Introduction
Burns are injuries to the skin and underlying tissues caused by heat, chemicals, electricity, radiation, or friction. They are among the most common household and workplace injuries, affecting people of all ages across India and globally. The severity of a burn depends on its depth, size, and location, as well as the source of injury. Burns can range from minor, superficial wounds to life-threatening conditions requiring urgent medical attention.
Types of Burns
1. Thermal Burns
Thermal burns are the most common type, resulting from direct contact with heat sources. These include flames, hot liquids (scalds), steam, and hot objects. In India, kitchen accidents, firecrackers during festivals, and workplace mishaps are frequent causes. Thermal burns can occur in homes, workplaces, or public spaces and vary in severity depending on the duration and intensity of exposure.
2. Chemical Burns
Chemical burns result from exposure to corrosive substances, such as acids, alkalis, or solvents. Common sources include household cleaning agents, industrial chemicals, and accidental spills in laboratories or factories. Chemical burns can affect not only the skin but also the eyes, respiratory tract, and digestive system if inhaled or ingested. The severity depends on the chemical’s strength, concentration, and duration of contact.
3. Electrical Burns
Electrical burns occur when an electric current passes through the body, causing damage to tissues. Sources include faulty wiring, exposed electrical appliances, lightning strikes, and contact with power lines. Electrical burns may appear minor on the skin but can cause significant internal injuries, including damage to nerves, muscles, and organs. Immediate medical attention is essential for such injuries.
4. Radiation Burns
Radiation burns are caused by exposure to ultraviolet (UV) rays, X-rays, or other forms of radiation. Sunburn is the most common example, especially in tropical climates like India’s. Radiation therapy for cancer and industrial accidents with radioactive materials can also lead to burns. The severity depends on the dose and duration of exposure.
5. Friction Burns
Friction burns result from skin rubbing against a rough surface, generating heat and causing tissue damage. Common examples include road rash from motor vehicle accidents and injuries from sports activities. These burns are often superficial but can be painful and prone to infection.
Causes of Burns: Common Sources and Risk Factors
Burns can occur in various settings and are often preventable. Understanding the sources and risk factors helps individuals and families take proactive measures.
- Household accidents: Hot water, cooking oil, gas stoves, irons, and electrical appliances.
- Workplace hazards: Factories, construction sites, laboratories, and industries using chemicals or high temperatures.
- Fire-related incidents: House fires, firecrackers during festivals, candle mishaps, and open flames.
- Chemical exposure: Cleaning agents, pesticides, battery acid, and industrial chemicals.
- Electricity: Faulty wiring, exposed cords, electrical repairs without safety precautions.
- Radiation: Prolonged sun exposure, tanning beds, radiation therapy, and accidental exposure to radioactive materials.
- Friction: Road accidents, sports injuries, and falls.
Risk factors include age (children and elderly are more vulnerable), lack of safety equipment, poor awareness, and unsafe practices at home or work.
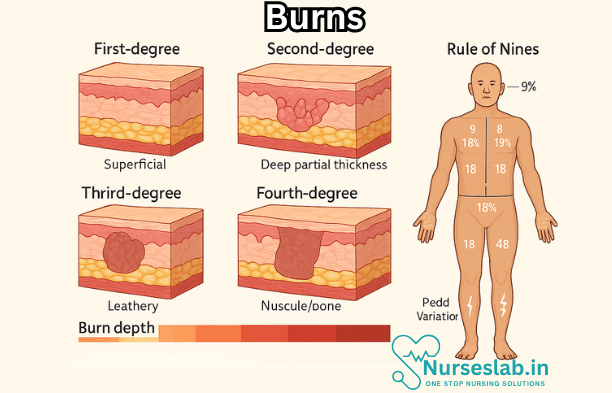
Symptoms and Severity: Classification by Degree, Signs, and Symptoms
Burns are classified based on their depth and the extent of tissue damage. Recognising the severity is crucial for appropriate treatment.
First-Degree Burns (Superficial)
These burns affect only the outer layer of skin (epidermis). Symptoms include redness, mild pain, and swelling. The skin may be dry without blisters. Common causes are sunburn and brief contact with hot objects. First-degree burns usually heal within a week without scarring.
Second-Degree Burns (Partial Thickness)
Second-degree burns involve the epidermis and part of the dermis (deeper skin layer). Symptoms include intense pain, redness, swelling, and blistering. The area may appear wet or shiny. Healing may take two to three weeks, and there is a risk of scarring or pigmentation changes.
Third-Degree Burns (Full Thickness)
Third-degree burns destroy both the epidermis and dermis, potentially affecting underlying tissues such as fat, muscles, and bones. The skin may appear white, charred, or leathery. Sensation is often lost due to nerve damage. These burns require immediate medical attention and often need surgical intervention. Healing is slow and scarring is inevitable.
Fourth-Degree Burns
These are the most severe, extending into muscle, bone, and deeper structures. The skin may be blackened or exposed, and there is often no pain due to extensive nerve damage. Fourth-degree burns are life-threatening and require complex treatment.
Other Signs and Symptoms
- Swelling and blistering
- Peeling skin
- Shock (pale, clammy skin, rapid pulse, dizziness)
- Difficulty breathing (especially with facial burns or inhalation injuries)
- Infection (redness, pus, fever)
Diagnosis
Diagnosing burns involves a thorough clinical assessment to determine severity, cause, and the best course of treatment.
- Physical examination: Doctors assess the burn’s size, depth, and location. The “Rule of Nines” is often used to estimate the percentage of body surface area affected.
- Medical history: Information on how the burn occurred, timing, and any previous medical conditions.
- Laboratory tests: Blood tests may be done to check for infection, dehydration, or organ involvement (especially in severe burns).
- Imaging: X-rays, CT scans, or MRIs may be ordered if deeper tissue damage or inhalation injury is suspected.
- Monitoring vital signs: Blood pressure, heart rate, respiratory rate, and oxygen levels are closely monitored.
Early and accurate diagnosis is critical for guiding treatment and preventing complications.
Treatment
First Aid for Burns
Immediate first aid can make a significant difference in outcomes. Here are key steps to follow:
- Remove the person from the source of the burn.
- Cool the burn with running cool (not cold) water for at least 10 minutes. Do not use ice.
- Remove jewellery, watches, or clothing near the burn unless stuck to the skin.
- Cover the burn with a clean, non-stick cloth or sterile dressing.
- Do not apply butter, oil, toothpaste, or other home remedies to the burn.
- If blisters form, do not burst them.
- Seek medical attention for burns larger than a palm, deep burns, burns on the face, hands, feet, genitals, or over major joints.
Medical Treatment
Treatment depends on burn severity, location, and overall health.
- Minor burns: Clean with mild soap and water, apply antibiotic ointment, and cover with a sterile dressing. Pain relief with paracetamol or ibuprofen may be recommended.
- Moderate to severe burns: Hospital admission may be required. Treatments include intravenous fluids, pain management, wound care, and antibiotics to prevent or treat infection.
- Burn dressings: Special dressings keep wounds moist, promote healing, and prevent infection.
- Tetanus vaccination: May be given if vaccination status is uncertain.
Surgical Procedures
- Debridement: Removal of dead tissue to promote healing.
- Skin grafts: Healthy skin from another part of the body is transplanted to cover large wounds.
- Reconstructive surgery: Needed for severe burns affecting function or appearance, especially on the face, hands, or joints.
- Physical therapy: Helps restore movement and prevent stiffness.
Other Supportive Care
- Nutrition: High-protein, high-calorie diet supports healing.
- Hydration: Prevents dehydration from fluid loss.
- Pain management: Medications and non-drug therapies are important for comfort.
- Psychological support: Counselling may be needed for trauma, anxiety, or depression following severe burns.
Complications
Burns can lead to serious complications, particularly if not treated promptly and properly.
Infection
Burn wounds are susceptible to bacterial, fungal, and viral infections. Signs include increased redness, swelling, pus, fever, and delayed healing. Severe infection can lead to sepsis, a life-threatening condition.
Scarring and Contractures
Deep burns often result in scarring, which may affect appearance and movement. Contractures—tightening of skin and underlying tissues—can restrict mobility, especially when joints are involved. Reconstructive surgery and physiotherapy may be needed.
Shock
Severe burns can lead to shock due to fluid loss and tissue damage. Symptoms include pale skin, rapid pulse, low blood pressure, and confusion. Shock is a medical emergency requiring immediate treatment.
Organ Damage
Electrical and deep burns may damage internal organs, muscles, and bones, leading to long-term health issues. Kidney failure, respiratory problems, and heart complications are possible.
Emotional and Psychological Effects
Burn injuries can cause emotional distress, anxiety, depression, and post-traumatic stress. Support from family, friends, and professionals is vital for recovery.
Prevention Strategies
Most burns are preventable with simple precautions. Here are practical tips for reducing risk at home, work, and in public areas:
- Kitchen safety: Keep hot liquids and foods away from children. Use potholders and avoid wearing loose clothing near open flames.
- Electrical safety: Regularly check wiring, use proper plugs, and avoid overloading sockets. Keep electrical appliances away from water.
- Chemical safety: Store chemicals out of reach of children, use protective gloves and eyewear, and follow instructions carefully.
- Fire safety: Install smoke alarms, have fire extinguishers, and plan escape routes. Be cautious with candles, firecrackers, and matches.
- Sun protection: Use sunscreen, wear protective clothing, and avoid prolonged exposure during peak UV hours (10 am to 4 pm).
- Workplace safety: Follow safety protocols, wear protective gear, and attend training sessions.
- Road safety: Wear helmets, seat belts, and appropriate clothing during travel or sports.
Educating children and vulnerable groups, promoting awareness, and regular safety checks are key to prevention.
Recovery and Rehabilitation
Recovery from burns varies based on severity, location, and individual health. It involves physical healing, emotional support, and rehabilitation.
Healing Process
Minor burns heal within days to weeks, while severe burns may take months or years. The process includes:
- Inflammation: The body responds with redness and swelling.
- Proliferation: New tissue forms to cover the wound.
- Remodelling: The skin strengthens and scars mature over time.
Physical Rehabilitation
- Physiotherapy to restore movement, especially for burns over joints.
- Occupational therapy to assist with daily activities and independence.
- Use of splints and exercises to prevent contractures and improve function.
Emotional and Psychological Support
- Counselling for trauma, anxiety, or depression.
- Support groups for patients and caregivers.
- Family involvement to provide encouragement and understanding.
Social and Vocational Rehabilitation
- Assistance with returning to work or school.
- Training and education for new skills if necessary.
- Advocacy for disability rights and inclusion.
Nursing Care of Patients with Burns
Nurses play a crucial role in the management, recovery, and rehabilitation of burn patients. Effective nursing care not only minimises complications but also promotes healing and improves the overall quality of life for patients.
Initial Assessment and Emergency Management
Immediate nursing intervention is critical:
- Airway, Breathing, Circulation (ABC): Assess and maintain airway, monitor breathing, and check circulatory status. Inhalation injury may require advanced airway management.
- Remove the Source: Stop the burning process by removing the patient from the source and removing any clothing or jewellery near the burn site (unless stuck to the skin).
- Cool the Burn: Apply cool (not cold) running water to the affected area for 10-20 minutes to halt further tissue damage. Avoid ice or very cold water.
- Prevent Hypothermia: Keep the patient warm, especially if large areas are affected.
- Monitor Vital Signs: Regular checks for pulse, blood pressure, respiratory rate, and oxygen saturation.
Fluid Resuscitation
Major burns (>15% total body surface area in adults) can lead to significant fluid loss. Nurses must monitor for signs of hypovolemic shock and initiate intravenous fluid therapy as per protocols (e.g., Parkland formula). Accurate input/output charting and regular assessment of urine output are essential.
Pain Management
Burns are extremely painful. Administer prescribed analgesics and sedatives, and assess pain regularly using appropriate pain scales. Non-pharmacological methods such as distraction, relaxation techniques, and family support also help in pain management.
Wound Care and Infection Prevention
Proper wound care is vital to prevent infection and promote healing:
- Cleansing: Gently clean wounds with sterile saline or prescribed solutions.
- Dressing: Apply sterile, non-adherent dressings; change dressings as per protocol, ensuring aseptic technique.
- Observation: Monitor for signs of infection (redness, swelling, pus, fever).
- Topical Antimicrobials: Use as prescribed to minimise infection risk.
Nutritional Support
Burn patients have increased metabolic demands. Provide a high-calorie, high-protein diet to support healing. Enteral nutrition may be needed for those unable to eat orally. Monitor nutritional status and consult with dietitians as necessary.
Psychosocial Care
Burn injuries can cause significant emotional distress. Nurses should offer psychological support, encourage family involvement, and refer patients to counselling or support groups as required.
Rehabilitation and Mobility
Early mobilisation and physiotherapy help prevent contractures and maintain function. Assist with active and passive exercises, and educate patients and families on the importance of rehabilitation.
Patient and Family Education
Educate patients and their families regarding wound care, signs of complications, the importance of nutrition, and follow-up care. Provide clear instructions and address any queries to ensure compliance and recovery.
Prevention of Complications
Monitor for and manage potential complications such as:
- Infection
- Sepsis
- Respiratory distress
- Contractures
- Psychological issues
Early detection and intervention are essential to minimise morbidity and mortality.
REFERENCES
- Burns. In: Hamm R, Carey JN, eds. Essential Elements of Wound Diagnosis. McGraw Hill; 2021.
- Collier ZJ, Carey JN, Gillenwater T. Burn Wound Management. In: Hamm RL. eds. Text and Atlas of Wound Diagnosis and Treatment. 3rd ed. McGraw Hill; 2024.
- Guzman E, Oropello JM. Critical Care of Burn Patients. In: Oropello JM, Pastores SM, Kvetan V, eds. Critical Care. McGraw-Hill Education; 2017.
- Keum H, Cevik E, Kim J, et al. Tissue Ablation: Applications and Perspectives. https://pubmed.ncbi.nlm.nih.gov/38771628/. Adv Mater. 2024 May;36(32):e2310856.
- Levi B, Wang S. Burns. In: Kang S, Amagai M, Bruckner AL, Enk AH, Margolis DJ, McMichael AJ, Orringer JS, eds. Fitzpatrick’s Dermatology. 9th ed. McGraw-Hill Education; 2019.
- Nielson CB, Duethman NC, Howard JM, Moncure M, Wood JG. Burns: Pathophysiology of Systemic Complications and Current Management. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5214064/. J Burn Care Res. 2017 Jan;38(1):e469-e481.
- Wei J, Meng L, Hou X, et al. Radiation-induced skin reactions: mechanism and treatment. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6306060/. Cancer Manag Res. 2018;11:167-177. Published 2018 Dec 21.\.
- Wolf SE. Burns. In: Townsend CM, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery. 21st ed. Elsevier Inc. 2022:484-505.
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





