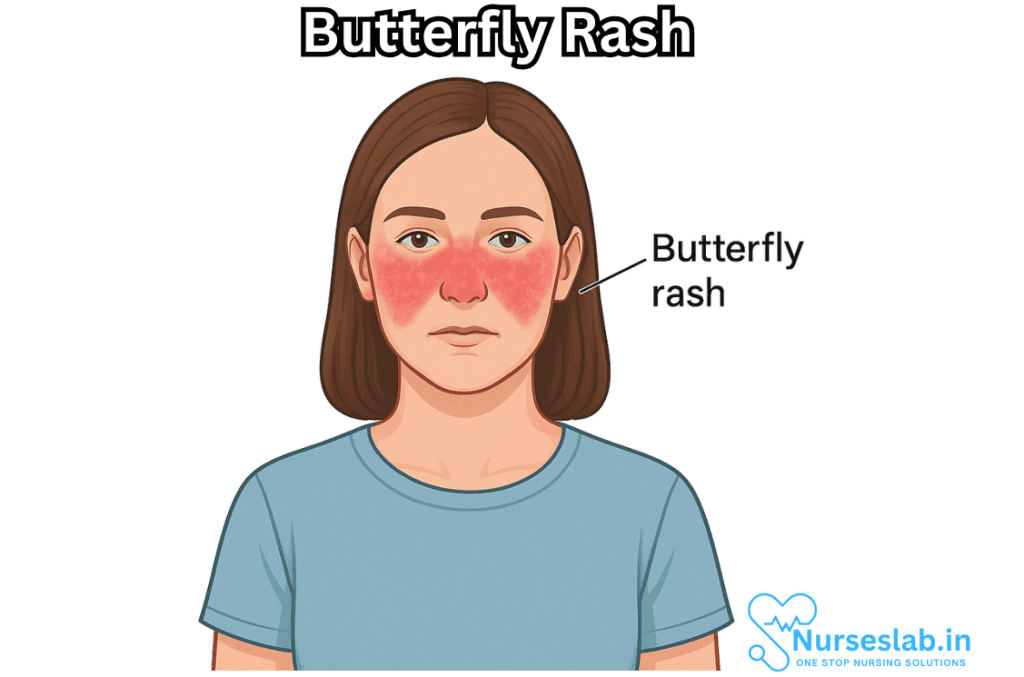
Butterfly rash, also known as malar rash, is a distinctive red or purplish rash that appears across the cheeks and the bridge of the nose, resembling the shape of a butterfly. This clinical sign is most famously associated with systemic lupus erythematosus (SLE), an autoimmune disease, but it can also be seen in a variety of other medical conditions. Recognizing a butterfly rash is crucial for early diagnosis and management of underlying diseases, making it an important topic in dermatology and rheumatology.
What is a Butterfly Rash?
A butterfly rash is a symmetrical erythematous (red) rash that covers the malar (cheek) areas of the face and extends over the nose, sparing the nasolabial folds (the skin creases running from each side of the nose to the corners of the mouth). The rash can vary in intensity—ranging from mild redness to pronounced swelling and scaling. It may be flat or slightly raised and is often sensitive to sunlight (photosensitive).
Causes of Butterfly Rash
While the butterfly rash is most commonly associated with SLE, it can also be triggered by other conditions. The major causes include:
- Systemic Lupus Erythematosus (SLE): The most classic and common cause of a butterfly rash. SLE is an autoimmune disease in which the immune system attacks healthy tissues.
- Rosacea: A chronic skin condition that causes facial redness and may mimic a butterfly pattern, but usually lacks the sharp demarcation and association with systemic symptoms.
- Dermatomyositis: An inflammatory disease marked by muscle weakness and characteristic rashes, including facial involvement.
- Seborrheic Dermatitis: Can occasionally present with a similar pattern but generally affects more areas and may have scaling.
- Other Causes: Certain viral infections (like parvovirus B19, which causes “slapped cheek” rash), adverse drug reactions, and rare genetic syndromes.
Pathophysiology
In autoimmune causes such as lupus, the butterfly rash develops due to inflammation of small blood vessels in the skin—often triggered or exacerbated by exposure to ultraviolet (UV) light. The immune system creates antibodies that attack skin cells, leading to the characteristic rash. In other conditions, mechanisms may include chronic inflammation, hypersensitivity reactions, or direct irritation of facial blood vessels.
Clinical Features
The typical presentation of a butterfly rash includes:
- Location: Symmetric involvement of both cheeks and the bridge of the nose, sparing the nasolabial folds.
- Appearance: Red or purplish color, flat or raised, sometimes with slight swelling or scaling.
- Photosensitivity: Worsening with exposure to sunlight is common, especially in lupus.
- Associated Symptoms: In systemic conditions like SLE, there may be joint pain, fatigue, fever, oral ulcers, and internal organ involvement.
- Duration: Can be transient or persistent, depending on the underlying cause and treatment.
Distinguishing Features
It is important to distinguish a butterfly rash from other facial rashes:
- Lupus Butterfly Rash: Often sharply demarcated, non-itchy, and photosensitive.
- Rosacea: Usually accompanied by flushing, visible blood vessels, and sometimes pimples.
- Seborrheic Dermatitis: More likely to involve the scalp, eyebrows, and nasolabial folds with greasy scales.
Diagnosis
Correct identification of a butterfly rash requires a thorough clinical evaluation. The diagnostic process involves:
- Detailed History: Including symptom onset, duration, possible triggers (such as sun exposure), associated systemic symptoms, and medication history.
- Physical Examination: Careful inspection of the rash, looking for symmetry, borders, and signs of systemic involvement.
- Laboratory Tests: In suspected SLE, tests may include antinuclear antibodies (ANA), anti-dsDNA, anti-Smith antibodies, complete blood count (CBC), and markers of kidney and liver function.
- Skin Biopsy: In uncertain cases, a small sample of skin may be examined under the microscope to help distinguish between causes.
- Phototesting: To assess for photosensitivity if not clear from history.
Associated Conditions
While lupus is the most well-known and serious association, clinicians must be aware of other causes:
- Systemic Lupus Erythematosus (SLE): Along with butterfly rash, patients can develop arthritis, nephritis (kidney inflammation), pleuritis (lung inflammation), pericarditis (heart inflammation), and neurological issues.
- Dermatomyositis: May present with a heliotrope rash (purplish discoloration around eyes), muscle weakness, and other characteristic rashes (Gottron’s papules).
- Rosacea: Chronic redness, swelling, and sometimes pustules. Unlike lupus, systemic symptoms are usually absent.
Management and Treatment
Treatment of a butterfly rash depends on the underlying cause. Key management strategies include:
- Sun Protection: Avoidance of direct sunlight, use of broad-spectrum sunscreen, protective clothing, and hats.
- Topical Treatments: Corticosteroid creams may be used for inflammation; calcineurin inhibitors for sensitive areas.
- Systemic Therapy: In cases of SLE or dermatomyositis, oral medications such as corticosteroids, antimalarials (like hydroxychloroquine), immunosuppressants, or biologic drugs may be required.
- Skin Care: Gentle skin cleansing and moisturizing to prevent irritation and promote healing.
- Lifestyle Adjustments: Patients may benefit from stress reduction, healthy diet, and regular follow-up with healthcare providers.
Addressing Underlying Disease
Since butterfly rash is often a marker of systemic disease, long-term management focuses on controlling the primary illness (e.g., SLE). This often requires a multidisciplinary approach involving rheumatologists, dermatologists, and primary care providers.
Prognosis
The prognosis of a butterfly rash depends on both its severity and the underlying condition. In SLE, for example, early recognition and comprehensive management can prevent organ damage and improve quality of life. Isolated butterfly rash due to skin-only involvement is usually less severe but should be monitored for systemic features.
When to Seek Medical Attention
Because a butterfly rash can be the first sign of a serious underlying disease, individuals noticing a new or unexplained rash over the cheeks and nose should seek prompt medical evaluation, especially if there are associated symptoms such as fatigue, joint pain, fever, or unexplained weight loss
Nursing Care of Patients with Butterfly Rash (Malar Rash)
Caring for patients displaying a butterfly rash requires a comprehensive nursing approach, not only to address the cutaneous symptoms but also to support the patient’s overall health and quality of life, considering the potential systemic involvement of diseases like SLE.
Assessment and Identification
- Physical Assessment: Observe and document the appearance, distribution, color, and texture of the rash. Note any associated symptoms such as swelling, pain, burning, or pruritus (itching).
- History Taking: Obtain a detailed medical history, including onset and duration of the rash, any identified triggers (e.g., sun exposure), and associated systemic symptoms such as joint pain, fever, fatigue, or photosensitivity.
- Systemic Review: Since malar rash often points toward SLE, inquire about other organ system involvements such as renal, cardiac, pulmonary, or neurological symptoms.
- Allergy and Medication Review: Review current and past medications, allergies, and any new products applied to the skin to rule out drug-induced rashes or contact dermatitis.
Nursing Diagnoses
- Impaired skin integrity related to autoimmune process as evidenced by malar rash.
- Risk for infection related to open skin lesions.
- Disturbed body image related to visible skin changes.
- Acute or chronic pain related to skin lesions and systemic disease activity.
- Deficient knowledge regarding disease process and self-care.
- Risk for impaired social interaction due to visible facial rash.
Nursing Interventions and Management
1. Skin Care Management
- Gentle Cleansing: Advise the use of mild, fragrance-free cleansers. Instruct the patient to avoid scrubbing the affected areas, which can worsen irritation.
- Moisturization: Recommend non-comedogenic, hypoallergenic moisturizers to prevent excessive dryness and scaling.
- Sun Protection: Emphasize the importance of strict photoprotection. Advise wearing broad-spectrum sunscreen (SPF 30 or higher) daily, even indoors if near windows. Encourage the use of wide-brimmed hats and protective clothing.
- Avoidance of Triggers: Identify and help the patient avoid known triggers—such as stress, strong sunlight, or specific skincare products—that could exacerbate the rash.
- Topical Medications: Administer prescribed topical corticosteroids or immunomodulators as directed by the physician. Monitor for side effects such as skin thinning or irritation.
- Monitoring: Routinely monitor the rash for signs of worsening, infection (such as increased redness, pus, or pain), or spread to other areas. Report significant changes to the healthcare provider promptly.
2. Systemic Management (for Underlying Conditions)
- Medication Adherence: Encourage adherence to systemic medications, such as antimalarials (e.g., hydroxychloroquine), corticosteroids, or immunosuppressants as prescribed for SLE or other causes.
- Monitor for Side Effects: Watch for medication side effects, such as gastrointestinal symptoms, mood changes, or signs of infection, and report them as necessary.
- Lab Monitoring: Facilitate regular laboratory assessments (blood counts, kidney function, etc.) as ordered, since SLE may involve multiple organ systems.
3. Infection Prevention
- Hygiene Education: Teach the patient proper hand hygiene and skin care to minimize secondary infection risk.
- Wound Care: If lesions become open or weepy, instruct on gentle cleaning and application of sterile, non-stick dressings as needed.
- Observation: Monitor for systemic signs of infection (fever, malaise) and local signs (increased warmth, swelling, purulent discharge) and report immediately.
4. Pain and Discomfort Management
- Coping Strategies: Encourage the use of cold compresses to relieve burning or itching sensations, as appropriate.
- Pharmacologic Support: Administer analgesics or anti-inflammatory medications as prescribed, and monitor their effectiveness.
- Positioning: Advise the patient to avoid prolonged pressure on affected areas and to sleep on their back if possible.
5. Psychosocial Support
- Body Image: Acknowledge the emotional and psychological impact of visible facial rashes. Offer support and encourage open expression of feelings.
- Counseling and Support Groups: Refer the patient to counseling, peer support groups, or patient networks for individuals with SLE or chronic skin conditions.
- Social Interaction: Support participation in social activities and provide strategies to cope with any stigma or negative reactions from others.
6. Patient and Family Education
- Understanding the Disease: Educate about the nature of butterfly rash and its relationship to underlying systemic conditions, particularly SLE.
- Medication Use: Instruct on the correct use, timing, and potential side effects of prescribed medications.
- Self-Monitoring: Teach the patient to recognize early warning signs of flare-ups or complications and when to seek medical attention.
- Lifestyle Modifications: Encourage a balanced diet, adequate rest, and stress reduction techniques, as these can help control autoimmune activity.
Collaborative Care
- Collaborate with dermatologists, rheumatologists, and other specialists involved in the patient’s care.
- Coordinate with nutritionists for dietary advice if systemic disease is present.
- Assist in the scheduling and follow-up of laboratory and imaging investigations as needed.
Evaluation and Follow-up
- Regularly assess the skin for improvements or deterioration.
- Monitor patient’s adherence to treatment and self-care routines.
- Evaluate psychosocial health and quality of life using standardized tools when appropriate.
- Review and update nursing care plans based on the patient’s changing needs and treatment response.
REFERENCES
- American Academy of Dermatology (AAD) Association. Lupus and Your Skin: Overview. https://www.aad.org/public/diseases/a-z/lupus-overview. Last updated 9/23/2022.
- Raharja A, Mahil SK, Barker JN. Psoriasis: A brief overview. Clin Med (Lond). 2021;21(3):170-173. doi:10.7861/clinmed.2021-0257
- Gisondi P, Bellinato F, Girolomoni G. Clinical characteristics of patients with pustular psoriasis: a single-center retrospective observational study. Vaccines. 2022;10(8):1171. doi:10.3390/vaccines10081171
- Cooper EE, Pisano CE, Shapiro SC. Cutaneous manifestations of “lupus”: systemic lupus erythematosus and beyond. Int J Rheumatol. 2021;2021:6610509. doi:10.1155/2021/6610509
- Lupus Foundation of America. Lupus and the Skin,. https://www.lupus.org/resources/how-lupus-affects-the-skin. Last updated 8/26/2021.
- Lupus Research Alliance (U.S.). Lupus Signs and Symptoms. https://www.lupusresearch.org/understanding-lupus/what-is-lupus/symptoms/. Last modified 7/1/2024.
- Ezeofor AJ, O’Connell KA, Cobos GA, Vleugels RA, LaChance AH, Nambudiri VE. Distinctive cutaneous features of dermatomyositis in Black adults: a case series. JAAD Case Rep. 2023;37:106-109. doi:10.1016/j.jdcr.2023.05.019
- Naji Rad S, Vashisht P. Malar Rash. https://www.ncbi.nlm.nih.gov/books/NBK555981/. 2023 Sep 4. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan.
- Ingrasci G, Tornes L, Brown A, et al. Chronic pruritus in multiple sclerosis and clinical correlates. J Eur Acad Dermatol Venereol. 2023;37(1):154-159. doi:10.1111/jdv.18561
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





