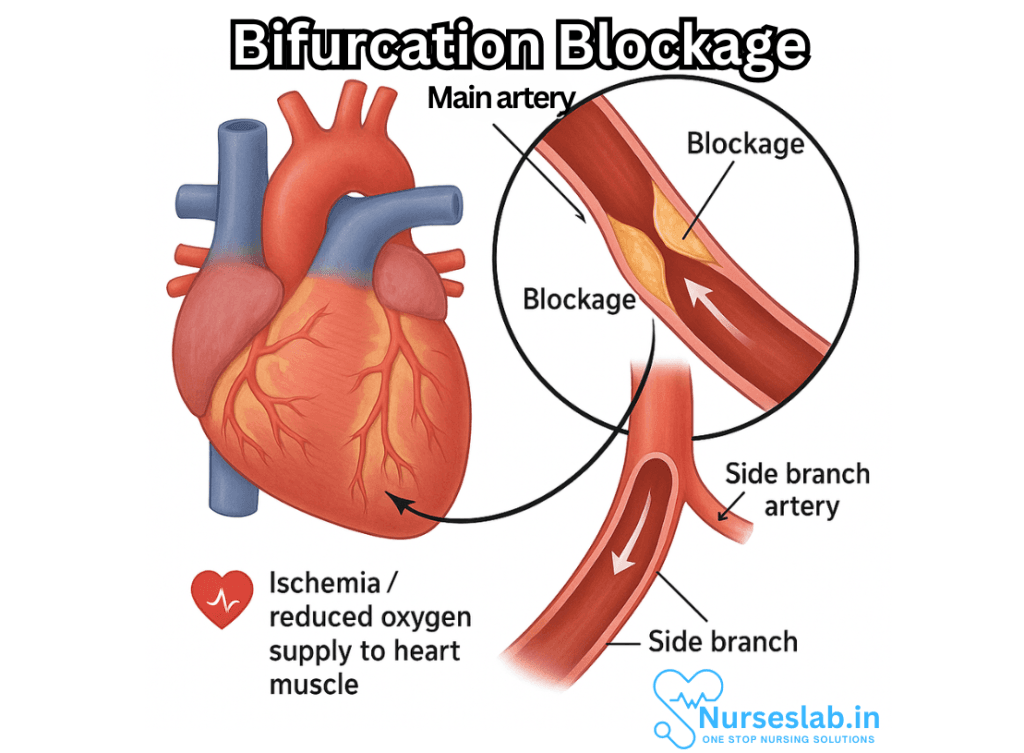
Bifurcation blockage is a specific type of coronary artery disease (CAD) that occurs at the point where a main coronary artery branches into a smaller side-branch vessel. This junction called a bifurcation—is particularly prone to plaque buildup due to turbulent blood flow, making it a complex site for both diagnosis and treatment.
Coronary artery disease (CAD) remains one of the leading causes of morbidity and mortality worldwide, manifesting itself in a multitude of clinical presentations, from silent ischemia to life-threatening acute coronary syndromes. Among the several patterns of arterial occlusion, bifurcation blockage holds particular clinical significance due to its complex anatomical and physiological considerations. This document aims to unravel the intricacies of CAD bifurcation blockage, encompassing its etiology, pathophysiology, diagnostic modalities, therapeutic approaches, and recent advances.
Introduction to Coronary Artery Bifurcation Anatomy
The coronary vasculature is a marvel of biological engineering, branching out to nourish the myocardium with life-sustaining oxygen and nutrients. Bifurcation refers to a point where a main coronary vessel divides into two branches; common sites include the left main coronary artery branching into the left anterior descending (LAD) and left circumflex (LCx) arteries, or the LAD bifurcating into diagonal and septal branches. The anatomical arrangement at these junctions renders them susceptible to atherosclerotic plaque formation and subsequent blockage.
Pathophysiology of Bifurcation Blockage
Atherosclerosis, the dominant culprit in CAD, is characterized by the accumulation of lipids, inflammatory cells, and fibrous elements within the arterial wall. The turbulent flow and altered shear stress at bifurcation sites accelerate the deposition of these elements. The branching pattern itself creates zones of low endothelial shear, fostering a pro-atherogenic environment.
When a plaque evolves at a bifurcation, it can compromise both the main vessel and one or both branches, creating a scenario that is more complex than single-vessel disease. The blockage may be concentric or eccentric, and may also involve plaque extension into the side branch ostium, jeopardizing distal blood flow.
Types of Bifurcation Lesions
Bifurcation lesions are classified based on the Medina classification, which considers involvement of the proximal main branch, distal main branch, and side branch:
- Medina 1,1,1: All three segments are affected.
- Medina 1,0,1: Proximal main and side branch affected, distal main spared.
- Medina 0,1,0: Only distal main branch affected, etc.
Understanding the lesion’s anatomy is crucial for planning intervention, as it predicts procedural complexity and the risk of side branch occlusion.
Clinical Manifestations
Bifurcation blockages can present with stable or unstable angina, depending on the degree and acuteness of obstruction. In some cases, patients may experience silent ischemia, especially in the setting of diabetes. Symptoms may include:
- Chest pain or discomfort, often radiating to the neck, jaw, or arm
- Shortness of breath
- Fatigue
- Palpitations
- In severe cases, syncope or sudden cardiac arrest
The clinical profile often depends on which coronary territory is involved and the extent of collateral circulation.
Diagnosis of Bifurcation Blockage
The diagnostic approach integrates clinical assessment, non-invasive imaging, and invasive coronary angiography.
Non-Invasive Modalities
- Electrocardiogram (ECG): May show signs of ischemia or infarction.
- Stress Testing: Assesses functional significance of coronary narrowing.
- Echocardiography: Detects wall motion abnormalities.
- CT Coronary Angiography: Offers a non-invasive visualization of coronary anatomy and bifurcations.
Invasive Modalities
Coronary angiography remains the gold standard, providing detailed visualization of bifurcation anatomy, the extent of blockage, and the relationship between main and side branches. Intravascular ultrasound (IVUS) or optical coherence tomography (OCT) can further characterize plaque morphology, vessel size, and stent positioning during intervention.
Management Strategies
The management of CAD bifurcation blockage is guided by patient symptoms, lesion complexity, and the overall risk profile. Treatment options include:
Medical Management
For patients with mild symptoms or limited disease:
- Antiplatelet therapy (aspirin, P2Y12 inhibitors)
- Statins to lower cholesterol
- Beta blockers and ACE inhibitors for risk reduction
- Lifestyle modifications: diet, exercise, smoking cessation
Medical therapy alone is often insufficient for significant bifurcation blockages, especially when the side branch supplies a large myocardial territory.
Interventional Approaches
Percutaneous coronary intervention (PCI) is the mainstay for significant bifurcation lesions, with techniques evolving over decades.
Stenting Techniques
- Provisional Stenting: The default strategy involves stenting the main branch and treating the side branch only if flow is compromised. It minimizes procedural complexity and restenosis risk.
- Two-Stent Strategies: Employed in complex lesions. Techniques include:
- Crush Technique: Stent is deployed in the side branch, then ‘crushed’ by a main branch stent.
- Culotte Technique: Stents are placed sequentially in both branches, overlapping at the bifurcation.
- T-stenting: Side branch stent placed perpendicularly to the main branch stent.
- Double Kissing (DK) Crush: Advanced technique with sequential balloon inflations for optimal expansion.
Choice depends on anatomy, operator experience, and side branch importance.
Adjunctive Techniques
- Kissing Balloon Inflation: Simultaneous inflation of balloons in both branches to optimize stent expansion.
- Final Pot (Proximal Optimization Technique): Post-dilation of the stent in the proximal main branch for better apposition.
Surgical Revascularization
In cases where PCI is not feasible, coronary artery bypass grafting (CABG) may be indicated, especially for left main bifurcation disease or multivessel involvement.
Complications and Prognosis
Bifurcation interventions carry higher risks than non-bifurcation procedures. Potential complications include:
- Side branch occlusion leading to myocardial infarction
- Stent malapposition or restenosis
- Coronary dissection or perforation
- Thrombosis at the stent site
Prognosis varies with lesion complexity, the success of revascularization, and comorbid conditions. Advances in drug-eluting stents and imaging have improved outcomes, but long-term follow-up is essential.
Nursing Care of Patients with Coronary Artery Disease: Bifurcation Blockage
Effective nursing care is essential for optimizing patient outcomes, minimizing complications, and supporting recovery throughout diagnosis, intervention, and rehabilitation.
Nursing Assessment
Comprehensive assessment is crucial to identify clinical manifestations, monitor disease progression, and establish a baseline for care.
Subjective Data
- History of chest pain or discomfort (angina), especially on exertion
- Dyspnea, fatigue, palpitations
- Risk factors: family history, smoking, diabetes, hypertension, hyperlipidemia
- Emotional status, anxiety, coping mechanisms
Objective Data
- Vital signs: blood pressure, heart rate, respiratory rate, oxygen saturation
- Physical exam: heart sounds, presence of murmurs or gallops, signs of heart failure (edema, jugular venous distension)
- ECG findings: ST-segment changes, arrhythmias
- Laboratory results: cardiac enzymes (troponin, CK-MB), lipid profile, blood glucose
- Imaging: echocardiogram, coronary angiography highlighting bifurcation lesions
Nursing Diagnoses
- Decreased cardiac output related to impaired myocardial perfusion
- Acute pain related to myocardial ischemia
- Ineffective tissue perfusion (cardiac) related to coronary artery blockage
- Risk for anxiety related to uncertainty of outcome and procedures
- Knowledge deficit regarding condition, treatment, and self-care
- Risk for ineffective coping related to chronic disease management
Nursing Interventions
Effective interventions focus on both acute management and long-term care of patients with CAD and bifurcation blockage.
Acute Phase Interventions
- Monitor Cardiac Status:
- Continuous ECG monitoring for arrhythmias or ischemic changes
- Frequent assessment of vital signs and oxygen saturation
- Monitor for signs of heart failure (e.g., crackles, peripheral edema, weight gain)
Manage Pain and Ischemia:
- Administer prescribed nitrates, beta-blockers, calcium channel blockers, and antiplatelet agents
- Provide supplemental oxygen as indicated
- Encourage rest and minimize exertion during acute episodes
- Prepare for and Support Interventions:
- Educate and prepare patients for diagnostic angiography and possible PCI or coronary artery bypass grafting (CABG)
- Monitor for complications post-procedure: bleeding, hematoma, arrhythmias, chest pain
- Maintain vascular access site integrity: monitor for bleeding or hematoma formation
- Administer IV fluids, anticoagulants, and antiarrhythmic medications per protocol
Long-Term Care and Rehabilitation
Secondary Prevention:
- Implement lifestyle modification education: dietary changes, smoking cessation, weight management, physical activity
- Educate on medication adherence for antiplatelets, statins, antihypertensives, and glycemic control agents
- Monitor and support risk factor management (cholesterol, glucose, blood pressure)
Psychosocial Support:
- Assess emotional response; provide counseling and psychological support as needed
- Encourage family involvement and educate on warning signs of recurrence
- Refer to cardiac rehabilitation programs
Care Considerations for Patients with Bifurcation Lesions
Bifurcation lesions require specialized consideration due to their complexity in both medical and interventional management.
- Technical Interventions: Be aware that treatment may involve advanced stenting techniques—such as provisional stenting, double stenting (culotte, crush, T-stenting)—which carry unique risks and require close hemodynamic monitoring.
- Risk Assessment: Monitor for restenosis, stent thrombosis, and impaired perfusion to side branches. Report any new chest pain or ECG changes promptly.
- Medication Management: Administer dual antiplatelet therapy as prescribed. Monitor for signs of bleeding or hematologic complications.
Patient and Family Education
Education is a cornerstone of care, empowering patients and families to manage CAD and prevent complications.
- Explain the nature of bifurcation blockages and why they are more complex than single-vessel disease.
- Describe the purpose and expectations of diagnostic and therapeutic procedures.
- Reinforce the importance of medication adherence and regular follow-up visits.
- Provide written and verbal information on lifestyle changes and symptom recognition.
- Discuss the signs and symptoms that require immediate medical attention (e.g., chest pain, shortness of breath, palpitations, syncope).
Complication Prevention and Management
Nurses must remain vigilant for both acute and chronic complications in CAD patients with bifurcation lesions.
- Acute Complications: Myocardial infarction, arrhythmias, cardiogenic shock, access site bleeding, renal impairment from contrast media.
- Long-Term Complications: In-stent restenosis, stent thrombosis, chronic angina, heart failure.
- Prevention Strategies: Adhere to infection prevention protocols, monitor for allergic reactions to contrast agents, encourage early mobilization post-procedure, and support cardiac rehabilitation.
Interdisciplinary Collaboration
Optimal outcomes are achieved when nurses collaborate with a multidisciplinary team, including cardiologists, interventional radiologists, pharmacists, dietitians, physical therapists, and social workers. Regular case conferences and collaborative care planning are encouraged to address the complex needs of patients with bifurcation blockages.
Documentation and Ongoing Evaluation
Accurate, timely documentation is essential for legal, clinical, and quality improvement purposes.
- Record all assessments, interventions, patient responses, and education provided.
- Evaluate patient progress and modify care plans as required.
- Ensure clear handover communication to subsequent care providers.
REFERENCES
- American College of Cardiology (ACC). From the Starting Line | Left Main Bifurcation Stenting: Tips and Tricks. https://www.acc.org/Latest-in-Cardiology/Articles/2021/12/01/01/42/Left-Main-Bifurcation-Stenting-Tips-and-Tricks.
- Dąbrowski EJ, Kożuch M, Dobrzycki S. Left Main Coronary Artery Disease-Current Management and Future Perspectives. J Clin Med. 2022 Sep 28;11(19):5745. doi: 10.3390/jcm11195745. PMID: 36233613; PMCID: PMC9573137.
- Dash D. Recent perspective on coronary artery bifurcation interventions. Heart Asia. 2014 Feb 14;6(1):18-25. doi: 10.1136/heartasia-2013-010451. PMID: 27326157; PMCID: PMC4832703.
- De Luca L. Percutaneous Treatment of Coronary Bifurcation Lesions. https://www.ahajournals.org/doi/10.1161/CIRCINTERVENTIONS.116.004328. Circulation: Cardiovascular Interventions. 2016 Sep;9(9):
- Gwon HC. Understanding the Coronary Bifurcation Stenting. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5986747/. Korean Circ J. 2018 Jun;48(6):481-491.
- Chang, CF., Chang, KH., Lai, CH. et al. Clinical outcomes of coronary artery bifurcation disease patients underwent Culotte two-stent technique: a single center experience. BMC Cardiovasc Disord 19, 208 (2019). https://doi.org/10.1186/s12872-019-1192-2
- Latib A, Colombo A. Bifurcation Disease: What Do We Know, What Should We Do?. https://www.sciencedirect.com/science/article/pii/S1936879808001684JACC: Cardiovascular Interventions. 2008 Jun;1(3):218-226.
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





