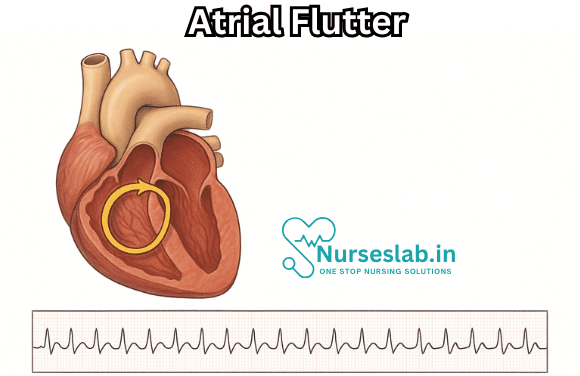
Atrial flutter is a common type of supraventricular tachycardia, a rapid heart rhythm originating above the heart’s ventricles. It is characterized by a distinctive “sawtooth” pattern on electrocardiograms (ECG), resulting from abnormal electrical activity in the atria the upper chambers of the heart. While atrial flutter is less prevalent than its cousin, atrial fibrillation, it remains a significant clinical concern due to its impact on cardiac function and its potential to cause serious complications.
What is Atrial Flutter?
At its core, atrial flutter is an arrhythmia, which means there is a disturbance in the normal rhythm of the heart. In a healthy heart, electrical impulses originate in the sinoatrial (SA) node, the heart’s natural pacemaker. These impulses travel through the atria, causing them to contract and pump blood into the ventricles. In atrial flutter, a re-entrant circuit forms within the right atrium, causing the atria to beat very rapidly often between 240 and 350 times per minute much faster than the ventricles, which are protected by the slower conduction through the atrioventricular (AV) node.
Pathophysiology
The classic mechanism of atrial flutter involves a continuous, self-perpetuating circuit of electrical activity within the right atrium. This is typically referred to as “typical atrial flutter” or “cavotricuspid isthmus-dependent flutter,” since the circuit travels around the tricuspid valve and through a narrow region of tissue known as the cavotricuspid isthmus. Less commonly, atrial flutter can be “atypical,” arising from other parts of the atria or in people who have undergone prior surgery or ablation.
The rapid atrial rates in atrial flutter mean that the atria are contracting so quickly that they are unable to effectively move blood into the ventricles. Since the AV node cannot conduct every impulse, the heart’s ventricles typically beat at a slower, but still rapid, rate (often 120-150 beats per minute).
Causes and Risk Factors
Atrial flutter can occur in otherwise healthy individuals, but it is most often associated with structural heart disease or other predisposing conditions. Common causes and risk factors include:
- Hypertension: High blood pressure can cause structural changes to the heart’s atria.
- Coronary artery disease: Blockages in the arteries can lead to atrial scarring and abnormal rhythms.
- Heart failure: Weakened heart muscle increases risk.
- Congenital heart disease: Especially repaired or unrepaired atrial septal defects.
- Valvular heart disease: Disease of heart valves, particularly the mitral or tricuspid valves.
- Post-cardiac surgery: Scarring after heart surgery can foster abnormal circuits.
- Chronic lung disease: Conditions like COPD can strain the right side of the heart.
- Thyroid disorders: Both overactive (hyperthyroidism) and underactive thyroid can contribute.
- Alcohol use: Heavy drinking is a known precipitant (“holiday heart syndrome”).
- Excessive stimulant use: Caffeine, certain medications, or illicit drugs.
Symptoms of Atrial Flutter
Some individuals with atrial flutter may be entirely asymptomatic, while others experience a range of symptoms. The severity of symptoms often correlates with the ventricular rate and underlying cardiac function. Common symptoms include:
- Palpitations (a sensation of rapid or irregular heartbeat)
- Fatigue or weakness
- Shortness of breath (dyspnea)
- Dizziness or lightheadedness
- Chest discomfort or pain
- Exercise intolerance
- In severe cases, fainting (syncope)
Diagnosis
The diagnosis of atrial flutter is typically established with an electrocardiogram (ECG or EKG). On the ECG, atrial flutter is recognized by its distinctive “sawtooth” flutter waves, usually best seen in the inferior limb leads (II, III, and aVF). These waves represent rapid, regular atrial depolarizations.
Other diagnostic steps may include:
- Holter monitoring: 24-hour or longer ambulatory ECG to detect intermittent episodes.
- Event monitoring: For less frequent symptoms, longer-term monitoring may be necessary.
- Echocardiography: To assess heart structure and function.
- Blood tests: To evaluate for underlying metabolic or thyroid abnormalities.
- Exercise stress testing: If exercise-induced symptoms or ischemia is suspected.
Complications
Atrial flutter, if left untreated, can lead to serious complications:
- Stroke: The rapid, ineffective atrial contractions promote formation of blood clots, which can travel to the brain.
- Heart failure: Rapid ventricular rates or loss of atrial contraction can worsen existing heart failure.
- Tachycardia-induced cardiomyopathy: Prolonged rapid heart rates can weaken the heart muscle.
Because of the elevated risk of stroke, most patients with atrial flutter will be evaluated for anticoagulation (blood thinners), similar to protocols for atrial fibrillation.
Management and Treatment
The goals of atrial flutter management are to restore normal rhythm (sinus rhythm), control the ventricular rate, prevent thromboembolic complications, and address underlying causes. Treatment strategies may include:
Acute Management
- Rate control: Medications such as beta-blockers, calcium channel blockers, or digoxin can slow the ventricular response.
- Rhythm control: If the episode is recent or the patient is unstable, electrical cardioversion (a controlled electrical shock) can restore normal rhythm.
- Anticoagulation: If the flutter has been present for more than 48 hours or the duration is unknown, anticoagulation is recommended before attempting cardioversion, unless it’s an emergency.
Long-Term Management
- Catheter ablation: Radiofrequency ablation of the cavotricuspid isthmus is highly effective (over 90% success) for typical atrial flutter and is considered a first-line, potentially curative treatment.
- Medication: Ongoing use of antiarrhythmic drugs may be necessary in some patients, especially those not suitable for ablation.
- Anticoagulation: Continued use may be needed based on individual stroke risk assessment (using tools like CHA₂DS₂-VASc score).
- Lifestyle modifications: Addressing contributing factors such as hypertension, sleep apnea, weight management, and moderating alcohol use.
Prognosis
With appropriate management, many individuals with atrial flutter can lead normal, active lives. Catheter ablation has dramatically improved outcomes by offering a high likelihood of durable cure for typical atrial flutter. However, atrial flutter can sometimes recur, and there is always a risk of developing atrial fibrillation, which may require ongoing attention.
The risk of stroke and heart failure underscores the importance of timely diagnosis and comprehensive management. Adherence to medical therapy, regular follow-up, and addressing modifiable risk factors are essential to optimize outcomes.
Prevention
While not all cases of atrial flutter are preventable, certain measures can reduce the risk:
- Regular physical activity and a heart-healthy diet.
- Managing blood pressure and other cardiovascular risk factors
- Limiting alcohol and stimulant use
- Treating sleep apnea and other contributory
Nursing Care of Patients with Atrial Flutter
1. Assessment and Monitoring
- Vital Signs Monitoring: Regularly monitor heart rate, rhythm, blood pressure, respiratory rate, oxygen saturation, and temperature. Assess for irregular pulse and changes in blood pressure.
- Electrocardiogram (ECG) Monitoring: Continuous or frequent ECG monitoring is essential to detect arrhythmia episodes, rate, and rhythm changes. Document and report any variations promptly.
- Symptom Assessment: Observe for symptoms such as palpitations, chest discomfort, dizziness, shortness of breath, fatigue, and syncope. Document onset, duration, and severity.
- Haemodynamic Status: Assess for signs of decreased cardiac output (e.g., hypotension, cool extremities, oliguria, altered mental status).
2. Medication Administration and Management
- Antiarrhythmic Drugs: Administer prescribed medications such as amiodarone, sotalol, or beta-blockers as per protocol. Monitor for efficacy and adverse effects.
- Anticoagulation Therapy: Patients may be prescribed anticoagulants (e.g., warfarin, heparin, direct oral anticoagulants) to reduce the risk of thromboembolism. Monitor for bleeding, check INR values if on warfarin, and educate patients on bleeding precautions.
- Electrolyte Balance: Monitor and correct electrolyte imbalances, especially potassium and magnesium, as they can precipitate arrhythmias.
3. Oxygenation and Respiratory Support
- Administer supplemental oxygen if the patient is hypoxic.
- Position the patient in a semi-Fowler’s or comfortable position to facilitate breathing.
- Monitor for signs of respiratory distress and report promptly.
4. Patient Safety and Prevention of Complications
- Fall Precautions: Implement fall prevention strategies for patients with dizziness or syncope.
- Thromboembolism Prevention: Encourage early mobilisation if possible and use compression stockings as prescribed.
- Monitor for Heart Failure: Assess for signs such as peripheral oedema, jugular venous distension, and worsening dyspnoea.
5. Patient Education and Psychosocial Support
- Condition Explanation: Educate the patient and family about atrial flutter, its causes, symptoms, and the importance of medication adherence.
- Lifestyle Modification: Advise on dietary changes (e.g., low-salt diet), limiting caffeine and alcohol, and the importance of regular exercise as tolerated.
- Symptom Recognition: Teach patients to recognise warning signs such as chest pain, severe breathlessness, or neurological symptoms, and to seek immediate medical attention.
- Emotional Support: Provide reassurance, address anxiety, and offer counselling or support group information if needed.
6. Collaborative Care
- Coordinate with physicians, cardiologists, physiotherapists, and dietitians for comprehensive care.
- Prepare patients for procedures such as electrical cardioversion, electrophysiological studies, or catheter ablation if indicated.
- Ensure effective communication and documentation of care provided and patient response.
REFERENCES
- American Heart Association. Ablation for Arrhythmias. https://www.heart.org/en/health-topics/arrhythmia/prevention–treatment-of-arrhythmia/ablation-for-arrhythmias. Last reviewed 11/17/2022.
- American Heart Association. Other Heart Rhythm Disorders. https://www.heart.org/en/health-topics/arrhythmia/about-arrhythmia/other-heart-rhythm-disorders Last reviewed 9/25/2024.
- Ferri FF. Atrial flutter. In: Ferri’s Clinical Advisor 2025. Elsevier; 2025. https://www.clinicalkey.com.
- Curtis AB, Baykaner T, Narayan M. Atrial Fibrillation and Atrial Flutter. In: Fuster V, Narula J, Vaishnava P, et al, eds. Fuster and Hurst’s The Heart. 15th ed. McGraw-Hill Education; 2022.
- Heart Rhythm Society. Atrial Flutter (AFL). https://upbeat.org/heart-rhythm-disorders/atrial-flutter Last updated 11/19/2021.
- Merck Manual (Consumer Version). Atrial Fibrillation and Atrial Flutter. https://www.merckmanuals.com/home/heart-and-blood-vessel-disorders/abnormal-heart-rhythms/atrial-fibrillation-and-atrial-flutter. Last revised 9/2024.
- Rodriguez Ziccardi M, Goyal A, Maani CV. Atrial Flutter. https://pubmed.ncbi.nlm.nih.gov/31082029/. 2022 Dec 8. In: StatPearls [Internet]. Treasure Island, FL: StatPearls Publishing; 2024 Jan.
- Lloyd-Jones DM, et al. Life’s essential 8: Updating and enhancing the American Heart Association’s construct of cardiovascular health: A presidential advisory from the American Heart Association. Circulation. 2022; doi:10.1161/CIR.0000000000001078.
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





