Capgras syndrome (Capgras delusion) is a type of delusional misidentification syndrome. You believe a family member or close friend is an imposter. Certain neurological conditions or mental health conditions increase risk of Capgras syndrome. Treatment includes antipsychotic medication and managing the underlying condition.
Introduction
Capgras Syndrome, also known as the Capgras delusion, is a rare and fascinating psychological disorder that disrupts the very fabric of personal identity and recognition. Individuals affected by this condition hold the persistent belief that someone close to them — often a spouse, family member, or friend — has been replaced by an identical impostor. This delusion extends, in some cases, to pets, personal belongings, or even themselves. First described in 1923 by French psychiatrist Joseph Capgras and his colleague Jean Reboul-Lachaux, Capgras Syndrome offers a unique window into the complex workings of the human mind, shedding light on the interplay between perception, memory, and emotion.
Historical Background
The syndrome was named after Joseph Capgras, who documented the case of a woman convinced that various people in her life were replaced by doubles. Capgras originally called the phenomenon “l’illusion des sosies,” meaning “the illusion of doubles.” Since its initial description, the syndrome has been observed in a variety of psychiatric, neurological, and medical contexts, but it remains a rare and poorly understood condition.
Symptoms and Presentation
The hallmark of Capgras Syndrome is the delusional misidentification of familiar individuals. This presentation can be startling and distressing for both the affected person and those around them. Common symptoms include:
- Belief that a loved one has been replaced: The individual is convinced that a close relative or friend is an impostor, identical in appearance but fundamentally different or harmful.
- Emotional detachment: A lack of emotional response or recognition for the “impostor,” even if the person looks and acts exactly as expected.
- Suspicion and paranoia: The delusion may extend to suspicion that the impostor has malicious intent or is part of a conspiracy.
- Extension of delusion: In some cases, the belief is not limited to people; pets, objects, or even the self may be perceived as replaced or duplicated.
The intensity and duration of these symptoms can vary. Some individuals experience transient episodes, often triggered by stress, while others may develop chronic and persistent delusional beliefs.
Underlying Mechanisms
Capgras Syndrome is most commonly associated with psychiatric disorders such as schizophrenia, schizoaffective disorder, and bipolar disorder. However, it has also been documented in people with brain injuries, neurodegenerative diseases (such as Alzheimer’s and Lewy body dementia), and other neurological conditions.
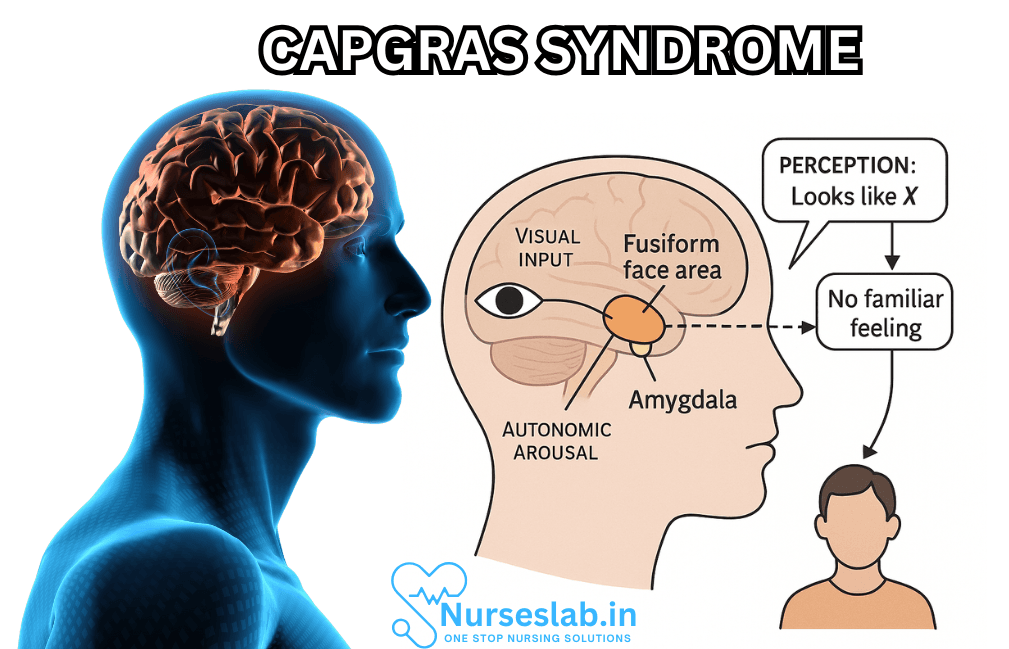
The prevailing theories suggest that Capgras Syndrome arises from a disconnect between facial recognition systems and emotional processing centers in the brain. Specifically, the fusiform gyrus, responsible for recognizing faces, may function normally; the individual can visually identify a loved one. However, the limbic system, particularly the amygdala — which attaches emotional significance to recognized faces — fails to activate. This lack of emotional resonance leads the individual to believe that the person must be an impostor, despite physical evidence to the contrary.
Neurological studies using functional imaging have shown that patients with Capgras Syndrome may have disrupted connections between the temporal lobes (involved in perception and memory) and the frontal lobes (involved in reasoning and judgment). Lesions, trauma, or degenerative changes affecting these areas can trigger the syndrome.
Associated Conditions and Risk Factors
Capgras Syndrome is not a diagnosis in itself but rather a symptom or manifestation within a broader context of mental or neurological illness. The most frequent associations include:
- Schizophrenia: Capgras delusion is one of several misidentification syndromes found in schizophrenia, alongside Fregoli delusion and intermetamorphosis.
- Dementia: Alzheimer’s disease and Lewy body dementia can produce Capgras Syndrome, especially as the disease progresses and cognitive decline deepens.
- Brain injury: Traumatic brain injuries, strokes, or lesions affecting the right hemisphere, particularly the temporal or frontal lobes, have been linked to Capgras delusion.
- Bipolar disorder: During manic or psychotic episodes, individuals may experience transient Capgras-like symptoms.
- Other psychiatric conditions: Depression with psychotic features, obsessive-compulsive disorder, and personality disorders have very occasionally been associated with Capgras delusion.
Additionally, certain medications, substance abuse, or metabolic disturbances can precipitate or worsen symptoms.
Diagnosis
Diagnosing Capgras Syndrome requires careful clinical assessment by a mental health professional or neurologist. The process typically involves:
- Detailed interview: Understanding the nature and extent of delusional beliefs, their onset, duration, and impact on daily life.
- Medical and psychiatric history: Reviewing past illnesses, injuries, medications, and psychosocial stressors.
- Neuropsychological assessment: Evaluating cognitive function, memory, executive skills, and facial recognition abilities.
- Imaging studies: MRI or CT scans may be ordered to identify structural brain abnormalities, lesions, or atrophy.
- Rule out other causes: Excluding conditions such as delirium, intoxication, or other psychoses that might explain the symptoms.
There are no specific laboratory tests for Capgras Syndrome; diagnosis rests on clinical expertise and observation.
Impact on Patients and Families
The emotional toll of Capgras Syndrome can be profound. For the individual, the experience is disorienting, frightening, and sometimes isolating. For families and caregivers, being perceived as impostors can cause heartbreak, frustration, and disruption of the relationship. Trust is eroded, and communication becomes challenging. In some cases, the delusion leads to aggression, withdrawal, or refusal of care, especially in dementia patients.
Caregivers require education, support, and compassion as they navigate the complexities of the syndrome, often seeking validation and help from professionals and peer groups.
Treatment and Management
No single treatment is universally effective for Capgras Syndrome; management is tailored to the underlying condition and the individual’s needs. Key approaches include:
- Pharmacological therapy: Antipsychotic medications (such as risperidone, olanzapine, or aripiprazole) are commonly prescribed for patients with schizophrenia or severe delusions. In cases related to dementia, cholinesterase inhibitors or memantine may be beneficial. Mood stabilizers and antidepressants can help if the syndrome occurs in bipolar disorder or depression.
- Psychotherapy: Cognitive-behavioral therapy (CBT) can help patients challenge and reframe delusional beliefs. Supportive therapy and counseling offer coping strategies for both patients and families.
- Environmental modification: Creating a calm, familiar, and supportive environment can reduce distress and confusion, particularly for dementia patients.
- Education and support: Providing information to families and caregivers fosters understanding, patience, and resilience.
- Addressing underlying causes: Treating infections, metabolic imbalances, or substance abuse may resolve secondary cases of Capgras Syndrome.
Treatment goals are to alleviate distress, improve reality testing, and support the overall well-being of the patient and their loved ones.
Nursing Care of Patients with Capgras Syndrome
Nursing care for individuals with Capgras syndrome requires a deep understanding of the disorder, a strong foundation in psychiatric nursing principles, and above all, empathy and patience. This document provides a comprehensive guide to the nursing management of patients diagnosed with Capgras syndrome, outlining assessment, communication strategies, safety considerations, psychoeducation, and family support.
Assessment and Initial Nursing Approaches
Accurate assessment forms the cornerstone of effective nursing care. Initial steps include:
- Comprehensive Mental Status Examination: Evaluate for the presence of delusions, hallucinations, cognitive deficits, mood disturbances, and insight.
- Physical Assessment: Screen for neurological signs, head trauma, or other medical conditions that may contribute to the syndrome.
- History-Taking: Obtain a detailed history from the patient and family. Note the onset, triggers, and course of symptoms, previous psychiatric illness, and recent changes in medication or health status.
- Risk Assessment: Assess for potential harm to self or others. The delusion may provoke fear, paranoia, or aggression towards perceived impostors.
Nurses must approach assessment with sensitivity, as direct confrontation or questioning of the delusional belief may increase agitation or distress.
Communication Strategies
Effective communication is vital in fostering trust and reducing anxiety in patients with Capgras syndrome. The following principles are recommended:
- Validation and Empathy: Acknowledge the patient’s feelings without directly challenging the delusion. For example, say, “I see that this is very upsetting for you,” rather than, “That’s not your spouse.”
- Gentle Redirection: If the patient fixates on the delusion, gently redirect the conversation to less distressing topics or engaging activities.
- Consistency: Maintain consistent routines, staff assignments, and environments to minimize confusion and reduce triggers for misidentification.
- Calm Environment: Provide a quiet, structured setting to help decrease anxiety and agitation.
- Nonverbal Communication: Use calm body language, soft tone, and reassuring gestures. Nonverbal cues are especially important if the patient’s verbal comprehension is impaired.
- Avoid Arguing or Rationalizing: Directly disputing the delusion can heighten distress and erode trust. Instead, focus on the patient’s emotional experience.
Safety Considerations
The risk of harm can be significant in Capgras syndrome, especially if the patient perceives the ‘impostor’ as threatening. Nursing staff should:
- Monitor for signs of agitation, paranoia, or escalating anger towards identified ‘impostors’.
- Remove potential hazards from the patient’s environment.
- Ensure that the patient is supervised, particularly if there is a history of aggression or if delusional beliefs are intense.
- Collaborate with the multidisciplinary team to develop safety plans, including protocols for de-escalation and emergency intervention if necessary.
- Document all incidents thoroughly, noting triggers, behavioral responses, and interventions used.
Psychoeducation and Therapeutic Engagement
Patient and family education is a central component of nursing care. Although patients with fixed delusions may have limited insight, ongoing therapeutic engagement can support recovery and adaptation.
- Patient Education: Tailor information to the individual’s level of understanding and readiness. Focus on coping strategies, recognizing triggers, and stress management techniques.
- Family Education: Provide families with information about Capgras syndrome, emphasizing that the condition is a symptom of illness, not a personal failing. Teach strategies for communicating and managing challenging behaviors.
- Support Groups: Encourage participation in support groups, both for patients and family members. This can reduce isolation and foster shared learning.
- Medication Adherence: Educate about the importance of taking prescribed medications consistently and reporting side effects promptly.
Collaboration with the Multidisciplinary Team
Optimal care for Capgras syndrome requires teamwork:
- Psychiatrists: For diagnostic evaluation, medication management, and psychotherapy
- Neurologists: For assessment of underlying brain pathology, especially in cases with cognitive impairment
- Clinical Psychologists: For cognitive-behavioral therapy and psychological assessments
- Social Workers: To connect families to community resources and support structures
- Occupational Therapists: To assist with daily living skills and environment modification
Regular case reviews and open channels of communication among team members ensure comprehensive and coordinated care.
Pharmacological Management and Nursing Implications
While Capgras syndrome itself is not cured by medication, pharmacological interventions may be indicated to address underlying psychiatric or neurological conditions:
- Antipsychotics: Commonly used to treat delusional symptoms, especially in schizophrenia or severe agitation.
- Cholinesterase Inhibitors: For patients with dementia-related Capgras syndrome, these can help with cognitive symptoms.
- Antidepressants/Mood Stabilizers: May be necessary if comorbid depression or mood disorders are present.
Nurses play a key role in monitoring for side effects, ensuring adherence, and educating patients and families about medication regimens.
Managing Challenging Behaviors
Delusional misidentification can provoke a range of challenging behaviors. Nursing interventions should be individualized:
- Identify and minimize triggers for delusional episodes (e.g., unfamiliar settings, changes in routine).
- Use distraction and engagement in meaningful activities to redirect attention.
- De-escalate agitation promptly, using non-threatening body language and verbal reassurance.
- Involve the patient in decisions about their care as much as possible, to promote autonomy and reduce feelings of helplessness.
Supporting Family and Caregivers
Living with someone who has Capgras syndrome can be emotionally taxing for families. Nursing support should focus on:
- Listening empathetically to family members’ concerns and providing a nonjudgmental space for discussion.
- Offering guidance on how to respond to delusional beliefs without confrontation.
- Educating about the importance of self-care and the availability of respite services.
- Connecting families to counseling or therapy if needed.
Ethical and Legal Considerations
Ethical dilemmas may arise, especially when the patient’s safety is compromised or when they refuse necessary care. Nurses must:
- Respect patient autonomy whenever possible, within the constraints of safety.
- Advocate for the least restrictive interventions.
- Maintain confidentiality and dignity in all interactions.
- Be aware of local legal frameworks regarding involuntary treatment, guardianship, and capacity assessments.
REFERENCES
- Shah KP, Jain SB, Wadhwa R. Capgras Syndrome. 2023 May 29. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan–. PMID: 34033319.
- Anderson A, Filley C. Delusional Misidentification Syndromes: Progress and New Challenges. https://neuro.psychiatryonline.org/doi/10.1176/appi.neuropsych.16030055). The Journal of Neuropsychiatry and Clinical Neurosciences. 2016 July 22.
- Bushra Iftikhar, Ramneesh Baweja, Aniket Tatugade, et al.What do we know about delusional misidentification disorders? A focus on Capgras syndrome. . https://www.jneuropsychiatry.org/abstract/what-do-we-know-about-delusional-misidentification-disorders-a-focus-on-capgras-syndrome-6043.html Neuropsychiatry. 2012 Feb;2(2).
- Darby RR, Laganiere S, Pascual-Leone A, et al. Finding the imposter: brain connectivity of lesions causing delusional misidentifications. https://pubmed.ncbi.nlm.nih.gov/28082298/. Brain. 2017 Feb;140(2):497-507
- Koc AE, Hocaoglu C. What Is Capgras Syndrome? Diagnosis and Treatment Approach. IntechOpen; 2020. doi:10.5772/intechopen.91153
- Kyrtsos CR, Stahl MC, Eslinger P, et.al. Capgras Syndrome in a Patient with Parkinson’s Disease after Bilateral Subthalamic Nucleus Deep Brain Stimulation: A Case Report. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4464017/. Case Rep Neurol. 2015 May 21;7(2):127-33.
- Subbarayan D, Farhana J. Capgras syndrome. Pondicherry Journal of Nursing. 2020;13(2):46-48. doi:10.5005/jp-journals-10084-12151
- Pandis C, Agrawal N, Poole N. Capgras’ Delusion: A Systematic Review of 255 Published Cases. https://pubmed.ncbi.nlm.nih.gov/31326968/. Psychopathology. 2019 Jul;52(3):161-173. 10/8/2024.
- Salvatore P, Bhuvaneswar C, Tohen M, et al. Capgras’ syndrome in first-episode psychotic disorders/. https://pubmed.ncbi.nlm.nih.gov/24516070/. Psychopathology. 2014 Feb;47(4):261-9.
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





