Retroperitoneal Lymph Node Dissection (RPLND) is a complex surgical procedure used to remove retroperitoneal lymph nodes for staging and treating testicular cancer. It supports accurate diagnosis, reduces relapse risk, and guides further oncologic management.
Introduction
Retroperitoneal lymph node dissection (RPLND) is a specialised surgical procedure with significant diagnostic and therapeutic value, particularly in the context of urological oncology. First developed in the mid-twentieth century, RPLND has evolved alongside advances in surgical techniques, imaging modalities, and our understanding of malignancies such as testicular cancer. It remains a cornerstone in the staging and management of select genitourinary neoplasms, with its diagnostic role garnering renewed interest due to improvements in minimally invasive surgery and molecular pathology.
Definition and Purpose
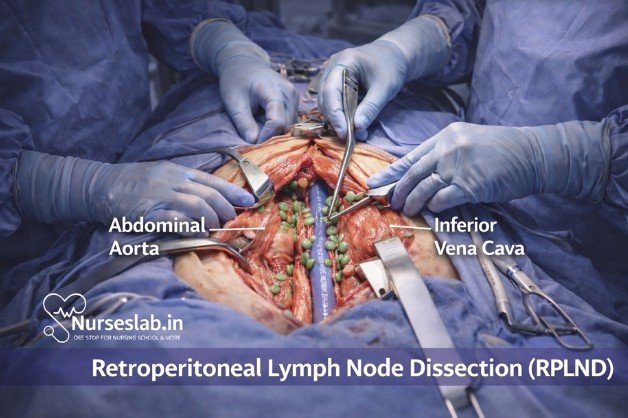
Retroperitoneal lymph node dissection refers to the surgical removal of lymphatic tissue from the retroperitoneal space, typically encompassing nodes along the aorta, vena cava, and iliac vessels. While RPLND can be performed for both diagnostic and therapeutic purposes, its diagnostic role is critical in accurate pathological staging, guiding subsequent management, and identifying occult metastatic disease.
Distinguishing between diagnostic and therapeutic RPLND is essential: Diagnostic RPLND is undertaken to obtain histological confirmation of lymph node involvement when non-invasive modalities are inconclusive, whereas therapeutic RPLND aims to achieve loco-regional control of disease.
Indications for RPLND
The primary indications for RPLND as a diagnostic procedure include:
- Testicular Cancer (Non-Seminomatous Germ Cell Tumours, NSGCT): Staging and detection of micrometastatic disease in clinical stage I or II patients, especially when imaging is ambiguous or serum tumour markers are discordant.
- Residual Mass Evaluation: Assessment of residual retroperitoneal masses following chemotherapy for germ cell tumours, to differentiate between viable tumour, teratoma, or necrosis.
- Other Malignancies: Selected cases of retroperitoneal sarcoma, lymphoma, or metastatic carcinoma where nodal pathology influences management.
- Uncertain Diagnosis: When less invasive diagnostic modalities (imaging, biopsy) are non-diagnostic, and tissue confirmation is required.
Patient selection for diagnostic RPLND is critical and based on multidisciplinary assessment, balancing the risks of surgery against the necessity for definitive staging. Absolute and relative contraindications must be considered, including comorbidities, previous retroperitoneal surgery, and performance status.
Preoperative Evaluation
Imaging
Comprehensive preoperative imaging is essential to delineate the extent of disease, anatomical variations, and surgical planning. Modalities include:
- Contrast-enhanced CT Scan: The standard imaging tool for evaluating retroperitoneal lymph nodes, vascular anatomy, and adjacent organ involvement.
- MRI: Useful in selected cases for superior soft tissue contrast or when CT is contraindicated.
- PET-CT: Occasionally employed to assess metabolic activity of masses or guide decision-making in ambiguous cases.
Laboratory Tests
Key laboratory investigations include:
- Serum Tumour Markers: Alpha-fetoprotein (AFP), beta-human chorionic gonadotropin (β-hCG), and lactate dehydrogenase (LDH) for germ cell tumours.
- Routine Preoperative Investigations: Complete blood count, renal and liver function tests, coagulation profile.
Patient Preparation
Preoperative preparation encompasses:
- Informed Consent: Detailed discussion regarding risks, benefits, and alternatives.
- Optimisation of Comorbidities: Cardiopulmonary assessment, control of hypertension or diabetes.
- Bowel Preparation: As per institutional protocol, especially for open procedures.
- Preoperative Marking and Planning: Identification of incision sites, review of imaging, and multidisciplinary input where necessary.
Surgical Techniques
Open RPLND
The traditional approach to RPLND is via a midline laparotomy, providing excellent exposure of the retroperitoneal space. The procedure is performed under general anaesthesia and involves the following steps:
- Midline incision from xiphoid to pubis.
- Mobilisation of the intestines and exposure of the retroperitoneum.
- Identification and preservation of major vessels (aorta, inferior vena cava).
- Systematic removal of lymphatic tissue in defined anatomical templates (right, left, or bilateral), according to tumour laterality.
- Special attention to nerve-sparing techniques to preserve antegrade ejaculation.
- Meticulous haemostasis and closure.
Minimally Invasive RPLND (Laparoscopic and Robotic)
Recent advancements have enabled RPLND to be performed using minimally invasive techniques, offering potential benefits in terms of reduced morbidity, shorter hospital stay, and faster recovery. Both laparoscopic and robotic-assisted approaches follow similar anatomical principles:
- Patient positioning and port placement (typically transperitoneal or retroperitoneal).
- Creation of working space and identification of anatomical landmarks.
- Dissection and removal of lymphatic tissue with enhanced visualisation.
- Nerve-sparing and vessel preservation facilitated by magnified views and precision instrumentation.
- Specimen retrieval using endoscopic bags.
- Closure and post-procedure assessment.
Minimally invasive RPLND requires advanced surgical expertise and may be limited by tumour bulk, prior surgery, or anatomical complexity.
Intraoperative Considerations
Anatomical Landmarks
Successful RPLND demands thorough knowledge of retroperitoneal anatomy, including:
- Aorta and inferior vena cava
- Renal vessels
- Ureters
- Sympathetic chain and genitofemoral nerve
- Psoas muscle
Clear identification of these structures is vital to avoid iatrogenic injury and ensure comprehensive dissection.
Nerve-Sparing Techniques
Preservation of the sympathetic and parasympathetic fibres responsible for ejaculation is a key consideration, especially in younger patients. Nerve-sparing RPLND utilises meticulous dissection and intraoperative nerve monitoring to reduce the risk of retrograde ejaculation and maintain sexual function.
Intraoperative Monitoring
Continuous monitoring of vital signs, urine output, and estimated blood loss is mandatory. In complex cases, intraoperative ultrasound or fluorescence imaging may aid in identifying vascular structures and lymph node boundaries.
Postoperative Management
Recovery Protocols
Postoperative care focuses on early mobilisation, pain control, and prevention of complications. Enhanced recovery protocols may include:
- Early ambulation
- Multimodal analgesia
- Thromboprophylaxis
- Gradual resumption of oral intake
Monitoring and Pain Management
Close monitoring for haemodynamic stability, urine output, and signs of infection is essential. Pain management typically involves a combination of opioids, non-steroidal anti-inflammatory drugs (NSAIDs), and local anaesthetic techniques such as epidural analgesia.
Early Complications
Potential early postoperative complications include:
- Bleeding and haematoma formation
- Infection (wound or intra-abdominal)
- Ileus and gastrointestinal dysfunction
- Chylous ascites due to lymphatic injury
- Urinary or vascular injury
Prompt recognition and management are critical to minimise morbidity and facilitate recovery.
Complications and Risks
RPLND is associated with both short-term and long-term risks, which must be discussed with patients preoperatively. Common complications include:
- Retrograde Ejaculation: Due to injury to sympathetic fibres; incidence is reduced with nerve-sparing techniques.
- Lymphocele or Chylous Ascites: Resulting from disruption of lymphatic channels; may require dietary modification, drainage, or surgical intervention.
- Vascular Injury: Injury to major vessels can result in significant blood loss and may necessitate repair.
- Infection: Wound infection or intra-abdominal abscess.
- Bowel Injury: Rare but serious complication requiring prompt recognition and surgical repair.
- Adhesion Formation: May lead to future bowel obstruction.
Long-term risks include:
- Infertility: Especially in bilateral or non-nerve-sparing procedures.
- Chronic Pain: Related to nerve injury or scar formation.
- Lymphedema: Lower limb swelling due to lymphatic disruption.
Management strategies for complications vary from conservative approaches (e.g., dietary modification for chylous ascites) to interventional procedures (e.g., drainage, surgical repair).
Diagnostic Value
RPLND provides unparalleled diagnostic accuracy in the assessment of retroperitoneal lymph node involvement, especially when imaging is inconclusive. Its sensitivity and specificity for detecting micrometastatic disease surpass most non-invasive modalities. Pathological staging obtained through RPLND directly impacts treatment planning, prognosis, and eligibility for adjuvant therapies.
In testicular cancer, RPLND can upstage or downstage disease, influencing the need for chemotherapy, radiotherapy, or surveillance. The ability to differentiate viable tumour from teratoma or necrosis in residual masses is of particular importance, as it guides further management and avoids overtreatment.
Limitations of RPLND as a diagnostic tool include its invasive nature, potential morbidity, and the requirement for specialised surgical expertise. Nonetheless, in carefully selected patients, its diagnostic value remains unmatched.
Nursing Care of Patients Undergoing Retroperitoneal Lymph Node Dissection (RPLND)
The operation involves removing lymph nodes from the retroperitoneal space – the area behind the peritoneum, the lining of the abdominal cavity. RPLND may also be indicated in certain cases of other malignancies, such as renal cell carcinoma or lymphoma, for diagnostic or therapeutic purposes.
Preoperative Nursing Care
Patient Assessment
A thorough preoperative assessment is crucial to identify any risk factors and ensure the patient is optimized for surgery:
- Medical History Review: Assess for comorbidities such as diabetes, hypertension, or bleeding disorders. Obtain a detailed oncological history including prior chemotherapy or radiotherapy.
- Physical Examination: Evaluate for signs of infection, nutritional status, and baseline vital signs. Assess for peripheral edema and signs of venous thromboembolism.
- Laboratory and Diagnostic Tests: Ensure completion of blood counts, coagulation profiles, renal and liver function tests, and relevant tumor markers. Review imaging studies (CT/MRI) for surgical planning.
- Psychosocial Assessment: Explore anxiety, understanding of the procedure, support systems, and potential concerns regarding fertility and body image.
Preoperative Preparation
- Informed Consent: Verify that informed consent for the procedure, anesthesia, and potential blood transfusion has been obtained and documented.
- Patient Education: Explain the surgical procedure, expected outcomes, and potential risks in understandable terms. Discuss postoperative expectations, pain management strategies, and the importance of early mobilization.
- Bowel Preparation: Some surgeons may require bowel prep to reduce the risk of intra-abdominal contamination.
- Skin Preparation: Instruct the patient on preoperative showering and assist with hair removal as per institutional protocol.
- Fasting and Medication Management: Ensure the patient is fasting as required. Review and manage regular medications, withholding or administering as indicated (e.g., anticoagulants, antihypertensives).
- IV Access and Blood Products: Establish reliable intravenous access. Ensure blood products are available if significant blood loss is anticipated.
Psychological Support
Provide emotional support to reduce preoperative anxiety. Facilitate communication with the surgical and anesthesia teams to address any patient or family queries. Offer information about fertility preservation options, such as sperm banking, if appropriate.
Intraoperative Nursing Considerations
- Positioning: Ensure correct patient positioning (usually supine) to prevent nerve injuries and pressure ulcers during the lengthy procedure.
- Monitoring: Collaborate with the anesthesia team to monitor vital signs, urine output, and blood loss.
- Infection Control: Maintain strict aseptic technique to minimize the risk of postoperative infection.
- Instrument and Sponge Counts: Perform accurate counts to prevent retained surgical items.
- Communication: Serve as a liaison between the surgical team and the patient’s family, providing updates as appropriate.
Postoperative Nursing Care
Immediate Postoperative Phase (PACU/ICU)
- Airway and Breathing: Assess airway patency, oxygen saturation, and respiratory effort. Administer supplemental oxygen as prescribed.
- Circulatory Status: Monitor heart rate, blood pressure, and peripheral perfusion. Be alert for signs of hypovolemia or hemorrhage (tachycardia, hypotension, decreased urine output).
- Pain Management: Administer prescribed analgesics, often via patient-controlled analgesia (PCA) or epidural. Assess pain frequently using validated scales.
- Fluid Balance: Maintain accurate records of input and output. Monitor for signs of fluid overload or deficit.
- Wound and Drain Care: Inspect the surgical site for bleeding, hematoma, or infection. Manage surgical drains as per protocol, noting type, volume, and character of output.
- Urinary Catheter Care: Monitor for hematuria, assess urine output, and maintain catheter patency. Be vigilant for signs of urinary tract infection.
Ongoing Postoperative Care (Ward)
Monitoring and Complication Prevention
- Vital Signs: Continue regular monitoring. Watch for early signs of sepsis, deep vein thrombosis (DVT), or pulmonary embolism.
- Gastrointestinal Function: Assess for return of bowel sounds and passage of flatus. Initiate gradual reintroduction of oral intake as tolerated. Monitor for ileus, nausea, or vomiting.
- Mobility: Encourage early, assisted mobilization to reduce the risk of DVT, pulmonary complications, and pressure injuries. Provide physiotherapy support as indicated.
- Respiratory Care: Instruct on deep breathing, coughing exercises, and use of incentive spirometry to prevent atelectasis and pneumonia.
- Infection Control: Observe for fever, redness, swelling, or discharge at surgical and intravenous sites. Adhere to hand hygiene and aseptic techniques.
- Venous Thromboembolism Prophylaxis: Administer prescribed anticoagulants and utilize mechanical prophylaxis (e.g., compression stockings) as directed.
- Psychological Support and Education: Provide ongoing reassurance. Address concerns about recovery, fertility, and sexual function. Involve family members in care and education as appropriate.
Specific Complications and Nursing Interventions
- Lymphocele Formation: Monitor for abdominal swelling or fluid collections. Notify the surgical team if suspected.
- Chylous Ascites: Be vigilant for milky drainage in surgical drains, which may indicate lymphatic leakage. Monitor nutritional status and consult dietitians for a low-fat diet if needed.
- Paralytic Ileus: Withhold oral intake until bowel function returns. Use nasogastric decompression as prescribed.
- Injury to Adjacent Structures: Monitor for hematuria, anuria, or signs of peritonitis, which may suggest injury to the urinary tract or bowel.
Pain Management
Effective postoperative pain control is essential for recovery and early mobilization. Utilize multimodal analgesia approaches, including opioids, non-steroidal anti-inflammatory drugs (NSAIDs), and regional techniques (e.g., epidural infusion). Assess pain regularly and adjust the regimen as needed. Educate the patient on pain management options and the importance of reporting breakthrough pain.
Nutrition and Hydration
Monitor for postoperative nausea and vomiting. Progress the patient’s diet from clear fluids to regular diet as tolerated, based on bowel function. Collaborate with dietitians to address increased nutritional needs during recovery, especially if lymphatic leakage is present. Maintain adequate hydration and electrolyte balance.
Discharge Planning and Patient Education
- Wound Care: Teach the patient and family how to care for the incision and drains at home. Provide instructions on signs of infection and when to seek medical attention.
- Activity Restrictions: Advise on activity limitations, lifting restrictions, and gradual return to normal activities.
- Follow-Up Appointments: Arrange for timely surgical, oncological, and primary care follow-up. Emphasize the importance of attending these appointments for ongoing surveillance and management.
- Fertility and Sexual Health: Discuss potential impacts on fertility and sexual function. Provide referrals to reproductive specialists or counseling services as needed.
- Psychosocial Support: Facilitate connections to support groups, counseling services, or psychological support for coping with cancer diagnosis and recovery.
Special Considerations
Cultural Sensitivity in Patient Care
Nurses should provide care that respects the patient’s cultural and religious beliefs, especially regarding modesty, gender of the caregiver, dietary restrictions, and family involvement in care decisions. In the context of Kuwait and the wider Middle East, involving family members and respecting cultural norms around privacy and consent is essential.
Multidisciplinary Collaboration
Optimal care for patients undergoing RPLND requires teamwork among surgeons, anesthesiologists, urologists, oncologists, physiotherapists, dietitians, and social workers. Nurses play a pivotal role in coordinating care and advocating for the patient’s needs throughout the surgical journey.
REFERENCES
- Beveridge T, Allman B, Johnson M. Retroperitoneal Lymph Node Dissection: Anatomical and Technical Considerations from a Cadaveric Study https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5412119/ . J Urol. Dec 2016; 196(6): 1764-1771.
- Canadian Cancer Society (CA). Retroperitoneal lymph node dissection (RPLND) https://cancer.ca/en/treatments/tests-and-procedures/retroperitoneal-lymph-node-dissection-rplnd.
- Zeng J, Cary C, Masterson TA. Retroperitoneal Lymph Node Dissection: Perioperative Management and Updates on Surgical Techniques. Urol Clin North Am. 2024 Aug;51(3):407-419. doi: 10.1016/j.ucl.2024.03.009. Epub 2024 May 18. PMID: 38925743.
- MacMillan Cancer Support (U.K.) Retroperitoneal lymph node dissection (RPLND) https://www.macmillan.org.uk/cancer-information-and-support/treatments-and-drugs/rplnd. Last updated 5/1/2022.
- Radiopaedia. Lymph node enlargement https://radiopaedia.org/articles/lymph-node-enlargement?lang=us. Last revised 6/29/2023.
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





