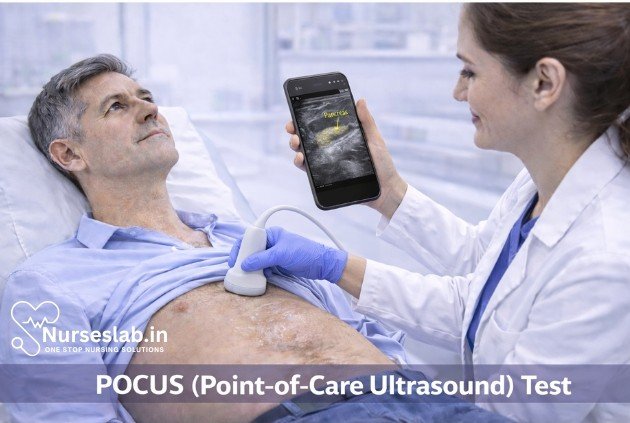
POCUS (Point‑of‑Care Ultrasound) is a bedside imaging tool that provides real‑time evaluation of cardiac, lung, abdominal, and vascular conditions. It enhances rapid diagnosis, guides procedures, and improves clinical decision‑making in emergency and critical‑care settings.
Introduction
Point-of-Care Ultrasound (POCUS) has transformed the landscape of modern medicine by providing clinicians with real-time, bedside diagnostic imaging capabilities. Unlike traditional radiology-based ultrasound, POCUS is performed and interpreted directly by the treating physician, allowing for immediate integration of findings into clinical decision-making.
Principles of POCUS
Basic Ultrasound Physics
Ultrasound imaging relies on high-frequency sound waves, typically between 2 and 15 MHz, transmitted into the body via a transducer (probe). These waves interact with tissues and organs, producing echoes that are received by the transducer and processed into visual images. The degree of sound wave reflection, refraction, and absorption depends on the acoustic properties of the tissues encountered. Key concepts include:
- Frequency: Higher frequencies yield better resolution but limited depth penetration; lower frequencies penetrate deeper but with reduced resolution.
- Echoes: Structures that reflect more sound waves (e.g., bone, air) appear brighter (hyperechoic), while those that absorb or transmit waves (e.g., fluid) appear darker (hypoechoic or anechoic).
- Artifacts: Recognising common ultrasound artifacts is essential for accurate interpretation; these include shadowing, enhancement, and reverberation.
Equipment and Image Acquisition
POCUS systems range from handheld devices to cart-based machines. Essential components include the transducer, display screen, and software for image optimisation. Selecting the appropriate probe is crucial:
- Linear probes (high-frequency, 7–15 MHz): Ideal for vascular, musculoskeletal, and superficial structures.
- Curvilinear probes (moderate frequency, 2–5 MHz): Suited for abdominal and obstetric imaging.
- Phased array probes (lower frequency, 1–5 MHz): Commonly used for cardiac and thoracic applications.
Image acquisition involves positioning the probe over the area of interest, optimising settings (gain, depth, focus), and systematically scanning to obtain diagnostic views.
Clinical Applications of POCUS
POCUS is employed across a multitude of medical specialties, providing rapid diagnostic information and guiding interventions. Its versatility has made it indispensable in:
Emergency Medicine
In emergency departments, POCUS facilitates the assessment of trauma (e.g., FAST exam for internal bleeding), cardiac function, pericardial effusion, pneumothorax, and vascular access. It enables timely management of life-threatening conditions.
Critical Care
Intensive care units use POCUS for evaluating shock, guiding resuscitation, monitoring fluid status, and detecting complications such as pleural effusions or deep vein thrombosis.
Internal Medicine
POCUS supports the diagnosis of ascites, biliary pathology, renal obstruction, and aids in procedures like paracentesis and thoracentesis.
Other Specialties
Applications extend to paediatrics (e.g., congenital heart disease screening), obstetrics (e.g., fetal viability), anaesthesia (e.g., nerve blocks), and rheumatology (e.g., joint effusions).
Diagnostic Techniques
Step-by-Step Guide for Common POCUS Examinations
Below are outlined techniques for several high-yield POCUS exams:
Cardiac Assessment (Focused Cardiac Ultrasound)
- Patient Preparation: Position the patient supine or slightly left lateral.
- Probe Selection: Use a phased array probe.
- Scanning Protocol: Obtain standard views—parasternal long axis, parasternal short axis, apical four-chamber, subcostal.
- Image Interpretation: Assess global contractility, chamber size, pericardial effusion, valvular function.
Abdominal Assessment (FAST Exam)
- Patient Preparation: Supine position; expose abdomen.
- Probe Selection: Curvilinear probe.
- Scanning Protocol: Survey four regions—right upper quadrant (Morrison’s pouch), left upper quadrant (splenorenal recess), pelvis (Douglas pouch), pericardium.
- Image Interpretation: Identify free fluid, organ injury, hemoperitoneum.
Pulmonary Assessment
- Patient Preparation: Upright or supine.
- Probe Selection: Linear or curvilinear probe.
- Scanning Protocol: Examine anterior, lateral, and posterior chest.
- Image Interpretation: Detect pneumothorax (absence of lung sliding), pleural effusion (anechoic fluid), consolidation, interstitial syndrome.
Vascular Assessment
- Patient Preparation: Expose region of interest.
- Probe Selection: Linear probe.
- Scanning Protocol: Compress veins to assess patency; visualise arteries for flow and occlusion.
- Image Interpretation: Identify DVT, arterial occlusion, vascular anomalies.
Other Techniques
Additional examinations include gallbladder (cholecystitis), kidneys (hydronephrosis), bladder (retention), and musculoskeletal (joint effusion, tendon rupture). Each follows similar preparation, probe selection, scanning sequence, and interpretation.
Procedure Steps
Patient Preparation
Successful POCUS begins with appropriate patient positioning, exposure of the area to be examined, and explanation of the procedure to ensure cooperation and comfort. Consider infection control measures, such as probe covers and gel application.
Probe Selection and Handling
Choosing the right probe based on target anatomy is critical for image quality. Hold the probe gently, stabilise your hand, and maintain consistent contact with the skin. Adjust orientation markers to match anatomical planes.
Scanning Protocols
Adhere to established protocols for each examination type to ensure comprehensive assessment and reproducibility. Systematic scanning reduces missed findings and enhances diagnostic accuracy.
Image Interpretation
Interpretation requires understanding normal anatomy, recognising pathological findings, and differentiating artifacts from true pathology. Documentation of images and relevant measurements is essential for clinical communication and follow-up.
Benefits of POCUS
- Rapid Diagnosis: POCUS provides immediate answers at the bedside, reducing delays associated with traditional imaging.
- Bedside Accessibility: Portability allows use in diverse settings—wards, emergency rooms, ambulances, remote clinics.
- Improved Patient Outcomes: Early detection of critical conditions enables timely intervention, often improving morbidity and mortality.
- Guidance for Procedures: Enhances safety and success rates for invasive procedures like central line placement, thoracentesis, and nerve blocks.
- Cost-Effective: Reduces reliance on more expensive imaging modalities and minimises patient transport risks.
- Patient Engagement: Real-time imaging fosters patient understanding and shared decision-making.
Limitations and Challenges
- Operator Dependency: Image acquisition and interpretation are highly skill-dependent; novice users may miss or misinterpret findings.
- Technical Limitations: Obesity, subcutaneous emphysema, and wound dressings can impair image quality.
- Potential Pitfalls: Artifacts, limited field of view, and over-reliance on POCUS without correlation to clinical context may lead to diagnostic errors.
- Scope of Use: POCUS is not a substitute for comprehensive radiology studies when complex pathology is suspected.
- Documentation and Integration: Ensuring proper documentation and integration into the medical record is essential to maintain quality and continuity of care.
Training and Competency
Effective use of POCUS demands structured training, supervised practice, and ongoing competency assessment. Key aspects include:
- Skill Acquisition: Foundational training in ultrasound physics, anatomy, and hands-on scanning techniques.
- Certification: Formal certification is available through professional bodies (e.g., American College of Emergency Physicians, European Society of Emergency Medicine).
- Ongoing Education: Regular workshops, simulation labs, and peer-reviewed assessments ensure skill maintenance and advancement.
- Mentorship: Access to experienced practitioners for feedback and guidance accelerates learning curves.
POCUS competency is often evaluated through objective structured clinical examinations (OSCEs), image review portfolios, and direct observation.
Case Studies and Examples
The following real-world scenarios illustrate the utility of POCUS:
- Case 1: Trauma FAST Exam
- A 34-year-old male presents following a motor vehicle collision with hypotension. POCUS reveals free fluid in Morrison’s pouch, expediting surgical intervention for intra-abdominal bleeding.
- Case 2: Cardiac Tamponade
- In the intensive care unit, a patient with shock is found to have a large pericardial effusion with right ventricular collapse on subcostal cardiac POCUS, prompting emergent pericardiocentesis.
- Case 3: Pulmonary Embolism
- Bedside vascular ultrasound in a breathless patient identifies a non-compressible femoral vein consistent with deep vein thrombosis, supporting the diagnosis of pulmonary embolism.
- Case 4: Guiding Central Venous Access
- POCUS is used to visualise the internal jugular vein, increasing the success rate and safety of central line placement.
- Case 5: Biliary Disease
- A patient with right upper quadrant pain undergoes POCUS, which reveals gallstones and sonographic Murphy’s sign, confirming acute cholecystitis.
Best Practices and Recommendations
To maximise the benefits and minimise risks associated with POCUS, clinicians should adhere to the following best practices:
- Follow Protocols: Use standardised scanning protocols and checklists for each examination type.
- Maintain Documentation: Record images and findings in the patient’s medical record, noting limitations and clinical context.
- Correlate Clinically: Integrate POCUS findings with history, examination, and other investigations.
- Recognise Limitations: Be aware of technical and interpretive limitations, seeking further imaging when necessary.
- Engage in Continuous Learning: Participate in ongoing education, attend workshops, and seek mentorship.
- Ensure Patient Safety: Apply infection control measures and monitor for adverse events during procedures.
- Promote Interdisciplinary Collaboration: Work with radiologists, sonographers, and other specialists for complex cases.
Nursing Care of Patients Undergoing POCUS (Point-of-Care Ultrasound) Procedures
Nurses play a pivotal role in the safe and efficient delivery of POCUS, from preparation to aftercare, ensuring both patient comfort and procedural efficacy.
Nursing Responsibilities in POCUS Procedures
Nurses are integral to the success of POCUS procedures. Their responsibilities span patient preparation, intra-procedural assistance, monitoring, documentation, and post-procedural care. Below is a detailed overview of nursing care at each stage of the POCUS process.
1. Pre-Procedure Nursing Care
- Patient Education and Consent:
- Explain the purpose, benefits, and steps of the POCUS procedure to the patient and their family to alleviate anxiety and foster cooperation.
- Address concerns regarding discomfort, risks, and expected outcomes.
- Ensure informed consent is obtained where required, following institutional protocols.
Assessment and Preparation:
- Review the patient’s medical history, allergies (especially to ultrasound gel or latex), and any contraindications.
- Assess the patient’s physical and psychological readiness, including pain levels and anxiety.
- Ensure the patient’s privacy and dignity by providing appropriate draping and minimizing unnecessary exposure.
Equipment Preparation:
- Check the functionality and cleanliness of the ultrasound machine and transducers.
- Prepare necessary supplies: ultrasound gel, gloves, sterile covers (if needed), and cleaning materials.
- Ensure the machine is plugged in or adequately charged and presets are selected according to the examination type.
Environmental Preparation:
- Arrange a safe, comfortable, and accessible environment for both patient and operator.
- Adjust lighting as required for optimal screen visibility.
2. Intra-Procedure Nursing Care
Patient Positioning and Comfort:
- Assist in positioning the patient according to the specific POCUS application (e.g., supine for abdominal scans, left lateral decubitus for cardiac imaging).
- Support the patient with pillows or foam wedges to maintain comfort and stability during the procedure.
- Monitor for signs of discomfort or distress, intervening as needed.
Aseptic Technique and Infection Control:
- Maintain hand hygiene before and after contact with the patient and equipment.
- Use gloves and sterile probe covers when indicated, especially for invasive procedures (e.g., vascular access, pericardiocentesis).
- Apply ultrasound gel in a manner that avoids contamination and excess application.
- Ensure the equipment and surrounding area are kept clean and organized to minimize infection risk.
Assistance During Procedure:
- Hand over equipment and supplies as needed, maintaining a sterile field for invasive procedures.
- Monitor the patient’s vital signs and comfort level, especially during longer or more invasive scans.
- Communicate clearly with the clinician performing the POCUS, anticipating needs and responding promptly to requests.
- Support the patient emotionally, providing reassurance and updates as appropriate.
3. Post-Procedure Nursing Care
Patient Care and Monitoring:
- Assist the patient in returning to a comfortable position post-procedure.
- Clean residual gel from the patient’s skin and ensure their clothing and bedding are clean and dry.
- Monitor for any immediate complications, such as skin irritation, allergic reactions, or procedural complications (e.g., bleeding after vascular access).
Equipment Cleaning and Maintenance:
- Disinfect the ultrasound probe and machine surfaces according to infection control policies.
- Dispose of single-use items appropriately and restock supplies for future use.
- Document any equipment malfunctions or supply shortages for follow-up.
Documentation:
- Record the procedure, including date, time, type of scan, indications, findings (if applicable), and patient tolerance.
- Document any adverse reactions or complications and the interventions provided.
- Communicate relevant findings and observations to the healthcare team, ensuring continuity of care.
Patient Education and Follow-Up:
- Inform the patient of any post-procedure care instructions, such as monitoring for delayed reactions or when to report symptoms.
- Schedule or coordinate follow-up appointments or additional investigations as ordered by the clinician.
Special Considerations in POCUS Nursing Care
Pediatric Patients
Children undergoing POCUS may require additional support due to anxiety, fear, or inability to remain still. Nurses should use age-appropriate communication, involve parents or caregivers, and employ distraction techniques such as toys or videos. Sedation may sometimes be required, necessitating close monitoring.
Geriatric Patients
Older adults may have mobility limitations, fragile skin, or cognitive impairments. Extra care should be taken with positioning and skin protection. Clear, simple explanations and a calm demeanor help build trust and cooperation.
Patients with Disabilities
Adaptations may be needed for patients with physical or sensory disabilities. Collaborate with the patient and their support persons to optimize comfort and communication, and ensure accessibility of equipment and environment.
Infection Control in High-Risk Settings
In settings with high infection risk (e.g., during outbreaks of communicable diseases), strict adherence to infection prevention protocols is crucial. This includes the use of dedicated machines for infected patients, enhanced cleaning procedures, and appropriate personal protective equipment (PPE).
Emotional and Psychological Support
POCUS procedures can be stressful, especially when associated with acute illness or invasive interventions. Nurses should provide empathetic communication, address fears and misconceptions, and advocate for the patient’s comfort and dignity throughout the process.
Interdisciplinary Collaboration
Effective POCUS care requires close collaboration between nurses, physicians, sonographers, and other healthcare professionals. Nurses act as patient advocates, ensuring that concerns are communicated and that care is coordinated seamlessly across disciplines.
Documentation and Quality Assurance
Accurate and thorough documentation is essential for legal, clinical, and quality improvement purposes. Nurses should ensure that all aspects of the procedure, including patient preparation, intra-procedural events, and post-procedure outcomes, are recorded in the patient’s medical record. Participation in quality assurance initiatives, such as audits and feedback sessions, helps maintain high standards of care.
Education and Competency
Nurses involved in POCUS procedures should receive regular education and competency assessment related to equipment operation, infection control, patient safety, and procedure-specific protocols. Ongoing professional development ensures that nurses remain current with best practices and emerging technologies in POCUS.
Ethical and Legal Considerations
Nurses must practice within their scope and adhere to institutional policies regarding POCUS. They should respect patient autonomy, privacy, and confidentiality at all times, obtaining informed consent and safeguarding patient information. If a nurse encounters findings outside their expertise, they should promptly escalate to the appropriate clinician.
REFERENCES
- Perez-Sanchez, A., Johnson, G., Pucks, N. et al. Comparison of 6 handheld ultrasound devices by point-of-care ultrasound experts: a cross-sectional study. Ultrasound J 16, 45 (2024). https://doi.org/10.1186/s13089-024-00392-3
- Carrera KG, Hassen G, Camacho-Leon GP, Rossitto F, Martinez F, Debele TK. The Benefits and Barriers of Using Point-of-Care Ultrasound in Primary Healthcare in the United States (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9508689/). Cureus. 2022 Aug 25;14(8):e28373.
- Fraleigh CDM, Duff E. Point-of-care ultrasound: An emerging clinical tool to enhance physical assessment https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9301985/. Nurse Pract. 2022 Aug 1;47(8):14-20.
- Hashim A, Tahir MJ, Ullah I, Asghar MS, et al. The utility of point of care ultrasonography (POCUS) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8606703/ . Ann Med Surg (Lond). 2021 Nov 2;71:102982.
- Hsieh A, Baker MB, Phalen JM, Mejias-Garcia J, et al. Handheld Point-of-Care Ultrasound: Safety Considerations for Creating Guidelines https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9393648/. J Intensive Care Med. 2022 Sep;37(9):1146-1151.
- Pai VV, Noh CY, Dasani R, Vallandingham S, Manipon C, et al. Implementation of a Bedside Point-of-Care Ultrasound Program in a Large Academic Neonatal Intensive Care Unit https://pubmed.ncbi.nlm.nih.gov/35691294/ . Am J Perinatol. 2024 May;41(S 01):e76-e84.
- Shen L, Lobo VE, Cordova D, Larson DB, Kamaya A. An Institutional Approach for Developing a Point-of-Care Ultrasound Program Infrastructure (https://pubmed.ncbi.nlm.nih.gov/37984768/). J Am Coll Radiol. 2024 Aug;21(8):1269-1275.
- Shokoohi H, Boniface KS, Pourmand A, Liu YT, Davison DL, et al. Bedside Ultrasound Reduces Diagnostic Uncertainty and Guides Resuscitation in Patients With Undifferentiated Hypotension (https://pubmed.ncbi.nlm.nih.gov/26575653/). Crit Care Med. 2015 Dec;43(12):2562-9.
- Thind GS, Fox S, Gupta M, Chahar P, Jones R, Dugar S. Point-of-care ultrasonography for the hospitalist (https://pubmed.ncbi.nlm.nih.gov/34078618/). Cleve Clin J Med. 2021;88(6):345-359. Published 2021 Jun 2.
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





