Traumatic brain injury (TBI) is a form of head injury that causes damage to the brain resulting from an external mechanical force. It can result in temporary or permanent impairment in sensory perception, cognition, mobility, or behavior.
Overview
Major causes of TBI include falls, assaults, motor vehicular accidents, and injuries resulting in a blow to the head. This condition may be categorized as mild (concussion) to moderate or severe, causing prolonged unresponsiveness, coma, or death.
Damage occurring due to TBI is described as primary or secondary.
Primary injuries are associated with the direct effects of trauma on the skull and brain at initial impact. Types of primary injuries include:
- Skull fractures
- Intracranial hemorrhage
- Cerebral contusions
- Concussions
- Penetrating injuries (gunshot wounds, projectiles)
Secondary injuries refer to the complications arising hours to days later and may include:
- Increased intracranial pressure
- Cerebral edema
- Hydrocephalus
- Brain herniation
- Chronic traumatic encephalopathy
Nursing Process
Management of TBI varies depending on the severity of the injury. Mild TBI management includes neurologic assessment and patient education about post-concussive symptoms like irritability, fatigue, headache, and sleep disturbances.
The management of moderate to severe TBI focuses more on acute treatment of cerebral perfusion and optimization of functional recovery through minimizing secondary brain injury.
Rehabilitation nurses may continue to support patients recovering from a TBI as they navigate physical, emotional, and cognitive challenges.
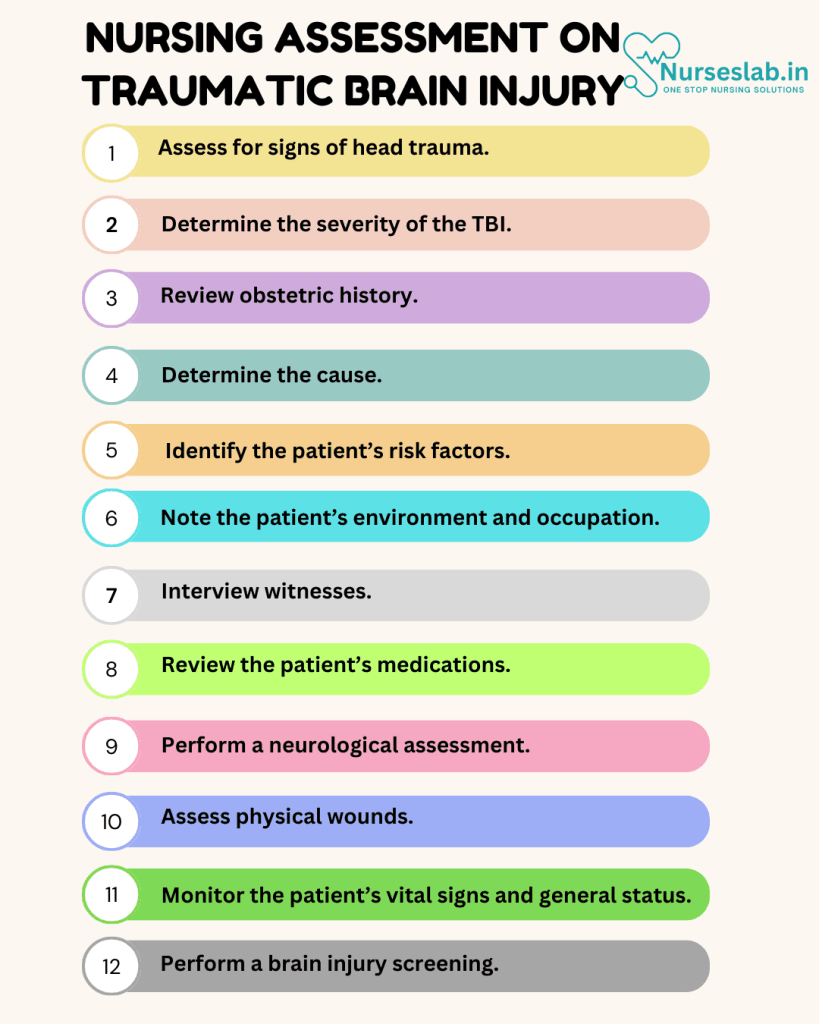
Nursing Assessment
The first step of nursing care is the nursing assessment, during which the nurse will gather physical, psychosocial, emotional, and diagnostic data. In this section, we will cover subjective and objective data related to a traumatic brain injury.
Initial Assessment
Primary Survey
The initial assessment of a patient with suspected TBI should follow the principles of the primary survey:
- Airway: Ensure that the patient’s airway is clear and provide assistance if necessary.
- Breathing: Assess the patient’s respiratory rate, effort, and oxygen saturation. Administer supplemental oxygen if needed.
- Circulation: Monitor blood pressure, heart rate, and capillary refill. Establish intravenous access for fluid resuscitation if required.
- Disability: Evaluate the patient’s level of consciousness using the Glasgow Coma Scale (GCS). This scale provides a standardized method for assessing the severity of TBI. A lower GCS score indicates a more severe injury.
- Exposure: Conduct a thorough physical examination to identify any other injuries that may require immediate attention.
Secondary Survey
Once the patient is stabilized, a more detailed secondary survey should be performed:
- History: Obtain a comprehensive history from the patient or witnesses, including the mechanism of injury, time of occurrence, and any relevant medical history.
- Neurological Examination: Perform a detailed neurological examination to assess cranial nerve function, motor and sensory function, and reflexes. This helps to identify focal neurological deficits that may indicate specific areas of brain injury.
- Imaging: Arrange for appropriate imaging studies, such as a computed tomography (CT) scan or magnetic resonance imaging (MRI), to evaluate the extent of brain injury and guide treatment decisions.
Ongoing Monitoring
Vital Signs
Regularly monitor and document the patient’s vital signs, including blood pressure, heart rate, respiratory rate, and oxygen saturation. Look for signs of increased intracranial pressure (ICP), such as bradycardia, hypertension, and irregular breathing patterns.
Neurological Status
Conduct frequent assessments of the patient’s neurological status using the Glasgow Coma Scale and other relevant tools. Monitor for any changes in level of consciousness, pupil size and reactivity, motor responses, and speech. Promptly report any deterioration in neurological status to the appropriate medical team.
Intracranial Pressure Monitoring
In patients with severe TBI, intracranial pressure monitoring may be necessary. This involves the insertion of a catheter into the brain to measure pressure and guide treatment decisions. Nurses should be familiar with the equipment and protocols for ICP monitoring.
Interdisciplinary Collaboration
Effective management of TBI requires collaboration among a multidisciplinary team, including:
Social Workers: Offer support and resources to help patients and families navigate the healthcare system and access community services.ertension.
Neurologists and Neurosurgeons: Provide specialized expertise in the diagnosis and treatment of brain injuries.
Rehabilitation Therapists: Assist in the recovery and rehabilitation process by providing physical, occupational, and speech therapy.
Psychologists and Psychiatrists: Address the psychological and emotional impact of TBI on the patient and their family.
Nursing Interventions
Nursing interventions and care are essential for the patients recovery. In the following section, you will learn more about possible nursing interventions for a patient with a traumatic brain injury.

1. Provide emergency treatment.
Emergency care in moderate to severe TBI focuses on keeping blood pressure stable, ensuring oxygenation and perfusion, and preventing further head or neck injuries.
2. Administer medications as ordered.
Following a TBI, medications used in the acute phase to prevent further brain damage may include:
- Anticonvulsants
- Coma-inducing drugs
- Mannitol for cerebral edema
3. Encourage the patient to rest.
Limit physical or mental activity that may aggravate symptoms. This “brain rest” may be the only treatment necessary for mild TBI.
4. Anticipate surgical procedures.
Surgery may be necessary to prevent further harm to the brain’s tissues. This may include a decompressive craniectomy to allow room for the brain to expand, evacuating a hematoma, repairing skull fractures, and repairing hemorrhaging.
5. Reduce the intracranial pressure.
Some techniques to lower intracranial pressure include:
- Elevating the head of the bed to a semi-Fowler’s position (30-degree angle)
- Brief hyperventilation
- Hyperosmolar treatment
- Therapeutic cooling
- Barbiturate-induced coma
6. Refer the patient to rehabilitation.
After stabilizing the patient and recovering from initial injuries, rehabilitation may be necessary for severe TBIs. Patients may require support from physical and occupational therapists, speech-language therapists, physiatrists, and neuropsychologists to relearn how to walk, talk, eat, and perform basic skills. The rehabilitation nurse provides continuous care to the patient in the inpatient setting.
7. Offer methods of coping and support.
Recovering from a severe TBI may take months or even years. The patient may experience a range of emotions if relearning basic skills. Support groups can provide an outlet for expression and understanding. Encourage the patient to keep a routine, write down important information, and focus on one task at a time to prevent becoming overwhelmed.
8. Prevent another TBI.
Prevent future TBIs by instituting the following safety measures:
- Reduce the risk of falls in older adults and children
- Wear safety gear such as helmets
- Always wear a seatbelt
- Do not attempt risky activities, especially under the influence of alcohol or drugs
- Keep firearms locked and unloaded
- Participate in physical activity to improve balance
Nursing Care Plans
Once the nurse identifies nursing diagnoses for traumatic brain injury, nursing care plans help prioritize assessments and interventions for both short and long-term goals of care. In the following section, you will find nursing care plan examples for traumatic brain injury.
Acute Confusion
Patients suffering from mild TBI may experience altered cognition, including acute confusion, decreased memory, and impaired reasoning ability. Additionally, severe TBI can cause prolonged confusion with amnesia.
Nursing Diagnosis: Acute Confusion
Related to:
- Brain injury
- Neurologic trauma
- Decreased level of consciousness
As evidenced by:
- Cognitive dysfunction
- Misperception
- Agitation or restlessness
Expected outcomes:
- Patient will maintain a baseline level of consciousness and will not experience decreased memory.
- Patient will be able to respond appropriately to questions.
Assessment:
1. Assess sensory awareness.
Assessment of sensory awareness is crucial to patient safety. Injury to the parietal lobe can cause loss of sensory perception and prevent appropriate responses to environmental stimuli.
2. Assess changes in orientation and personality.
The upper cerebral functions are the first to be affected when there is altered circulation or oxygenation. The damage can occur initially at the onset of the injury or develop later due to swelling or bleeding. Motor, cognitive, perceptual, and personality changes can develop and may persist.
3. Assess the patient’s level of cognitive impairment.
Cognitive impairment can interfere with how the patient with TBI functions. Assessing the patient’s level of cognitive impairment can help determine appropriate rehabilitation.
Interventions:
1. Ensure patient safety.
Patients with acute confusion are not able to follow directions. It is important to promote patient safety by providing a hazard-free environment.
2. Reorient the patient as needed.
Patients with mild TBI may be disoriented and may exhibit short-term memory loss. Frequent reorientation is essential before any interaction to promote a trusting relationship and cooperation from the patient.
3. Keep explanations and activities short and simple.
This allows the patient to better understand the instructions and procedures performed. It is vital to give these explanations before and throughout the patient’s care. They are unlikely to remember long instructions so keep teaching sessions short.
4. Eliminate extraneous noise as necessary.
This can help reduce the patient’s anxiety, confusion, and exaggerated emotional responses associated with sensory overload.
5. Provide structured therapies and activities.
This will help promote consistency and reassurance, reduces the patient’s anxiety and confusion, and promotes a sense of control.
Deficient Knowledge
Many patients suffering from TBI exhibit various long-term physical and cognitive disabilities. Patient and family education is important to clarify misconceptions, implement new behaviors to adapt to the resulting changes, develop coping strategies, and ensure adherence to the plan of care.
Nursing Diagnosis: Deficient Knowledge
Related to:
- Cognitive dysfunction
- Inadequate access to resources
- Inadequate awareness of resources
- Inadequate knowledge of resources
- Misinformation
- Neurobehavioral manifestations
As evidenced by:
- Inappropriate behavior
- Inaccurate statements about topics related to the condition
- Inaccurate follow-through of instructions
- Development of further complications
Expected outcomes:
- Patient and/or family will demonstrate knowledge about the condition, treatments, and prognosis as evidenced by verbalization of teaching instructions and adherence with follow-up activities.
Assessment:
1. Assess the patient’s cognitive ability.
Patients with TBI may exhibit disorientation, confusion, short-term memory loss, and mood changes. Determine cognition to tailor teaching methods for optimal effectiveness.
2. Assess the patient’s support system.
The patient’s support system is important to identify as those with severe TBI often require at a minimum, assistive care.
Interventions:
1. Encourage the patient to participate in developing a relevant treatment regimen.
This will let the patient feel a sense of control in their treatment regimen and likely result in the best outcomes.
2. Encourage the patient and family to participate in required therapies.
Rehabilitation may be indicated for patients after TBI to maximize return to the patient’s highest level of functioning. The patient’s family may be required to provide continuous support to the patient even after the patient is discharged.
3. Discuss possible changes in behavior, mood, and personality at home.
Personality and behavioral problems can develop after TBI. The family must be prepared to cope with the possible changes in the patient’s behavior, personality, and mood.
4. Discuss the importance of follow-up care.
Follow-up care is essential in ensuring the patients return to their highest level of functioning.
5. Instruct the family to develop a structured and consistent home routine.
Patients suffering from TBI respond best to a structured and consistent environment that does not deviate much from their normal routine.
Ineffective Breathing Pattern
A traumatic brain injury may cause the patient to exhibit breathing pattern alterations or respiratory distress.
Nursing Diagnosis: Ineffective Breathing Pattern
Related to:
- Brainstem impairment
- Altered level of consciousness
- Respiratory muscle weakness
- Acute respiratory distress syndrome
As evidenced by:
- Bradypnea
- Cyanosis
- Decreased inspiratory pressure
- Decreased expiratory pressure
- Irregular breathing patterns
- Shallow respirations
- Hypoventilation
- Hyperventilation
- Hypoxemia
- Hypoxia
- Nasal flaring
- Accessory muscle use
Expected outcomes:
- Patient will maintain arterial blood gases within an acceptable range.
- Patient will not require the use of mechanical ventilation.
Assessment:
1. Assess and monitor the patient’s respiratory rate, rhythm, and depth.
Note any alterations in breathing patterns such as irregularities like Cheyne-Stokes respirations, tachypnea, bradypnea, or shallow breathing.
2. Assess blood gas values and oxygen saturation.
A significant decline in the patient’s oxygen saturation and arterial blood gas values can indicate an ineffective breathing pattern and the development of respiratory complications.
3. Monitor for acute respiratory distress syndrome (ARDS).
Approximately 20% of patients will experience ARDS within a few days after a severe TBI, which increases the rate of mortality. The nurse should remain alert for symptoms of ARDS, such as dyspnea, cyanosis, altered mental status, and rales upon auscultation.
Interventions:
1. Position the patient with the head of the bed elevated 30-45 degrees.
Elevating the head of the bed can help reduce increased intracranial pressure in patients with TBI and, at the same time, promote lung expansion for optimal breathing.
2. Administer supplemental oxygen as indicated.
TBI can cause hypoxia, so oxygen supplementation is essential to reverse tissue hypoxia, enhance breathing patterns, and promote oxygen exchange.
3. Assist in providing ventilatory support.
Severe cases of TBI may require mechanical ventilation to help protect the airways, promote normal breathing patterns, and prevent hypoxemia.
4. Encourage breathing exercises and ambulation.
Breathing exercises, along with early ambulation, can significantly improve cardiorespiratory fitness after TBI.
Ineffective Cerebral Tissue Perfusion
Patients with TBI are susceptible to a decrease in cerebral tissue perfusion. As a result of brain injury, there may be swelling, bleeding, or CSF leaking affecting perfusion. Increased ICP occurs when the brain is not able to accommodate further volume changes, resulting in decreased cerebral perfusion, brain tissue ischemia, and edema. If cerebral edema is left untreated, the brainstem will herniate downward causing irreversible brain damage and death.
Nursing Diagnosis: Ineffective Tissue Perfusion
Related to:
- Hemorrhage
- Skull fractures
- Cerebral edema (localized or generalized response to injury)
- Decreased systemic blood pressure
- Hypoxia
As evidenced by:
- Mental status changes
- Decreased LOC
- Pupillary changes
- Changes in motor response
- Difficulty swallowing or speaking
Expected outcomes:
- Patient will maintain an expected level of consciousness, motor response, sensory function, and cognition.
- Patient will display adequate perfusion as evidenced by stable vital signs and hemodynamics.
Assessment:
1. Assess and obtain an accurate patient history.
Obtaining an accurate history from the patient suffering from TBI may be difficult depending on the severity of the brain injury. It can be obtained from witnesses of the injury or the first responders. It is essential to ask when, where, and how the injury occurred as this will help plan and formulate the most appropriate treatment regimen.
2. Assess and monitor neurological status frequently.
Changes in the patient’s level of consciousness can indicate complications. Monitoring changes in neurologic status and GCS in patients with TBI is vital because the patient’s condition can deteriorate rapidly, requiring emergency surgery.
3. Assess and monitor vital signs.
The mechanism of autoregulation is impaired following TBI. Severe TBI causes impairment in the function of the cerebral vasculature to modify systemic pressure to ensure sufficient blood flow to the brain. Blood pressure and pulse must be monitored frequently as the patient can exhibit hypotension or hypertension. Cushing’s triad (irregular respirations, widened pulse pressure, and bradycardia), a classic but late sign of increased ICP, indicates imminent brainstem herniation.
4. Evaluate diagnostic studies.
A CT scan is often ordered to identify the extent of the injury. This diagnostic procedure can help identify injuries such as hemorrhage requiring immediate surgical intervention. An MRI may be ordered to diagnose a diffuse axonal injury.
Interventions:
1. Evaluate and monitor pupillary responses.
It is essential to report any changes in pupil size, reactivity, and shape immediately as this can indicate an increase in the patient’s ICP. This assessment can also reveal specific areas of brain damage. Unresponsive pinpoint pupils indicate brainstem dysfunction while asymmetric pupils, dilated pupils, or loss of light reaction indicate brainstem herniation.
2. Monitor the patient’s bilateral motor responses.
Motor dysfunction in TBI often appears contralateral to the site of the injury. It is important to frequently monitor the motor responses of a patient with TBI because any form of deterioration in mobility and abnormal posture can indicate progressive brain injury.
3. Maintain head or neck in midline or neutral position.
Turning the head to one side tends to compress the jugular veins and impedes cerebral venous drainage, which can increase intracranial pressure. To keep the head in a neutral position, use rolled towels or pillows for support as needed.
4. Provide rest periods between care activities and limit the duration of procedures.
Continuous activities and unnecessary stimulation can increase intracranial pressure.
5. Administer IV fluids.
Perfusion can be supported by crystalloid and colloid IV fluids. Hypotonic and dextrose-containing fluids should be avoided. Some instances may require fluid to be restricted.
6. Administer supplemental oxygen as needed.
Providing supplemental oxygen can help reduce hypoxemia. Hypoxemia causes cerebral vasodilation and increased ICP, causing further damage to the brain tissue.
7. Administer medications as indicated.
Diuretics such as mannitol may be prescribed to reduce brain swelling, which helps improve cerebral blood flow and oxygenation.
8. Prepare for surgical intervention as indicated.
Craniotomy may be indicated to help remove bone fragments, elevate depressed fractures, control hemorrhage, evacuate hematoma, and debride necrotic tissues, relieving pressure.
Ineffective Thermoregulation
Hyperthermia and hypothermia are observed in patients following traumatic brain injury due to damage to the preoptic area of the hypothalamus, posttraumatic cerebral inflammation, and secondary infection.
Nursing Diagnosis: Ineffective Thermoregulation
Related to:
- Brain injury
- Inflammatory process
- Neurological impairment
- Secondary infection
- Increased oxygen demand
As evidenced by:
- Increased body temperature above the normal range
- Reduction in body temperature below the normal range
- Flushed skin
- Hypertension
- Increased respiratory rate
- Tachycardia
- Skin warm to touch
- Skin cool to the touch
- Seizures
Expected outcomes:
- Patient will maintain body temperature within normal range.
- Patient will not experience complications such as seizures from ineffective thermoregulation.
Assessment:
1. Assess and monitor the patient’s temperature
Assessment and monitoring of the patient’s body temperature using a consistent method of measurement can help determine developing complications and enable accurate treatment decisions.
2. Assess causative factors for ineffective thermoregulation.
Fever is common after a brain injury due to inflammation, damage to the hypothalamus, or an infectious process. Identifying the causative factor can help plan an appropriate treatment regimen.
3. Assess and monitor for complications.
Fever increases the risk for seizures and increased intracranial pressure (ICP) and is associated with poorer outcomes. ICP can be monitored using an internal catheter in the brain.
Interventions:
1. Administer antipyretics as indicated.
Tylenol can maintain a normothermic body temperature to prevent further brain damage.
2. Prevent overheating.
After a TBI, patients may be prone to heat sensitivity due to a damaged hypothalamus. Keep the patient cool by removing excess blankets and dressing in loose clothing. Apply cool cloths or ice packs as needed.
3. Adjust and monitor the room temperature.
Environmental factors can further aggravate hypothermia or hyperthermia. Since the patient cannot regulate their own body temperature, it is important to ensure the room is not too hot or cold.
4. Administer intravenous fluids as indicated.
Adequate hydration is essential in replacing fluid loss and in managing increased systemic requirements resulting from hyperthermia in patients after traumatic brain injury. Isotonic fluids are generally recommended to prevent further brain swelling.
Nursing Diagnoses and Rationales for Traumatic Brain Injury
1. Ineffective Cerebral Tissue Perfusion
Rationale: Traumatic Brain Injury (TBI) can result in hemorrhage, edema, and increased intracranial pressure, all of which compromise cerebral perfusion. Ensuring adequate oxygenation, monitoring intracranial pressure, and administering medications to reduce swelling are crucial to prevent further brain damage and promote recovery.
2. Risk for Infection
Rationale: Patients with TBI often have invasive devices such as intracranial pressure monitors, central lines, or endotracheal tubes, which increase the risk of infection. Adhering to strict aseptic techniques, monitoring for signs of infection, and administering prophylactic antibiotics can help prevent infections and complications.
3. Acute Pain
Rationale: TBI patients may experience headaches, neck pain, or pain from associated injuries. Pain management through analgesics, positioning for comfort, and providing a calm environment can alleviate pain and improve overall patient comfort.
4. Impaired Physical Mobility
Rationale: Neurological deficits, muscle weakness, and balance issues following TBI can impair mobility. Implementing physical therapy, ensuring a safe environment, and using assistive devices can help improve mobility and prevent falls or further injury.
5. Impaired Memory
Rationale: TBI can lead to memory loss, impacting the patient’s ability to retain new information or recall past events. Providing memory aids, creating a structured routine, and offering cognitive rehabilitative therapy can support memory function and enhance daily living activities.
6. Impaired Verbal Communication
Rationale: Patients with TBI may have difficulty expressing themselves due to cognitive or speech impairments. Utilizing speech therapy, encouraging alternative communication methods, and being patient and supportive can enhance communication abilities.
7. Risk for Aspiration
Rationale: Swallowing difficulties following TBI can increase the risk of aspiration. Conducting a thorough swallowing assessment, providing modified textures for food and liquids, and positioning the patient properly during meals can reduce aspiration risk and ensure safe nutrition.
8. Anxiety
Rationale: The uncertainty and potential long-term effects of TBI can cause significant anxiety for the patient and their family. Providing clear information, emotional support, and involving the patient and family in treatment decisions can help alleviate anxiety and promote a sense of control.
9. Risk for Imbalanced Nutrition
Rationale: Patients with TBI might have reduced appetite, difficulty swallowing, or increased metabolic demands, leading to nutritional imbalances. Consulting with a dietitian, monitoring dietary intake, and offering nutrient-dense meals can help meet nutritional needs and support recovery.
10. Ineffective Coping
Rationale: The emotional and psychological impact of TBI can hinder the patient’s ability to cope with their condition. Providing psychological support, offering counseling services, and involving mental health professionals can help the patient develop effective coping strategies and facilitate emotional healing.
11. Deficient Knowledge
Rationale: Patients and their families may lack understanding of TBI, its potential complications, and the recovery process. Educating them about the condition, demonstrating self-care techniques, and providing written and verbal instructions for home care are essential to ensure safe and effective recovery.
12. Fatigue
Rationale: The physical and mental exertion required to recover from TBI can lead to significant fatigue. Encouraging rest, clustering nursing care to minimize energy expenditure, and gradually increasing activity levels as tolerated can help manage fatigue and support recovery.
13. Sensory-Perceptual Alterations
Rationale: TBI can affect the patient’s sensory perception, such as vision, hearing, or balance. Conducting regular sensory assessments, providing appropriate sensory aids, and creating a safe environment can help manage these alterations and prevent injury.
14. Risk for Post-Traumatic Seizures
Rationale: TBI increases the risk of seizures due to potential brain damage. Monitoring for seizure activity, administering anticonvulsant medications as prescribed, and educating the patient and family on seizure precautions can help manage this risk and ensure safety.
15. Interrupted Family Processes
Rationale: The impact of TBI on the patient can disrupt family dynamics and roles. Providing family-centered care, offering support services, and facilitating open communication can help the family adjust and support the patient’s recovery.
REFERENCES
- Dawodu, S. T. (2023, September 25). Traumatic brain injury (TBI) – Definition, epidemiology, pathophysiology. Diseases & Conditions – Medscape Reference. https://emedicine.medscape.com/article/326510-overview#a3
- Geroges, A., & Das, J. M. (2023, January 2). Traumatic brain injury – StatPearls – NCBI bookshelf. National Center for Biotechnology Information. https://www.ncbi.nlm.nih.gov/books/NBK459300/
- Loewen, J. (2023, January 23). Why concussion can lead to blood pressure change & POTS. Cognitive FX | Post Concussion Syndrome Treatment. https://www.cognitivefxusa.com/blog/pots-and-concussion-blood-pressure-changes
- Lewis’s Medical-Surgical Nursing. 11th Edition, Mariann M. Harding, RN, PhD, FAADN, CNE. 2020. Elsevier, Inc.
- Lizzo JM, Waseem M, Tatikonda G. Brain Trauma (Nursing) [Updated 2022 May 2]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK568686/
- Medical-Surgical Nursing: Concepts for Interprofessional Collaborative Care. 9th Edition. Donna D. Ignatavicius, MS, RN, CNE, ANEF. 2018. Elsevier, Inc.
- Nakase-Richardson, R., Yablon, S. A., & Sherer, M. (2007). Prospective comparison of acute confusion severity with duration of post-traumatic amnesia in predicting employment outcome after traumatic brain injury. Journal of neurology, neurosurgery, and psychiatry, 78(8), 872–876. https://doi.org/10.1136/jnnp.2006.104190
- Posti, J. P., Takala, R. S., & Tenovuo, O. (2019). TBIcare investigators’ response to papa and Wang (DOI: 10:1089/neu.2017.5030): Raising the bar for traumatic brain injury biomarker research: Methods make a difference. Journal of Neurotrauma, 36(10), 1680-1681. https://doi.org/10.1089/neu.2017.5209
- Shaikh F, Waseem M, Boling AM. Head Trauma (Nursing) [Updated 2021 Nov 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; https://www.ncbi.nlm.nih.gov/books/NBK568699/
- TBI among service members and veterans. (2023, October 16). Centers for Disease Control and Prevention. https://www.cdc.gov/traumaticbraininjury/military/index.html
- Traumatic Brain Injury. Cleveland Clinic. © 2022 Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/8874-traumatic-brain-injury
- Traumatic Brain Injury. The Johns Hopkins University, The Johns Hopkins Hospital, and Johns Hopkins Health System. Copyright © 2022. https://www.hopkinsmedicine.org/health/conditions-and-diseases/traumatic-brain-injury
- Traumatic Brain Injury & Concussion. Centers for Disease Control and Prevention. https://www.cdc.gov/traumaticbraininjury/index.html
- Traumatic brain injury (TBI): What is it, causes, types. (2021, November 1). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/8874-traumatic-brain-injury
- Traumatic brain injury. (2021, February 4). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/traumatic-brain-injury/symptoms-causes/syc-20378557
- Traumatic brain injury. (2021, February 4). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/traumatic-brain-injury/diagnosis-treatment/drc-20378561
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.







