Benign Prostatic Hyperplasia (BPH) is a non-cancerous enlargement of the prostate gland that commonly affects aging males, leading to lower urinary tract symptoms such as hesitancy, weak stream, nocturia, and incomplete bladder emptying—managed through lifestyle changes, medications, or surgical interventions depending on severity
What is Benign Prostatic Hyperplasia?
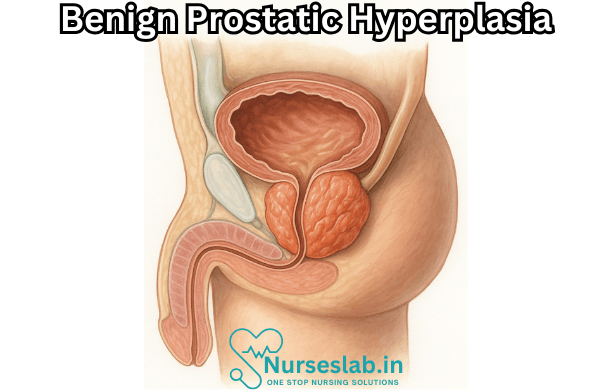
Benign Prostatic Hyperplasia refers to the non-cancerous growth of the prostate gland, a small organ situated below the bladder and in front of the rectum. The prostate surrounds the urethra—the tube through which urine passes from the bladder out of the body. As the prostate enlarges, it can press against and constrict the urethra, leading to various urinary symptoms.
BPH is a common condition, with prevalence increasing with age. By age 60, about half of individuals with a prostate have some signs of BPH, and by age 85, up to 90% may be affected to some degree.
Causes and Risk Factors
BPH is believed to be a consequence of hormonal changes that occur with aging, particularly the balance between testosterone and dihydrotestosterone (DHT), a more potent form of testosterone. As individuals age, DHT accumulates in the prostate, stimulating growth of prostate cells. Other proposed mechanisms involve changes in estrogen levels, chronic inflammation, and genetic predisposition.
- Age: The most significant risk factor. BPH is rare before age 40, but the risk increases steadily thereafter.
- Family History: Having a close relative with BPH increases the likelihood of developing the condition.
- Lifestyle Factors: Obesity, lack of physical activity, and metabolic syndrome may contribute.
- Chronic Diseases: Diabetes and heart disease are associated with a higher risk.
Signs and Symptoms
The symptoms of BPH are primarily related to lower urinary tract obstruction and are collectively known as lower urinary tract symptoms (LUTS). These can be divided into two main categories: voiding (obstructive) symptoms and storage (irritative) symptoms.
Voiding Symptoms
- Hesitancy: Difficulty starting urination
- Weak or interrupted stream
- Straining to empty the bladder
- Sensation of incomplete bladder emptying
Storage Symptoms
- Urgency: Sudden, compelling urge to urinate
- Frequency: Needing to urinate more often than usual
- Nocturia: Waking up at night to urinate
- Incontinence: Leakage of urine (less common in BPH alone but may occur)
Symptoms may be mild or severe and can significantly affect quality of life, sleep, and wellbeing. While BPH is not life-threatening, severe urinary obstruction can lead to complications such as urinary retention, recurrent urinary tract infections, bladder stones, and kidney damage.
Diagnosis
Diagnosing BPH involves a combination of medical history, physical examination, and specific investigations to rule out other causes of urinary symptoms (such as urinary tract infections, bladder cancer, or neurologic disorders).
History and Physical Exam
The healthcare provider will ask about the nature and duration of symptoms, their impact on life, and any history of urinary tract infections, surgeries, or neurological diseases. A digital rectal exam (DRE) is performed to assess the size and consistency of the prostate.
Investigations
- Urinalysis: To check for infection or blood in the urine.
- Prostate-Specific Antigen (PSA) Test: This blood test helps rule out prostate cancer, though PSA can be elevated in BPH.
- Uroflowmetry: Measures the strength and amount of urine flow.
- Postvoid Residual Volume: Ultrasound is used to assess how much urine remains in the bladder after urination.
- Imaging: Transrectal ultrasound may be used for further evaluation.
- Cystoscopy: Direct visualization of the urethra and bladder in select cases.
Severity Assessment
Clinicians often use symptom questionnaires, such as the International Prostate Symptom Score (IPSS), to assess severity and guide treatment decisions. The IPSS rates symptoms on a scale from mild to severe and helps monitor changes over time.
Management and Treatment Options
Treatment for BPH is tailored to symptom severity, prostate size, overall health, and patient preferences. Many individuals with mild symptoms require only monitoring, while those with bothersome symptoms may benefit from medical or surgical interventions.
Watchful Waiting
Individuals with mild symptoms and minimal impact on quality of life may opt for watchful waiting, which involves regular monitoring and lifestyle modifications. This approach is appropriate when symptoms are stable and complications are absent.
Lifestyle Modifications
Certain behavioral changes can help relieve symptoms:
- Limiting fluid intake in the evening
- Reducing caffeine and alcohol consumption
- Double voiding (urinating, waiting a few moments, then trying again)
- Regular physical activity
- Maintaining a healthy weight
Medications
Several classes of medications are used to manage BPH:
- Alpha Blockers: (e.g., tamsulosin, alfuzosin) Relax the muscles in the prostate and bladder neck, improving urine flow and reducing symptoms.
- 5-Alpha Reductase Inhibitors: (e.g., finasteride, dutasteride) Reduce the size of the prostate by blocking hormone changes, most effective in larger prostates.
- Combination Therapy: Using both alpha blockers and 5-alpha-reductase inhibitors may provide greater symptom relief in some cases.
- Phosphodiesterase-5 Inhibitors: (e.g., tadalafil) Sometimes used, especially if erectile dysfunction coexists.
- Anticholinergics and Beta-3 Agonists: May be considered for those with storage symptoms, though caution is needed.
Minimally Invasive Procedures
When medications are ineffective or not tolerated, minimally invasive procedures can relieve obstruction with fewer complications than surgery. Examples include:
- Transurethral Microwave Thermotherapy (TUMT): Uses heat to destroy excess prostate tissue.
- Transurethral Needle Ablation (TUNA): Uses radiofrequency energy to shrink tissue.
- Prostatic Urethral Lift (PUL): Mechanically lifts and holds enlarged prostate tissue away from the urethra.
- Water Vapor Therapy: Steam is used to ablate prostate tissue.
Surgical Interventions
Surgery is considered for individuals with severe symptoms, complications, or failure of less invasive therapies. Common surgical options include:
- Transurethral Resection of the Prostate (TURP): The most common procedure, where excess prostate tissue is removed via the urethra.
- Open or Robotic Prostatectomy: Reserved for very large prostates.
- Laser Surgery: Uses focused light energy to remove or vaporize tissue.
Prognosis and Outlook
BPH is a chronic condition, but with proper management, most individuals achieve good control of symptoms and maintain their quality of life. Untreated, severe obstruction can lead to complications, but these are infrequent with modern care.
Complications
- Acute Urinary Retention: Sudden inability to urinate, often requiring emergency intervention.
- Urinary Tract Infections: Increased risk due to incomplete bladder emptying.
- Bladder Stones: May form as a result of stagnant urine.
- Bladder or Kidney Damage: Rare, but can occur in severe cases.
Prevention and Healthy Living
While BPH cannot always be prevented, maintaining a healthy lifestyle may reduce risk or delay progression. This includes regular exercise, a balanced diet, weight management, and routine medical checkups.
Nursing Care of Patients with Benign Prostatic Hyperplasia (BPH)
Nursing Interventions
Promoting Urinary Elimination
- Encourage the patient to void at regular intervals to prevent retention.
- Monitor intake and output, noting any decrease in urine output or signs of retention.
- Assist with techniques such as double voiding (void, wait a few minutes, then void again).
- Advise the patient to avoid excessive fluid intake in the evening to reduce nocturia.
Preventing Infection
- Maintain strict aseptic technique during catheterisation or any invasive procedures.
- Encourage adequate fluid intake during the day (unless contraindicated) to flush the urinary tract.
- Monitor for signs of urinary tract infection—fever, dysuria, cloudy urine, and foul odour.
Patient Education
- Explain the nature of BPH, its benign nature, and the rationale for various treatments.
- Discuss lifestyle modifications such as avoiding caffeine and alcohol, which may worsen symptoms.
- Teach the importance of adhering to prescribed medications (e.g., alpha-blockers, 5-alpha-reductase inhibitors).
- Instruct on recognising signs of complications like acute urinary retention or infection, and when to seek medical attention.
Pre- and Post-operative Care (if Surgery is Indicated)
- Prepare the patient physically and psychologically for procedures like Transurethral Resection of the Prostate (TURP).
- Monitor for post-operative complications such as bleeding, infection, or catheter blockage.
- Provide catheter care, observe urine colour and volume, and ensure the patency of the catheter.
- Encourage early mobilisation to prevent deep vein thrombosis (DVT).
Supporting Emotional Well-being
- Offer reassurance regarding the benign nature of the condition.
- Provide a platform for the patient to express concerns about sexual function and body image.
- Refer to counsellors or support groups if needed.
Evaluation
- Patient reports improved urinary pattern and reduced symptoms.
- No signs of urinary tract infection or retention are observed.
- Patient verbalises understanding of the disease process and self-care measures.
- Patient demonstrates compliance with the treatment plan and lifestyle modifications.
REFERENCES
- American Urological Association. What is Benign Prostatic Hyperplasia (BPH)?. https://www.urologyhealth.org/urology-a-z/b/benign-prostatic-hyperplasia-(bph%29 Updated 9/2023.
- Wein AJ, et al., eds. Benign prostatic hyperplasia: Etiology, pathophysiology, epidemiology, and natural history. In: Campbell-Walsh-Wein Urology. 12th ed. Elsevier; 2021. https://www.clinicalkey.com.
- Bortnick E, Brown C, Simma-Chiang V, et al. Modern best practice in the management of benign prostatic hyperplasia in the elderly https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7273551/. Ther Adv Urol. 2020 May;12:1756287220929486.
- Garcia C, Chin P, Rashid P. Prostatic urethral lift: A minimally invasive treatment for benign prostatic hyperplasia. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4494639/. Prostate Int. 2015 Mar;3(1):1-5.
- Whitley B, et al. Benign prostatic hyperplasia. In: Conn’s Current Therapy 2021. Elsevier; 2021. https://www.clinicalkey.com.
- McVary KT, Roehrborn CG. Three-Year Outcomes of the Prospective, Randomized Controlled Rezūm System Study: Convective Radiofrequency Thermal Therapy for Treatment of Lower Urinary Tract Symptoms Due to Benign Prostatic Hyperplasia. https://pubmed.ncbi.nlm.nih.gov/29122620/. Urology. 2018 Jan;111:1
- Merck Manual Consumer Version. Benign Prostate Hyperplasia (BPH). https://www.merckmanuals.com/home/quick-facts-men-s-health-issues/benign-prostate-disorders/benign-prostate-hyperplasia-bph. Reviewed/revised 5/2023.
- Wein AJ, et al., eds. Evaluation and nonsurgical management of benign prostatic hyperplasia. In: Campbell-Walsh Urology. 12th ed. Elsevier; 2021.
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





