Urine specific gravity evaluates how concentrated or dilute urine is, helping assess hydration, kidney function, and conditions such as dehydration, SIADH, diabetes insipidus, and renal impairment. It is a key component of routine urinalysis and clinical evaluation.
Introduction
Urinalysis remains one of the most widely used diagnostic tools in clinical medicine, offering valuable insights into renal function, hydration status, and a variety of systemic conditions. Among the parameters assessed, the specific gravity of urine holds particular significance. It provides an indirect measure of urine concentration, reflecting the kidney’s ability to conserve or excrete water and solutes.
Definition and Principles
What Is Specific Gravity?
Specific gravity (SG) is a dimensionless measurement that compares the density of urine to the density of pure water at a specified temperature. In clinical practice, it is typically measured at room temperature (20°C). The SG of pure water is defined as 1.000. Urine, which contains dissolved substances such as electrolytes, urea, creatinine, and other metabolites, will have a higher density than water, resulting in a specific gravity greater than 1.000.
Physical and Chemical Principles
The principle behind specific gravity measurement is based on the mass of solutes dissolved in urine per unit volume. The more concentrated the urine, the higher its specific gravity. This concentration is determined by the kidney’s ability to reabsorb water and solutes, which is influenced by hormonal regulation (e.g., antidiuretic hormone) and renal tubular function. Unlike osmolality, which strictly measures the number of particles in solution, specific gravity is affected by both the size and number of molecules present, making it sensitive to the presence of large molecules such as glucose and proteins.
Methods of Measurement
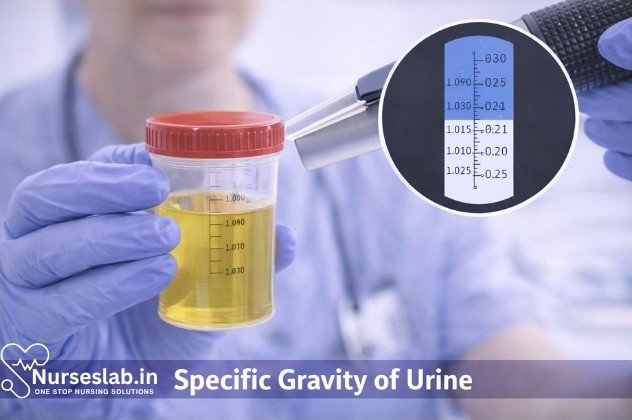
1.Refractometry
Refractometry is the most accurate and widely used method for determining urine specific gravity in modern laboratories. It operates on the principle that the refractive index of urine increases with the concentration of dissolved solutes. A refractometer requires only a small volume of urine and provides rapid results. It is less affected by temperature and allows for correction based on the presence of abnormal solutes such as glucose and protein.
2.Urinometer
The urinometer is a traditional device consisting of a weighted glass float that is placed in a cylinder containing urine. The level at which the float stabilizes corresponds to the specific gravity. While simple and inexpensive, the urinometer requires a larger urine volume and its accuracy can be compromised by temperature variations and the presence of high molecular weight substances.
3.Dipstick Method
Urine dipsticks offer a rapid, convenient, and semi-quantitative assessment of specific gravity. The dipstick pad contains chemicals that change color in response to ionic concentration. However, this method is less precise, as it primarily reflects ionic solutes and may not accurately account for non-ionic solutes such as glucose or urea. Dipstick readings can also be influenced by urine pH and the presence of interfering substances.
Comparison of Methods
| Method | Accuracy | Sample Volume | Interferences | Clinical Use |
| Refractometry | High | Low | Protein, glucose (correctable) | Laboratory, point-of-care |
| Urinometer | Moderate | High | Temperature, protein, glucose | Traditional, resource-limited settings |
| Dipstick | Low to moderate | Low | pH, ionic solutes | Screening, bedside testing |
Clinical Significance
The specific gravity of urine is a vital indicator of renal concentrating and diluting ability. It provides insights into hydration status, renal tubular function, and the presence of abnormal solutes. In healthy adults, normal urine specific gravity ranges from 1.005 to 1.030, with values fluctuating according to fluid intake, physical activity, and environmental factors. Persistent deviations from normal ranges can signal underlying pathology.
Why Specific Gravity Matters
Assessment of urine specific gravity is crucial in the evaluation of patients with suspected renal dysfunction, electrolyte imbalances, and disorders of water metabolism. It helps differentiate between prerenal, renal, and postrenal causes of abnormal urine concentration, guides fluid management, and assists in monitoring the effectiveness of therapeutic interventions.
Interpretation of Results
High Specific Gravity
Elevated urine specific gravity (>1.030) typically indicates concentrated urine, which may result from dehydration, reduced fluid intake, excessive sweating, vomiting, diarrhea, or glycosuria (as seen in uncontrolled diabetes mellitus). It may also be observed in conditions causing increased secretion of antidiuretic hormone (ADH), such as the syndrome of inappropriate antidiuretic hormone secretion (SIADH).
Low Specific Gravity
A low specific gravity (<1.005) suggests dilute urine and may be seen in patients with excessive fluid intake (polydipsia), diabetes insipidus (deficiency or resistance to ADH), or renal tubular dysfunction (e.g., acute tubular necrosis). In chronic kidney disease, the loss of concentrating ability can result in a fixed specific gravity around 1.010, indicating isosthenuria.
Clinical Scenarios
- Dehydration: High specific gravity due to water conservation by the kidneys.
- Diabetes Mellitus: High specific gravity from glycosuria; may be accompanied by other findings such as ketonuria.
- Diabetes Insipidus: Low specific gravity from inability to concentrate urine.
- SIADH: High specific gravity due to inappropriate water retention.
- Renal Failure: Fixed or low specific gravity due to impaired tubular function.
Factors Affecting Specific Gravity
Hydration Status
Fluid intake is the most significant determinant of urine specific gravity. In states of dehydration or restricted fluid intake, kidneys conserve water, resulting in concentrated urine and elevated SG. Conversely, excessive fluid intake or intravenous fluids dilute urine and lower SG.
Dietary Influences
Dietary composition affects urine concentration. High protein diets, increased salt intake, and consumption of diuretics can alter urine osmolality and SG. The ingestion of large amounts of glucose or other solutes can also artificially elevate SG.
Medications
Several medications impact urine concentration and SG. Diuretics promote water and solute excretion, lowering SG. Drugs affecting ADH secretion or action (e.g., vasopressin analogs, lithium) can cause significant changes. Contrast agents used in imaging studies may transiently increase SG due to high molecular weight compounds.
Disease States
Renal diseases, endocrine disorders, and systemic illnesses influence urine SG. Renal tubular disorders impair concentrating or diluting ability, resulting in abnormal SG readings. Endocrine conditions such as diabetes mellitus and SIADH profoundly affect water and solute handling by the kidneys.
Diagnostic Implications
Assessment of Renal Function
Specific gravity is a key parameter in the evaluation of renal concentrating ability. In acute and chronic renal failure, the loss of tubular function leads to a fixed SG, reflecting isosthenuria. SG measurement aids in distinguishing prerenal azotemia (high SG) from intrinsic renal disease (low or fixed SG).
Detection of Dehydration
Elevated SG is a sensitive marker of dehydration and volume depletion. It guides fluid resuscitation and management in acute care settings, especially in pediatric and elderly populations.
Diagnosis of Diabetes Insipidus and SIADH
Urine SG measurement is integral to the workup of polyuria and polydipsia. In diabetes insipidus, persistent low SG confirms impaired ADH activity, while high SG in SIADH reflects inappropriate water reabsorption.
Monitoring and Management
Serial SG assessments are useful for monitoring disease progression, therapeutic response, and adherence to fluid and dietary restrictions in a variety of clinical scenarios.
Limitations and Considerations
Potential Errors
Measurement errors can arise from improper sample handling, temperature fluctuations, and instrument calibration issues. Contamination, the presence of high concentrations of glucose or protein, and certain medications may skew results.
Confounding Factors
Non-renal factors such as fever, exercise, and gastrointestinal losses can influence SG independently of kidney function. Interpretation must be contextual, considering the patient’s clinical status, laboratory values, and history.
Best Practices
To enhance accuracy, urine samples should be collected midstream, analyzed promptly, and interpreted alongside other urinalysis parameters and clinical information. Refractometry is preferred for precise measurement, and dipstick results should be confirmed by laboratory methods when critical decisions are involved.
acy, urine samples should be collected midstream, analyzed promptly, and interpreted alongside other urinalysis parameters and clinical information. Refractometry is preferred for precise measurement, and dipstick results should be confirmed by laboratory methods when critical decisions are involved.
Nursing Care of Patients Undergoing Specific Gravity of Urine Testing
Nurses play a pivotal role in ensuring the accuracy of the test results, patient safety, comfort, and education throughout the procedure.
Nursing Responsibilities Before the Procedure
Patient Assessment and Preparation
- Review Physician’s Orders:
- Confirm the indication for the test and any special instructions regarding fluid intake, medications, or timing. Note if the test should be conducted as part of a 24-hour urine collection or random sample.
- Patient Identification and Consent:
- Ensure correct identification using at least two patient identifiers. Explain the procedure, its purpose, and obtain informed consent if required by policy.
- Education and Communication:
- Clearly inform the patient about the process of urine collection. Emphasize the importance of providing a clean-catch midstream sample to minimize contamination. Address any concerns or questions.
- Assess for Factors Affecting Results:
- Inquire about recent fluid intake, diuretic use, medications, or intravenous infusions that may alter urine concentration. Document findings and communicate with the healthcare team as needed.
- Prepare Equipment:
- Gather sterile or clean specimen containers, gloves, cleansing wipes, labels, and requisition forms. Ensure all materials are within reach and the collection area is clean and private.
- Hand Hygiene and Infection Control:
- Wash hands thoroughly before and after patient contact. Use gloves during specimen handling to prevent cross-contamination.
Special Considerations
- Pediatric Patients: May require assistance or parental involvement for specimen collection. Use age-appropriate explanations and comfort measures.
- Bedridden or Incontinent Patients: Utilize urine collection bags, catheters, or non-invasive methods as prescribed. Maintain dignity and privacy.
- Patients with Mobility Issues: Offer assistance to the bathroom or provide bedside commode if needed. Ensure safety to prevent falls.
Nursing Responsibilities During the Procedure
Specimen Collection
- Patient Instruction:
- Guide the patient to wash hands and cleanse the genital area thoroughly. For midstream collection, instruct the patient to void the first portion into the toilet, collect the midstream urine in the container, and finish voiding in the toilet.
- Assistance and Privacy:
- Provide privacy by closing doors or curtains. Offer assistance as needed, especially for elderly, pediatric, or disabled patients.
- Specimen Handling:
- Immediately cover and label the specimen container with patient details, date, and time of collection. Ensure prompt delivery to the laboratory to prevent changes in specific gravity due to evaporation or bacterial growth.
- Safety and Comfort:
- Monitor for signs of discomfort, urgency, or inability to void. In cases where catheterization is necessary, follow aseptic technique and institutional protocols.
Documentation
- Record the time of collection, appearance of urine (color, clarity, volume), and any relevant patient observations.
- Note any deviations from standard procedures, such as difficulties in collection or use of alternative methods.
Nursing Responsibilities After the Procedure
Post-Collection Care and Follow-Up
- Monitor Patient Well-being:
- Observe for any adverse reactions, such as discomfort during voiding or complications from catheterization. Address patient concerns promptly.
- Hand Hygiene and Disposal:
- Dispose of used materials safely according to infection control guidelines. Perform hand hygiene after specimen handling.
- Patient Education:
- Inform the patient about when results will be available and any further instructions, such as fluid intake or medication adjustments. Reinforce the importance of reporting changes in urinary patterns.
- Documentation:
- Complete all required documentation in the patient’s chart, including the procedure, any complications, and patient education provided.
- Result Interpretation and Communication:
- Upon receipt of the specific gravity results, collaborate with the healthcare team to interpret findings in the clinical context. Notify the physician of abnormal values and assist in implementing further diagnostic or therapeutic interventions.
Potential Complications and Nursing Interventions
- Inadequate Specimen: If the sample is insufficient or contaminated, notify the physician and repeat the collection, ensuring proper technique.
- Patient Anxiety or Discomfort: Provide reassurance, explain the importance of the procedure, and offer emotional support.
- Catheter-Related Issues: Monitor for signs of infection, trauma, or discomfort at the insertion site. Follow aseptic technique and institutional protocols.
Special Populations and Considerations
Pediatric Patients
Children may find urine collection challenging due to anxiety or lack of understanding. Use age-appropriate language, involve caregivers, and utilize non-invasive collection methods when possible. Distraction techniques or rewards may help alleviate stress.
Geriatric Patients
Older adults may have mobility issues, incontinence, or cognitive impairment. Provide assistance, maintain dignity, and adapt procedures to individual needs. Monitor closely for dehydration or renal dysfunction, which may be more prevalent in this population.
Patients with Chronic Illness
Patients with diabetes, renal disease, or heart failure may require frequent monitoring of urine specific gravity. Educate about the significance of the test in disease management and encourage adherence to prescribed fluid and medication regimens.
Patient Education and Advocacy
Nurses serve as advocates and educators for patients undergoing diagnostic procedures. Ensure that patients understand the purpose of the specific gravity test and its role in their overall care. Address misconceptions, provide written materials if available, and encourage questions. Empower patients to participate actively in their care.
Quality Assurance and Safety Measures
- Standardized Protocols: Adhere to institutional guidelines for specimen collection, handling, and documentation to ensure reliable results.
- Infection Control: Strictly follow hygiene and aseptic techniques to prevent healthcare-associated infections.
- Continuing Education: Stay updated with current best practices in urine testing procedures and patient care through ongoing professional development.
REFERENCES
- Common Laboratory Tests. In: Suneja M, Szot JF, LeBlond RF, et al., eds. DeGowin’s Diagnostic Examination. 11th ed. McGraw Hill; 2020.
- National Library of Medicine (U.S.). Urine Specific Gravity Test https://medlineplus.gov/ency/article/003587.htm. Last reviewed 8/20/2023.
- Odisho AY, Porten SP, Greene KL. Urologic Laboratory Examination. In: McAninch JW, Lue TF, eds. Smith & Tanagho’s General Urology. 19th ed. McGraw Hill; 2020
- Winter WE. The Kidney. In: Laposata M, eds. Laposata’s Laboratory Medicine: Diagnosis of Disease in the Clinical Laboratory. 3rd ed. McGraw-Hill Education; 2019.
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





