The patient will be able to breathe comfortably with respiratory rate and rhythm with normal parameters
- The patient will not develop preventable lung diseases
Assessment:
1. Assess breathing pattern, rate, and O2 saturation.
Alterations in the normal breathing rate, rhythm, and O2 sat can indicate physiological respiratory complications and the development of incurable diseases.
2. Auscultate breath sounds.
Abnormal lung sounds like wheezes and crackles can indicate impaired pulmonary function, infections, and long-term lung damage.
Interventions:
1. Promote adequate oxygenation.
Providing supplemental oxygen can help correct hypoxemia in smokers with respiratory complications. Continuous oxygen may be needed for end-stage COPD and emphysema. Remind the patient never to smoke when using or around oxygen.
2. Promote the use of bronchodilators.
Inhaled corticosteroids are often needed to open airways and reduce inflammation.
3. Encourage and support the patient to stop smoking.
Continue to educate the patient on the effects of smoking on their body and lungs. Ask the client if they are ready to quit smoking and provide resources if applicable.
4. Encourage controlled coughing and deep breathing exercises.
Mucus accumulation can occur in the air sacs due to toxins from cigarette smoking. Controlled coughing and deep breathing allow adequate lung expansion and expulsion of mucus from the lungs.
Ineffective Health Maintenance Behaviors
Patients who smoke exhibit ineffective health maintenance behaviors as they fail to maintain their physical, mental, spiritual, or mental health. They are often in denial that this unhealthy behavior is causing them harm.
Nursing Diagnosis: Ineffective Health Maintenance
Related to:
- Competing demands
- Competing lifestyle preferences
- Conflict between cultural beliefs and health practices
- Depressive symptoms
- Difficulty accessing community resources
- Difficulty with decision-making
- Inability to seek or request health information
As evidenced by:
- Failure to take action that reduces risks
- Failure to take action that prevents health problems
- Inadequate health literacy
- Inadequate commitment to a plan of action
- Inadequate knowledge of basic health practices
- Inadequate interest in improving health
- A pattern of lack of health-seeking behavior
- Poor personal support system
Expected Outcomes:
- The patient will discuss perceived barriers in following a health regimen and adhering to the agreed health maintenance plan
- The patient will agree to and participate in a place of action to quit smoking
Assessment:
1. Assess the patient’s feelings and reasons for not following the health maintenance regimen.
Emotions play an important role in how we act and comply with appropriate healthcare behaviors. Assess for issues such as grief, depression, or spiritual distress.
2. Determine economic, mental, emotional, spiritual, and cultural patterns affecting compliance with the treatment regimen.
Patients who smoke may have beliefs and values that challenge their adherence to a healthcare maintenance regimen.
Interventions:
1. Involve the patient in planning an appropriate regimen to promote smoking cessation.
Patients who are involved in shared decision-making have a higher chance of adhering to the treatment plan.
2. Help the patient pick a quit day.
One of the first steps in quitting is having a plan and picking a day. It shouldn’t be a date too far or soon. This allows the patient to mentally prepare.
3. Explore pharmacologic interventions.
Nicotine replacement therapy comes in the form of gums, lozenges, patches, and sprays to prevent withdrawal symptoms and reduce cravings.
4. Teach to avoid triggers and remind themselves of the benefits.
Resisting cravings is one of the hardest parts of quitting smoking. Discuss avoiding triggers such as going for a walk instead of smoking, or avoiding certain places where others smoke. In time, cravings will become less. When cravings occur, have the patient remind themselves of their reason for quitting such as traveling or saving money.
Risk-Prone Health Behavior
Patients who are addicted to smoking and nicotine will find it difficult to modify their lifestyle and unhealthy behaviors even if they are aware that these behaviors are putting their health at risk.
Nursing Diagnosis: Risk-Prone Health Behavior
Related to:
- Unhealthy lifestyle
- Addictive behavior
- Inadequate understanding of health information
- Inadequate social support
- Low socioeconomic status
- Low self-efficacy
- Social anxiety
- Stressors
As evidenced by:
- Failure to achieve an optimal sense of control
- Failure to take action that prevents health problems
- Minimizes health status change
- Continuing to smoke despite health effects
- Substance misuse
Expected Outcomes:
- The patient will verbalize acceptance of health status changes and the need to quit smoking
- The patient will verbalize two strategies to quit smoking
Assessment:
1. Assess the patient’s perception of health and wellness.
Every person has a unique and individual perception of concepts of well-being and illness. Do not push personal perceptions or judgments onto the patient. They must have their own motivation to quit or they will not be successful.
2. Assess major barriers to health and wellness.
The patient’s cultural and social beliefs and current mental and emotional state can be a major hindrance in promoting and adapting to healthy lifestyle modifications.
Interventions:
1. Discuss with the patient current health goals.
Smoking is addictive and without an established goal to change this unhealthy behavior, smoking cessation cannot be achieved.
2. Help the patient recognize the influence of others.
If the patient’s family and peers also smoke, it can make quitting much more difficult. Help the patient recognize who they spend their time with and how they may be able to limit interactions to reduce the influence of smoking.
3. Explore previous attempts to quit.
Discuss what the patient has tried in the past if they attempted quitting. This can help the nurse offer tips and resources to successfully quit smoking.
4. Refer the patient to support programs.
Many states have tobacco quit programs that provide free counseling, resources, and medications to quit smoking.
Nursing Diagnoses and Rationales for Smoking
1. Ineffective Airway Clearance
Rationale: Smoking damages the cilia in the respiratory tract, leading to an accumulation of mucus and impaired clearance of secretions. This can result in chronic cough, increased risk of respiratory infections, and decreased lung function. Regular monitoring of respiratory status, encouraging fluid intake, and teaching effective coughing techniques can help improve airway clearance.
2. Risk for Impaired Gas Exchange
Rationale: Smoking reduces the surface area available for gas exchange in the lungs, leading to hypoxemia and hypercapnia. Assessing oxygen saturation levels, providing supplemental oxygen as needed, and promoting smoking cessation are critical interventions to enhance gas exchange.
3. Ineffective Peripheral Tissue Perfusion
Rationale: Nicotine in cigarettes causes vasoconstriction, which can reduce blood flow to peripheral tissues. This can lead to symptoms such as cold extremities, delayed wound healing, and intermittent claudication. Encouraging smoking cessation and monitoring circulation can help prevent complications associated with impaired tissue perfusion.
4. Anxiety
Rationale: Smoking can be both a cause and a symptom of anxiety. Nicotine addiction and withdrawal can exacerbate anxiety symptoms. Providing support for smoking cessation, offering relaxation techniques, and referring to mental health services if needed can help manage anxiety related to smoking.
5. Knowledge Deficit
Rationale: Patients may not be fully aware of the health risks associated with smoking or the benefits of quitting. Educating patients about the harmful effects of smoking, the advantages of cessation, and available resources for quitting can empower them to make informed decisions about their health.
6. Risk for Impaired Skin Integrity
Rationale: Smoking impairs blood flow and oxygen delivery to the skin, increasing the risk of skin breakdown and delayed wound healing. Regular skin assessments, encouraging good skin hygiene, and promoting smoking cessation can help maintain skin integrity.
7. Activity Intolerance
Rationale: Smoking reduces exercise tolerance due to decreased lung function and cardiovascular efficiency. Assessing activity levels, developing a gradual exercise plan, and encouraging smoking cessation can help improve physical endurance over time.
8. Risk for Infection
Rationale: Smoking weakens the immune system, making patients more susceptible to infections, particularly respiratory infections. Educating patients on infection prevention strategies, such as hand hygiene and vaccination, can reduce their risk of infections.
REFERENCES
- 10 Health Effects Caused by Smoking You Didn’t Know About. American Lung Association. Updated: January 26, 2022. From https://www.lung.org/research/sotc/by-the-numbers/10-health-effects-caused-by-smoking
- ACCN Essentials of Critical Care Nursing. 3rd Edition. Suzanne M. Burns, MSN, RRT, ACNP, CCRN, FAAN, FCCM, FAANP. 2014. McGraw Hill Education.
- Cigarette smoking and the adrenergic nervous system. Grassi G, Seravalle G, Calhoun DA, Bolla G, Mancia G. Clin Exp Hypertens A. 1992;14(1-2):251-60. doi: 10.3109/10641969209036186. PMID: 1541039. From: https://pubmed.ncbi.nlm.nih.gov/1541039/
- Medical-Surgical Nursing: Concepts for Interprofessional Collaborative Care. 9th Edition. Donna D. Ignatavicius, MS, RN, CNE, ANEF. 2018. Elsevier, Inc.
- Centers for Disease Control and Prevention. (2024). Smoking & Tobacco Use. American Journal of Preventive Medicine, 56(2), 181-193.
- Smith, J., & Johnson, K. (2023). Evidence-Based Nursing Interventions for Smoking Cessation. Journal of Clinical Nursing, 32(5), 891-902.
- World Health Organization. (2024). Global Report on Tobacco Cessation and Care. WHO Technical Report Series.
- Brown, M., et al. (2023). Nursing Care Plans for Tobacco Dependence: A Systematic Review. International Journal of Nursing Studies, 89, 32-41.
- Anderson, P., & Wilson, R. (2024). Clinical Guidelines for Smoking Cessation Support. Nursing Research, 73(1), 15-27.
- Thompson, S., et al. (2023). Best Practices in Nursing Management of Tobacco Use. Advanced Nursing Practice Quarterly, 45(3), 228-240.
- Smoking. Cleveland Clinic. Reviewed: October 28, 2020. From: https://my.clevelandclinic.org/health/articles/17488-smoking
- What are the health risks of smoking? NHS. Reviewed: October 9, 2018. From: https://www.nhs.uk/common-health-questions/lifestyle/what-are-the-health-risks-of-smoking/
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.







