Paraplegia is a condition characterized by paralysis that primarily affects the legs, but it can also involve the lower body and, in some cases, impair arm function. It most commonly results from damage to the spinal cord, but can also be caused by other medical conditions and diseases that affect the nervous system.
Overview
The level and severity of the condition can be further classified into the following types of paraplegia:
Complete paraplegia: This type of injury causes total loss of function of the legs with symptoms like loss of sensation, movement, and bladder and bowel control.
Incomplete/partial paraplegia: This type of injury causes partial loss of function, and patients may still be able to move one leg or feel sensations below the level of injury.
An injury that affects the thoracic spine may also affect the abdominal and respiratory muscles making breathing and coughing difficult. If the lumbar spine is affected, chest and abdominal muscles will be spared, but bowel and bladder control may be affected. Sacral spinal injuries are more likely to cause partial paraplegia, and the patient may be able to walk with devices or braces. Bowel or bladder control may still be affected.
Symptoms of paraplegia other than loss of movement and sensation include:
- Phantom pain or sensations
- Loss of sexual function
- Loss of bowel or bladder function
- Depression
- Chronic pain
- Autonomic dysreflexia causing changes in vital signs, sweating, and temperature changes
Paraplegia is caused by injury to the spinal cord due to motor vehicle accidents, penetrating injuries, falls, and medical conditions like spinal cord tumors, cysts, infection, stroke, ischemia, and inflammatory diseases like multiple sclerosis.
Paraplegia is diagnosed through imaging: x-ray, CT scan, or MRI, neurological exams, and electromyography.
Nursing Process
The management of paraplegia often focuses on preventing complications and further injuries. Immediate medical treatment can prevent partial paraplegia from becoming complete paraplegia. Physical and rehabilitation therapy is vital to strengthening muscles and alleviating pain. The nurse can support and encourage lifestyle modifications to empower patients to live actively and productively.
Nursing Assessment
A thorough nursing assessment is essential for developing an individualized care plan for patients with paraplegia. The assessment should include the following components:
1. Physical Assessment
- Neurological Examination: Assess motor function, sensory function, and reflexes to determine the level and extent of the spinal cord injury.
- Skin Integrity: Inspect for pressure ulcers, especially in areas prone to pressure due to immobility, such as the sacrum, heels, and hips.
- Musculoskeletal System: Evaluate muscle strength, tone, and range of motion in the lower extremities. Monitor for joint contractures and spasticity.
- Respiratory Function: Assess respiratory rate, depth, and pattern. Check for signs of respiratory distress or infections, as individuals with paraplegia may have compromised respiratory function.
- Cardiovascular Status: Monitor blood pressure, heart rate, and signs of orthostatic hypotension. Assess for deep vein thrombosis (DVT) and peripheral edema.
- Bladder and Bowel Function: Evaluate urinary and bowel patterns, monitor for signs of urinary tract infections (UTIs), and assess for bowel incontinence or constipation.
2. Psychosocial Assessment
- Emotional Well-being: Assess the patient’s emotional state, coping mechanisms, and mental health. Address feelings of depression, anxiety, or frustration.
- Social Support: Evaluate the availability and strength of the patient’s support system, including family, friends, and community resources.
- Cognitive Function: Assess cognitive abilities and any changes in mental status that may affect the patient’s ability to participate in their care.
3. Functional Assessment
- Activities of Daily Living (ADLs): Evaluate the patient’s ability to perform ADLs such as bathing, dressing, grooming, and feeding.
- Mobility: Assess the patient’s mobility status, including the use of assistive devices, transfers, and wheelchair skills.
- Home Environment: Evaluate the patient’s living conditions, accessibility, and potential barriers to independence.
Nursing Intervention
Nursing interventions for patients with paraplegia focus on preventing complications, promoting independence, and enhancing quality of life. Key interventions include:
1. Skin Care
- Implement a regular turning schedule to prevent pressure ulcers.
- Use pressure-relieving devices such as specialized mattresses and cushions.
- Maintain skin hygiene and monitor for signs of skin breakdown.
- Educate the patient and caregivers on skin care practices and pressure ulcer prevention.
2. Respiratory Management
- Encourage deep breathing exercises and incentive spirometry to maintain lung function.
- Monitor for signs of respiratory infections and provide prompt treatment if needed.
- Position the patient to optimize respiratory function and prevent complications.
3. Cardiovascular Care
- Monitor for signs of orthostatic hypotension and educate the patient on preventive measures.
- Promote venous return through the use of compression stockings and regular leg exercises.
- Monitor for signs of DVT and provide prophylactic measures as needed.
4. Bladder and Bowel Management
- Implement a bladder training program and monitor for signs of UTIs.
- Educate the patient on intermittent catheterization if required.
- Establish a bowel routine to prevent constipation and fecal incontinence.
- Provide dietary modifications and medications as needed to promote bowel function.
5. Mobility and Rehabilitation
- Collaborate with physical and occupational therapists to develop a rehabilitation plan.
- Encourage the use of assistive devices to enhance mobility and independence.
- Provide training on transfers, wheelchair skills, and other mobility techniques.
- Promote participation in exercise programs to maintain muscle strength and prevent complications.
6. Psychosocial Support
- Provide emotional support and counseling to address feelings of depression, anxiety, or frustration.
- Facilitate support groups and peer interactions to enhance social support.
- Educate the patient and family on coping strategies and available resources.
Nursing Care Plans
Once the nurse identifies nursing diagnoses for paraplegia, nursing care plans help prioritize assessments and interventions for both short and long-term goals of care. In the following section, you will find nursing care plan examples for paraplegia.
Autonomic Dysreflexia
Paraplegia is characterized by paralysis and loss of sensation in the lower extremities that occurs after a spinal cord injury. With paraplegia, autonomic dysreflexia can occur as an overreaction of the patient’s autonomic nervous system from noxious stimuli, resulting in potentially life-threatening hypertension.
Nursing Diagnosis: Autonomic Dysreflexia
Related to:
- Constipation
- Skin irritation
- Tissue injury
- Constricting clothing
- Positioning
- Bladder distention
- Urinary tract infection
- Sexual intercourse
- Painful stimuli below the level of injury
As evidenced by:
- Blurred vision
- Severe headache
- Bradycardia
- Tachycardia
- Chest pain
- Nasal congestion
- Paresthesia
- Diaphoresis above the level of injury
- Pallor below the level of injury
Expected outcomes:
- Patient will maintain vital signs within normal limits.
- Patient and caregivers will verbalize the causes and prevention of autonomic dysreflexia.
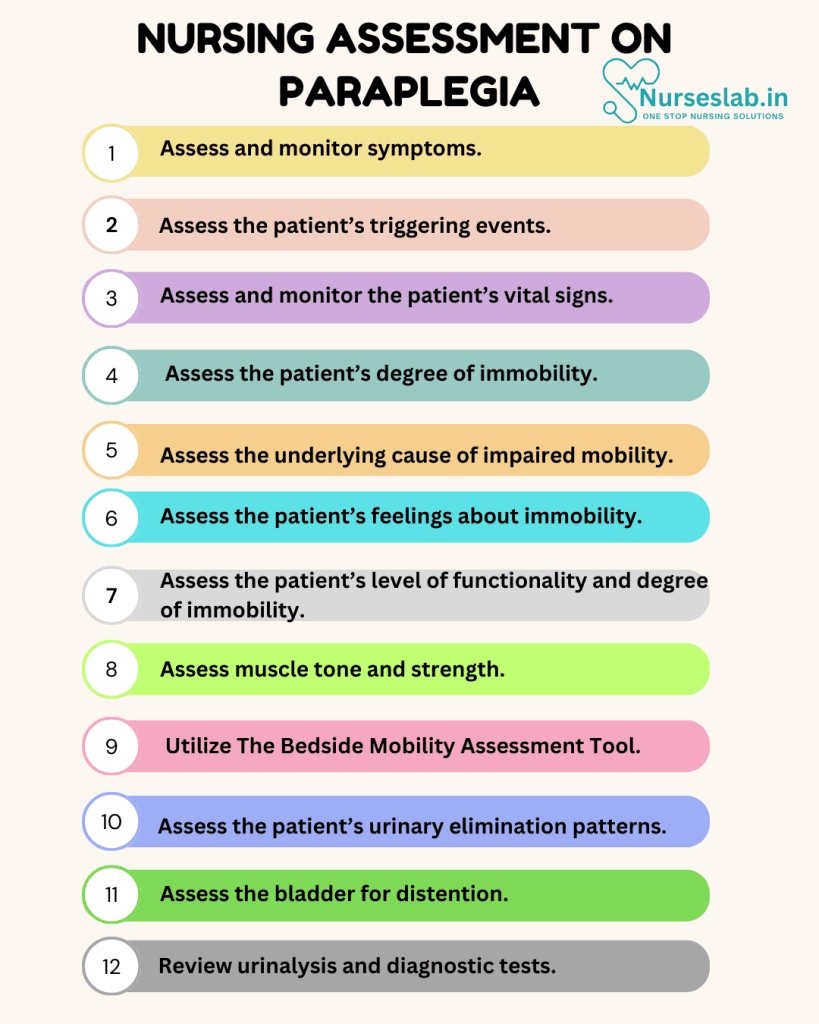
Assessment:
1. Assess and monitor symptoms.
A severe headache may be the first presenting symptom. If a patient with paraplegia reports this symptom, the nurse should immediately assess the patient’s blood pressure.
2. Assess the patient’s triggering events.
Patients are often knowledgeable about what causes their episodes of autonomic dysreflexia. The nurse can inquire about precipitating factors in order to develop a plan of care. If unknown, the nurse can assist the patient in identifying potential causes.
3. Assess and monitor the patient’s vital signs.
Autonomic dysreflexia causes life-threatening hypertension due to vasodilation that can result in a lethal stroke. Patients with symptoms of autonomic dysreflexia should have their blood pressure closely monitored.
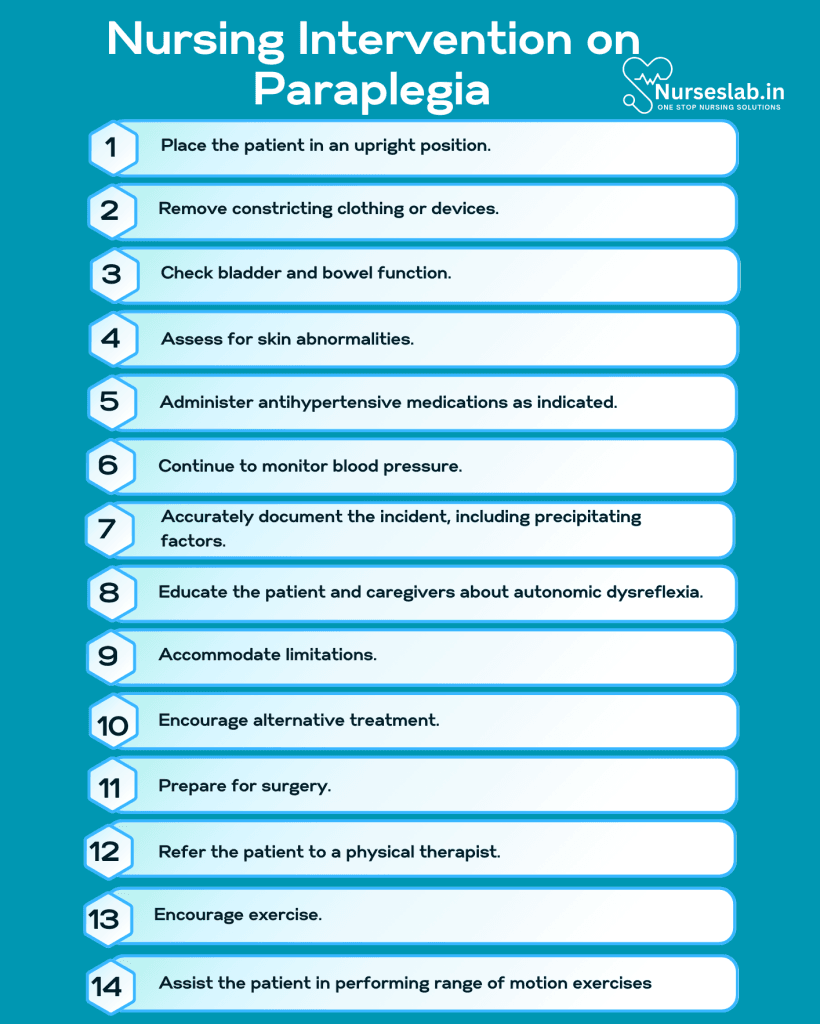
Interventions:
1. Place the patient in an upright position.
The first immediate step is to assist the patient into a high-Fowler’s or upright position with the legs dangling in an effort to reduce the blood pressure.
2. Remove constricting clothing or devices.
Loosen or remove tight clothing, shoes, compression stockings, and binders, and ensure IV lines and catheters are not pressing into the skin.
3. Check bladder and bowel function.
Kinked catheters and bladder distention are common causes of autonomic dysreflexia. Obtain a urinalysis as another potential source. If normal, an evaluation for fecal impaction should occur next.
4. Assess for skin abnormalities.
If bladder and bowel assessments are normal, the nurse should next evaluate the skin for wounds, pressure ulcers, ingrown toenails, etc.
5. Administer antihypertensive medications as indicated.
Nitroglycerin 2% paste is the initial medication administered for hypertension in autonomic dysreflexia. Immediate-release nifedipine is the next preferred medication choice.
6. Continue to monitor blood pressure.
The nurse should reassess the blood pressure every three to five minutes during an episode and for up to two hours after the episode.
7. Accurately document the incident, including precipitating factors.
It is important to document any episodes of autonomic dysreflexia, including the precipitating cause. This is especially important if the trigger is unusual.
8. Educate the patient and caregivers about autonomic dysreflexia.
Autonomic dysreflexia occurs in about 90% of paraplegic patients with spinal cord injuries at or above the level of T6. The nurse should educate the patient and family/caregivers about the causes and symptoms of this disorder to prevent life-threatening complications.
Impaired Physical Mobility
Spinal cord injury and paraplegia result in impaired physical mobility and loss of function, which can significantly decrease quality of life.
Nursing Diagnosis: Impaired Physical Mobility
Related to:
- Neuromuscular dysfunction
- Decreased muscle control
- Decreased muscle strength
- Joint stiffness
- Pain
As evidenced by:
- Inability to move purposely
- Decreased gross motor skills
- Paralysis
- Postural instability
- Decreased range of motion
- Muscle atrophy
- Muscle spasticity
Expected outcomes:
- Patient will demonstrate the use of assistive devices effectively.
- Patient will participate in rehabilitation and physical therapy as prescribed.
Assessment:
1. Assess the patient’s degree of immobility.
Paraplegia can be complete or incomplete. Treatment and management must be tailored according to the patient’s degree of immobility.
2. Assess the underlying cause of impaired mobility.
The patient may also struggle with motivational or psychological causes that prevent movement. The nurse and healthcare team should assess for additional barriers.
3. Assess the patient’s feelings about immobility.
Depression and negative emotions can affect adherence to the treatment regimen and attempts at rehabilitation.
Interventions:
1. Accommodate limitations.
Home settings may require ramps or lifts installed while cars can be outfitted to support wheelchairs.
2. Encourage alternative treatment.
Acupuncture, massage, and chiropractic care can make mobility less painful.
3. Prepare for surgery.
Some physical limitations may be relieved through surgery at the site of injury, such as removing a tumor.
4. Refer the patient to a physical therapist.
Ongoing physical therapy provides appropriate rehabilitative exercises for patients with paraplegia.
5. Encourage exercise.
Swimming, yoga, and seated aerobics can help with stretching to prevent muscle atrophy and promote controlled breathing to avoid respiratory complications.
Impaired Sitting/Standing/Transfer Ability
Paraplegia is characterized by paralysis and loss of sensation in the lower body leading to difficulty with mobility, sitting, and standing.
Nursing Diagnosis: Impaired Physical Mobility
Related to:
- Disease process
- Immobility
- Paralysis
- Insufficient muscle strength
- Loss of sensation in the lower extremities
As evidenced by:
- Difficulty adjusting the position of one or both lower limbs on an uneven surface
- Difficulty flexing/extending one or both knees
- Difficulty maintaining a balanced torso
- Difficulty flexing one or both hips
- Difficulty maintaining postural balance
- Difficulty transferring between the bed and chair/standing
- Difficulty transferring in/out of the shower
- Difficulty ambulating
- Difficulty climbing stairs
Expected outcomes:
- Patient will demonstrate independence with sitting/standing/transferring within their physical capabilities.
- Patient will demonstrate the use of assistive devices to sit/stand/transfer.
Assessment:
1. Assess the patient’s level of functionality and degree of immobility.
The patient’s degree of impairment with sitting, standing, and transferring is dependent on their level of spinal cord injury. Identifying the patient’s level of paralysis and functionality will help plan an appropriate treatment regimen.
2. Assess muscle tone and strength.
When considering the patient’s physical capabilities, the nurse should assess the patient’s muscle strength, tone, range of motion, balance, and coordination.
3. Utilize The Bedside Mobility Assessment Tool.
Nurses can use The Bedside Mobility Assessment Tool to evaluate the patient’s mobility status and determine the level of assistance necessary for transferring or ambulation.
Interventions:
1. Assist the patient in performing range of motion exercises.
Range of motion exercises can help improve circulation, prevent contractures and atrophy, and restore muscle tone.
2. Refer the patient to occupational and physical therapy.
Physical and occupational therapists can help patients develop appropriate exercise and strengthening programs and advise on equipment and devices to aid mobility.
3. Instruct on the use of mobility aids and transfer devices.
Mobility and transfer devices such as slide boards, lifts, walkers, wheelchairs, canes, and more can help paraplegic patients move, sit, stand, and transfer from one position to another while reducing the risk of injury and falls.
4. Consider the use of braces and orthotics.
The nurse can discuss fitting the client with braces or orthotics to aid in stabilizing the knee, ankle, or foot to assist with movement.
Impaired Urinary Elimination
Patients with paraplegia may not have bladder and bowel control due to disrupted transmission between the brain and nerves that control elimination, referred to as neurogenic bladder.
Nursing Diagnosis: Impaired Urinary Elimination
Related to:
- Disease process
- Bladder dysfunction
- Involuntary sphincter relaxation
- Weakened bladder muscles
As evidenced by:
- Dysuria
- Nocturia
- Urinary hesitancy
- Urinary urgency
- Urinary retention
- Urinary incontinence
- Frequent bladder or urinary infections
Expected outcomes:
- Patient will verbalize symptoms of a bladder or urinary infection.
- Patient will demonstrate how to care for a urinary catheter properly.
Assessment:
1. Assess the patient’s urinary elimination patterns.
Assess for incontinence episodes, frequent infections, nocturia, or difficulty emptying to determine possible causes and related interventions.
2. Assess the bladder for distention.
Bladder dysfunction can manifest with bladder distention and overflow. A distended bladder can contribute to an infection. The nurse can perform a post-void residual to assess for impairments in emptying.
3. Review urinalysis and diagnostic tests.
Urodynamic testing evaluates urinary tract dysfunction and the exact cause of the impaired urinary elimination. Urinalysis can assess the presence of bacteria.
Interventions:
1. Encourage adequate fluid intake.
Patients may limit fluid intake to prevent the need to urinate, but this can cause urinary stasis and dehydration. Adequate fluid intake is necessary to maintain renal function and prevent urinary tract infections.
2. Evaluate urine color, odor, and other characteristics.
Dark urine color and a strong odor can signal dehydration or an infection. The presence of blood, pus, or stones, can indicate further complications.
3. Instruct on the Credé maneuver.
Applying manual pressure on the abdomen below the umbilicus and stroking downward can stimulate the voiding reflex. The goal is to place pressure on the bladder while the urethral sphincter relaxes to drain urine in patients with neurogenic bladder.
4. Insert a urinary catheter as indicated.
An intermittent or indwelling urinary catheter may be required for some patients with neurogenic bladder. Suprapubic catheters may be easier to manage long-term.
5. Administer anticholinergics.
These medications can increase bladder capacity, reduce bladder pressure, and preserve renal function in patients with neurogenic bladder.
6. Educate on botulinum toxin.
Botox is an effective treatment that can increase bladder capacity and reduce incontinence.
Risk for Injury
Paraplegic patients have a higher risk for injuries because of the loss of function and sensation.
Nursing Diagnosis: Risk for Injury
Related to:
- Altered psychomotor performance
- Neuromuscular injury
- Spinal cord injury
- Muscle weakness
- Inability to move lower extremities
- Sensory disruption
As evidenced by:
A risk diagnosis is not evidenced by signs and symptoms, as the problem has not occurred yet, and nursing interventions are directed at preventing signs and symptoms.
Expected outcomes:
- Patient will be free from falls, injury, or skin breakdown.
- Patient will adhere to the use of safety equipment at all times.
Assessment:
1. Assess risk factors predisposing the patient to injury.
Patients with paraplegia have difficulty making purposeful movements in their lower extremities, increasing the risk of injuries and falls. Assess for a loss of sensations that also predispose the patient to injuries.
2. Assess the environment for any hazards.
Hazardous items must be removed from the environment or altered to ensure the patient’s safety.
3. Assess the availability of a support person.
A patient with paraplegia may require frequent care and assistance by a caregiver for movement, ADLs, elimination, and injury prevention.
Interventions:
1. Assist the patient with transferring or ambulating
The patient that can ambulate should be assisted with a gait belt, walker, braces, etc. The client with no lower leg function should be assisted to transfer and turn by a competent individual.
2. Prevent skin breakdown.
Pressure injuries are a significant complication of paraplegia. The patient may not be able to feel sharp or painful sensations. Reposition the patient frequently and keep IV lines and cords away from their body to prevent damaging tissues.
3. Encourage self-care.
Patients with paraplegia can still perform self-care activities as they have the use of their arms. The patient may be able to use a trapeze bar to reposition themselves, can likely perform some of their grooming, and feed themselves.
4. Refer the patient to rehabilitation programs.
Rehabilitation programs for paraplegic patients are available to provide support, maintain muscle strength and mass, and teach techniques to maneuver and perform tasks safely and independently.
Nursing Diagnosis and Rationale for Paraplegia
1. Impaired Physical Mobility
Rationale: Paraplegia leads to significant limitations in physical mobility, affecting the patient’s ability to perform daily activities. Nurses should evaluate the patient’s range of motion, strength, and functional abilities. Implementing physical therapy programs and assisting with mobility aids can help enhance independence and prevent complications such as muscle atrophy and contractures.
2. Risk for Pressure Ulcers
Rationale: Patients with paraplegia are at a high risk of developing pressure ulcers due to prolonged immobility and decreased sensation. Nurses should regularly inspect the skin for signs of pressure injury, reposition the patient every two hours, and use pressure-relieving devices. Educating the patient and caregivers on skin care and the importance of maintaining good nutrition and hydration is also vital.
3. Impaired Urinary Elimination
Rationale: Paraplegia often results in neurogenic bladder dysfunction, leading to issues with urinary retention or incontinence. Nurses should monitor urinary output, assess for signs of urinary tract infections, and assist with bladder management techniques such as intermittent catheterization or the use of indwelling catheters. Collaborating with a urologist can ensure optimal bladder care.
4. Constipation
Rationale: Reduced physical activity and neurogenic bowel dysfunction in patients with paraplegia can increase the risk of constipation. Nurses should assess bowel patterns, encourage a high-fiber diet, adequate fluid intake, and regular bowel routines. Administering stool softeners or laxatives as prescribed can also help manage constipation effectively.
5. Risk for Deep Vein Thrombosis (DVT)
Rationale: Prolonged immobility in paraplegic patients can lead to venous stasis and an increased risk of DVT. Nurses should assess for signs of DVT, such as swelling, redness, and pain in the legs. Implementing prophylactic measures such as compression stockings, anticoagulant therapy, and encouraging leg exercises can help prevent DVT.
6. Potential for Autonomic Dysreflexia
Rationale: Patients with paraplegia, especially those with injuries at or above the T6 level, are at risk for autonomic dysreflexia, a potentially life-threatening condition. Nurses should monitor for symptoms such as severe headache, hypertension, and sweating. Educating the patient on triggers and how to manage symptoms, along with prompt intervention, is crucial to prevent complications.
7. Altered Body Image
Rationale: The sudden change in physical abilities and dependence on others can lead to altered body image and self-esteem issues in patients with paraplegia. Nurses should provide psychological support, facilitate support group participation, and encourage the patient to express their feelings. Promoting self-care and independence to the extent possible can also help improve body image.
8. Risk for Respiratory Complications
Rationale: Paraplegic patients may experience respiratory complications due to weakened respiratory muscles and limited chest expansion. Nurses should regularly assess respiratory status, encourage deep breathing exercises, and use incentive spirometry. Providing respiratory therapy and ensuring proper positioning can help maintain optimal respiratory function.
9. Ineffective Coping
Rationale: The psychological impact of paraplegia can lead to ineffective coping mechanisms, including depression and anxiety. Nurses should assess the patient’s emotional state, provide counseling, and refer to mental health professionals as needed. Creating a supportive environment and involving family members in care can also enhance coping strategies.
10. Knowledge Deficit
Rationale: Patients and their families may lack knowledge about paraplegia, its management, and available resources. Nurses should provide comprehensive education on the condition, care techniques, and community support services. Empowering the patient and family with knowledge can improve self-management and enhance the quality of life.
REFERENCES
- ACCN Essentials of Critical Care Nursing. 3rd Edition. Suzanne M. Burns, MSN, RRT, ACNP, CCRN, FAAN, FCCM, FAANP. 2014. McGraw Hill Education.
- Lewis’s Medical-Surgical Nursing. 11th Edition, Mariann M. Harding, RN, Ph.D., FAADN, CNE. 2020. Elsevier, Inc.
- Paraplegia. Beth Israel Lahey Health Winchester Hospital. 2023. From: https://www.winchesterhospital.org/health-library/article?id=230663
- Spinal cord injury. Mayo Clinic. Reviewed: October 02, 2021. From: https://www.mayoclinic.org/diseases-conditions/spinal-cord-injury/symptoms-causes/syc-20377890
- What is paraplegia? The University of Alabama. 2023. From: https://www.uab.edu/medicine/sci/faqs-about-spinal-cord-injury-sci/what-is-paraplegia
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.







