A right‑to‑left cardiac shunt scan is a nuclear medicine test used to detect abnormal blood flow from the right to the left side of the heart. It helps diagnose congenital heart defects, evaluate hypoxemia, and guide cardiology management through precise shunt quantification.
Introduction
The evaluation of cardiac shunts forms a cornerstone in the diagnosis and management of congenital and acquired heart diseases. A right to left (R-L) cardiac shunt refers to the abnormal passage of blood from the right side of the heart to the left, bypassing the pulmonary circulation. The right to left cardiac shunt scan is a diagnostic procedure designed to identify and quantify such shunts, providing crucial information for clinical decision-making.
Pathophysiology of Right to Left Cardiac Shunt
Mechanisms
A right to left cardiac shunt occurs when blood flows directly from the right atrium or ventricle to the left atrium or ventricle, bypassing the lungs. This abnormal flow can result from structural defects such as atrial septal defects (ASD), ventricular septal defects (VSD), patent foramen ovale (PFO), or more complex congenital anomalies like Eisenmenger syndrome. The shunted blood, being deoxygenated, mixes with oxygenated blood in the systemic circulation, leading to varying degrees of hypoxaemia.
Clinical Implications
The presence of a significant R-L shunt can manifest clinically as cyanosis, exercise intolerance, digital clubbing, and paradoxical embolism. Chronic hypoxaemia may result in secondary erythrocytosis and end-organ dysfunction. Early and accurate identification of the shunt is vital for timely intervention, risk stratification, and prevention of complications such as stroke, brain abscess, and pulmonary hypertension.
Indications for the Procedure
Patient Selection
A right to left cardiac shunt scan is indicated in patients where there is clinical suspicion or evidence of a shunt. Common clinical scenarios include:
- Unexplained cyanosis, particularly in young children or adults with no apparent pulmonary disease
- Paradoxical embolic events, such as cryptogenic stroke
- Preoperative evaluation in patients undergoing surgery for congenital heart disease
- Assessment of patients with known congenital heart defects for quantification of shunt severity
- Investigation of unexplained hypoxaemia or polycythaemia
Common Conditions
- Patent foramen ovale (PFO)
- Atrial septal defect (ASD)
- Ventricular septal defect (VSD) with Eisenmenger physiology
- Complex congenital heart diseases (e.g., Tetralogy of Fallot, Transposition of the great arteries)
- Pulmonary arteriovenous malformations
Preparation for the Scan
Patient Preparation
Patient preparation is essential to ensure optimal scan quality and patient safety. Key steps include:
- Informed consent: Explain the procedure, risks, and benefits to the patient or guardian.
- Fasting: Some protocols require fasting for 4–6 hours before the scan, especially when sedation is needed.
- Medication review: Assess for medications that may interfere with the scan, such as anticoagulants or contrast allergies.
- IV access: Secure a reliable intravenous line for radionuclide or contrast administration.
- Baseline assessment: Record vital signs, oxygen saturation, and obtain a detailed medical history.
Contraindications
- Known allergy to contrast or radiopharmaceutical agents (for radionuclide scans)
- Severe renal dysfunction (for certain contrast studies)
- Unstable clinical condition or decompensated heart failure
- Pregnancy (relative contraindication for radionuclide scans)
Diagnostic Techniques
Types of Scans
Multiple imaging modalities are available for the detection and quantification of R-L shunts. The choice depends on the clinical context, patient characteristics, and available resources.
- Echocardiography
- Transthoracic Echocardiography (TTE): Non-invasive, first-line imaging for structural assessment. Agitated saline contrast (bubble study) enhances detection of shunts.
- Transoesophageal Echocardiography (TOE/TEE): Provides superior visualisation of interatrial septum and small shunts, especially in adults.
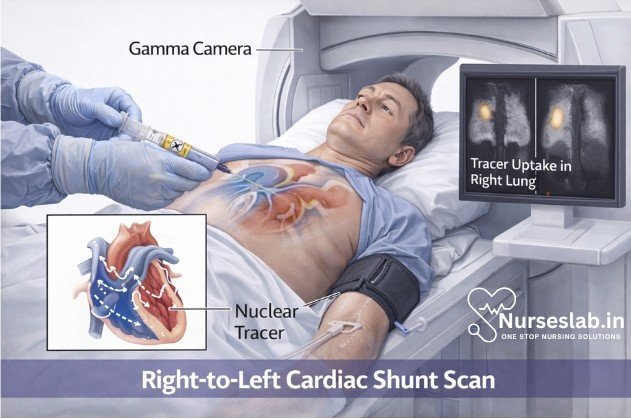
- Radionuclide Perfusion Scans
- Involves intravenous injection of radiolabelled particles (e.g., Technetium-99m macroaggregated albumin, Tc-99m MAA). Detection of systemic distribution indicates R-L shunt.
- Cardiac Magnetic Resonance Imaging (MRI)
- Provides detailed anatomical and functional assessment, quantifies shunt fraction (Qp:Qs), and detects associated anomalies.
- Computed Tomography (CT) Angiography
- High-resolution imaging of cardiac and pulmonary vasculature, useful for detecting pulmonary AVMs.
Equipment Used
- Echocardiography machines with Doppler and contrast capabilities
- Gamma cameras for radionuclide scans
- MRI and CT scanners with cardiac imaging protocols
- Ancillary equipment: intravenous lines, monitoring devices, resuscitation equipment
Procedure Steps
Step-by-Step Methodology
1. Echocardiographic Bubble Study
- Position the patient in the left lateral decubitus position.
- Apply ECG leads for cardiac monitoring.
- Obtain baseline echocardiographic images to assess cardiac anatomy.
- Prepare agitated saline by mixing 9 mL saline with 1 mL air (and optionally a drop of the patient’s blood) in two syringes connected by a three-way stopcock.
- Inject the agitated saline rapidly through a peripheral IV line while imaging the right atrium.
- Observe for microbubble appearance in the left atrium/ventricle within 3–5 cardiac cycles, indicating R-L shunt; delayed appearance suggests pulmonary AVM.
- Record and store images for quantitative analysis.
2. Radionuclide Perfusion Scan (Tc-99m MAA)
- Confirm patient identity and obtain informed consent.
- Establish intravenous access and monitor vital signs.
- Inject the calculated dose of Tc-99m MAA intravenously.
- Acquire images using a gamma camera, focusing on the lungs, brain, kidneys, and liver.
- Systemic uptake (e.g., in the brain or kidneys) indicates presence of a R-L shunt.
- Quantify the shunt fraction by comparing counts in the lungs versus systemic organs.
3. Cardiac MRI/CT
- Screen for contraindications (e.g., metal implants, renal function for contrast).
- Position the patient and apply ECG gating leads.
- Administer contrast agent (if required).
- Acquire sequences in multiple planes to visualise septal defects and quantify shunt fraction.
- Analyse images for anatomical and functional assessment.
Interpretation of Results
Reading Scan Findings
Interpretation requires a systematic approach, integrating imaging findings with clinical context.
- In echocardiography, immediate appearance of microbubbles in the left chambers after right atrial opacification confirms an intracardiac R-L shunt.
- Delayed appearance (after 3–8 cardiac cycles) suggests a pulmonary shunt (e.g., AVM).
- Radionuclide scans: Any systemic uptake beyond the lungs (notably in the brain, kidneys, or spleen) is diagnostic of a R-L shunt.
- Shunt fraction (Qp:Qs ratio) quantifies the magnitude; a Qp:Qs < 1 indicates predominant right to left flow.
- MRI and CT provide anatomical localisation and functional quantification.
Common Patterns and Quantification
Quantification is essential for risk stratification and management planning:
- Small shunt: Minimal clinical impact; often managed conservatively.
- Moderate shunt: May require intervention depending on symptoms and risk of complications.
- Large shunt: Associated with severe hypoxaemia, risk of paradoxical embolism; usually requires closure or surgical correction.
Quantitative radionuclide scan: Shunt fraction (%) = (Counts in systemic organs) / (Total counts in lungs + systemic organs) × 100.
Clinical Significance
The detection and quantification of a right to left cardiac shunt have significant implications for patient management:
- Guides the decision for surgical or percutaneous closure of the defect
- Assists in risk assessment for paradoxical embolism and stroke
- Informs the need for endocarditis prophylaxis and anticoagulation in selected patients
- Monitors response to therapy and disease progression
- Provides prognostic information, especially in complex congenital heart disease
Early intervention in significant shunts can prevent irreversible complications like pulmonary hypertension and Eisenmenger syndrome, improving long-term outcomes and quality of life.
Potential Complications
- Allergic reactions: To contrast or radiopharmaceutical agents, although rare
- Vascular complications: Phlebitis, haematoma at injection site
- Arrhythmias: Particularly during echocardiography in susceptible patients
- Systemic embolisation: Theoretical risk when injecting particulate agents in patients with large shunts (hence, careful dose calculation and technique are mandatory)
- Radiation exposure: Minimal but relevant in paediatric and pregnant populations
- Contrast nephropathy: With CT/MRI contrast in patients with renal impairment
- Anxiety or claustrophobia: Especially during MRI or CT procedures
Mitigation strategies include thorough patient screening, adherence to protocol, use of minimal effective doses, and immediate availability of resuscitation facilities.
Nursing Care of Patients Undergoing Right to Left Cardiac Shunt Scan Diagnostic Procedure
The diagnosis and evaluation of right-to-left cardiac shunts are crucial for appropriate clinical management, and nurses play an essential role in the care of patients undergoing this procedure.
Nursing Responsibilities and Roles
Nurses are integral to the multidisciplinary team managing patients undergoing a right-to-left cardiac shunt scan. Key responsibilities include:
- Patient assessment and identification of indications and contraindications for the scan.
- Patient preparation, including education, consent, and physical preparation.
- Monitoring and supporting the patient during the procedure.
- Post-procedural care, including observation for immediate and delayed complications.
- Documentation and communication with the healthcare team.
Pre-Procedure Nursing Care
Patient Assessment
Before the procedure, a thorough assessment is vital. The nurse should:
- Review the patient’s medical history, focusing on cardiac conditions, previous surgeries, allergies (especially to radiopharmaceuticals), and current medications.
- Assess baseline vital signs, oxygen saturation, and the presence of any signs of hypoxemia, such as cyanosis or clubbing.
- Evaluate the patient’s understanding of the procedure and address any concerns or misconceptions.
- Ensure all required laboratory results (e.g., renal function tests, coagulation profile) are available and within acceptable limits.
Patient Education and Consent
Providing comprehensive information about the procedure alleviates anxiety and ensures cooperation. Education should include:
- Explanation of the purpose and steps of the shunt scan, including the use of a radioactive tracer and gamma camera imaging.
- Discussion of potential sensations (e.g., minor discomfort during IV insertion, possible warmth from the tracer injection).
- Reassurance regarding the safety of the tracer and radiation exposure, which is minimal and generally well-tolerated.
- Instructions regarding fasting status or medication adjustments, if required by the facility protocol.
- Obtaining and witnessing informed consent, ensuring the patient or legal guardian understands the risks, benefits, and alternatives.
Physical Preparation
Physical preparation includes:
- Ensuring the patient is appropriately attired in a hospital gown and has removed any jewelry or metal objects that may interfere with imaging.
- Establishing reliable intravenous access for tracer administration.
- Confirming the patient’s identity and procedure details in accordance with the facility’s safety protocols (e.g., time-out procedure).
- Ensuring emergency equipment (e.g., oxygen, suction, resuscitation cart) is readily available in case of an adverse reaction.
Intra-Procedure Nursing Care
Assisting with Tracer Administration
The nurse assists the nuclear medicine technologist or physician in administering the radiopharmaceutical. Responsibilities include:
- Verifying the correct tracer, dose, and patient identity before administration.
- Observing for immediate adverse reactions, such as allergic responses, and initiating appropriate interventions if necessary.
- Documenting the time, dose, and site of injection.
Monitoring During Imaging
During the imaging phase, the nurse should:
- Monitor the patient’s vital signs, oxygen saturation, and level of consciousness, especially in patients with severe cyanosis or compromised cardiopulmonary status.
- Provide emotional support and reassurance, as the patient may need to remain still for extended periods.
- Assist in positioning the patient as required for optimal imaging, while ensuring comfort and safety.
- Be prepared to respond to any acute complications, such as hypoxemia, vasovagal episodes, or anxiety attacks.
Post-Procedure Nursing Care
Immediate Post-Scan Care
After the scan, the nurse should:
- Monitor the patient for any delayed reactions to the tracer, such as rash, shortness of breath, or hypotension.
- Assess the IV site for signs of infiltration or phlebitis and remove the cannula if no longer needed.
- Reassess vital signs and oxygen saturation, comparing them to pre-procedure values.
- Encourage oral hydration, as appropriate, to promote tracer elimination from the body.
- Inform the patient about the expected duration of radioactivity in the body and any required precautions (usually minimal for this procedure).
Observation for Complications
While complications are rare, nurses should be vigilant for:
- Allergic or anaphylactic reactions to the radiopharmaceutical.
- Worsening hypoxemia, especially in patients with severe right-to-left shunts.
- Signs of infection or thrombophlebitis at the IV site.
- Vasovagal episodes or anxiety-induced symptoms.
Prompt identification and management of complications are critical for patient safety.
Documentation and Communication
Comprehensive documentation is essential for continuity of care and medico-legal purposes. The nurse should record:
- Pre-procedure assessment findings, including baseline vital signs and patient education provided.
- Details of tracer administration: type, dose, time, and site.
- Any intra-procedural events or patient responses.
- Post-procedure observations, interventions, and patient education.
- Communication with the physician or other team members regarding abnormal findings or complications.
Patient Discharge and Education
Once the procedure is completed and the patient is stable, the nurse should provide discharge instructions, including:
- Advising the patient to maintain adequate hydration to facilitate excretion of the tracer.
- Instructing on signs and symptoms that require immediate medical attention, such as difficulty breathing, chest pain, or severe rash.
- Clarifying any activity restrictions or follow-up appointments, as directed by the physician.
- Reinforcing the importance of adherence to the overall management plan for their underlying cardiac condition.
Special Considerations
Pediatric Patients
Care of children undergoing right-to-left shunt scans requires additional considerations:
- Use age-appropriate language and visual aids to explain the procedure.
- Involve parents or guardians in the preparation and support of the child.
- Consider sedation if necessary, following strict protocols and monitoring.
Patients with Cognitive Impairment
For patients with cognitive deficits or communication barriers:
- Use simple instructions and non-verbal cues to enhance understanding.
- Involve family members or carers in the process.
- Monitor closely for signs of distress or agitation during the procedure.
Ethical and Legal Considerations
Nurses must ensure that patient autonomy and confidentiality are respected throughout the care process. Informed consent must be obtained before the procedure, and all information should be provided in a manner that the patient can understand. Cultural, religious, and personal beliefs should be acknowledged and accommodated whenever possible.
REFERENCES
- March of Dimes. Congenital Heart Defects and Critical CHDs https://www.marchofdimes.org/complications/congenital-heart-defects.aspx.
- Radiopaedia. Cardiovascular shunts https://radiopaedia.org/articles/cardiovascular-shunts?lang=us.
- Shahjehan RD, Abraham J. Intracardiac Shunts https://www.ncbi.nlm.nih.gov/books/NBK558969. [Updated 2021 Oct 11]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-.
- Lu H, Zhang D, Fu H, Chen T, Li F, Liu T, Liu C. Apical Left Ventricular Pseudoaneurysm With Left-to-Right Shunt: A Rare Mechanical Complication of Myocardial Infarction Involving Both Ventricles. Echocardiography. 2026 Feb;43(2):e70410. doi: 10.1111/echo.70410. PMID: 41677421.
- Boussell, L., Douek, P., Elicker, B. (2009). Right-to-Left Shunts. In: Rémy-Jardin, M., Rémy, J. (eds) Integrated Cardiothoracic Imaging with MDCT. Medical Radiology. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-540-72387-5_23
- Torigoe T, Mawad W, Seed M, et al. Treatment of fetal circular shunt with non-steroidal anti-inflammatory drugs https://obgyn.onlinelibrary.wiley.com/doi/full/10.1002/uog.20169. Ultrasound Obstet Gynecol. 2018;(53)6:841-46.
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





