Introduction
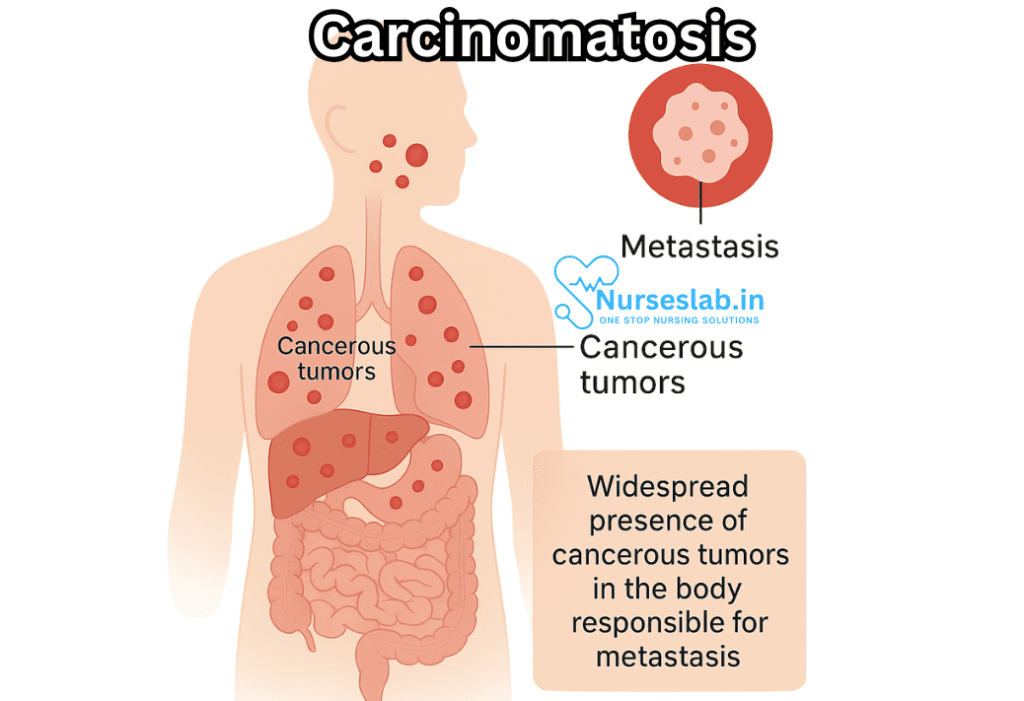
Carcinomatosis is a term used to describe the widespread dissemination of carcinoma cells throughout the body, typically within a specific body cavity or across multiple organ systems. Unlike localized cancers that remain confined to their tissue of origin, carcinomatosis refers to a scenario where malignant cells have migrated far beyond their initial site, seeding into distant tissues and surfaces. This often signals an advanced stage of disease, with significant implications for prognosis and management.
Pathology and Mechanism of Spread
Carcinomatosis is most commonly associated with epithelial malignancies—cancers arising from the lining of organs and surfaces—such as adenocarcinomas. The mechanisms underlying carcinomatosis involve complex interactions between the tumor, the host’s immune system, and the microenvironment of the affected tissues.
Peritoneal Carcinomatosis
One of the most frequently encountered forms is peritoneal carcinomatosis, wherein cancerous cells disseminate across the peritoneal cavity, the space within the abdomen that houses the digestive organs. Tumors originating from the gastrointestinal tract (such as colorectal or gastric cancers), ovarian cancer, and pancreatic cancer are among the most common sources.
The spread occurs when malignant cells detach from the primary tumor and travel, either by direct extension or via peritoneal fluid, to implant onto peritoneal surfaces. These implants can form nodules, plaques, or diffuse sheets, disrupting normal organ function and often causing symptoms such as ascites (fluid accumulation), pain, and bowel obstruction.
Pleural Carcinomatosis
Malignant cells can also disseminate within the pleural cavity—the space surrounding the lungs. This is frequently seen in lung cancers, breast cancers, and certain gastrointestinal cancers. Pleural carcinomatosis may lead to pleural effusion (fluid build-up), shortness of breath, chest pain, and cough.
Other Forms
Though less common, carcinomatosis can affect other serosal surfaces, such as the pericardium (around the heart), and even present as “meningeal carcinomatosis,” where cancer spreads within the protective membranes of the brain and spinal cord.
Clinical Presentation
The symptoms and signs of carcinomatosis depend on the organs and cavities involved, the amount and nature of tumor burden, and the underlying primary cancer. However, some common clinical features include:
- General malaise and fatigue: The extensive spread of cancer can lead to systemic symptoms and a profound sense of illness.
- Cachexia: Progressive weight loss and muscle wasting are often observed in advanced carcinomatosis.
- Abdominal distension and pain: Especially in peritoneal involvement, patients may report bloating, discomfort, or sharp pain due to fluid accumulation and tumor growth.
- Bowel obstruction: Tumor implants may obstruct the intestines, causing nausea, vomiting, constipation, or inability to pass gas.
- Dyspnea and pleuritic pain: Pleural involvement can restrict lung expansion and cause breathing difficulties.
- Neurological deficits: In rare meningeal carcinomatosis, patients may experience headaches, confusion, weakness, or cranial nerve abnormalities.
Diagnosis
Diagnosing carcinomatosis requires a high index of suspicion, especially in individuals with known malignancies who develop new systemic or cavity-related symptoms.
Imaging Studies
- CT Scan and MRI: These imaging modalities can reveal characteristic findings such as peritoneal thickening, nodularity, and fluid collections. They are essential for evaluating the extent of spread.
- Ultrasound: Useful particularly for detecting ascites or pleural effusions and guiding biopsies.
- PET Scan: Can highlight areas of metabolic activity, pinpointing both primary and metastatic disease.
Laboratory Tests
Blood tests may reveal nonspecific findings such as anemia, elevated inflammatory markers, and abnormal liver or kidney function, depending on organ involvement.
Histopathological Confirmation
The definitive diagnosis of carcinomatosis is made by obtaining tissue or fluid samples (such as ascitic fluid or biopsy of a peritoneal nodule) and demonstrating malignant cells under microscopic examination. Immunohistochemical staining may help identify the tissue of origin.
Common Primary Tumors Associated With Carcinomatosis
- Ovarian Cancer: Notoriously spreads throughout the peritoneal cavity.
- Colorectal Cancer: Can seed the peritoneum, particularly in advanced stages.
- Gastric Cancer: Peritoneal carcinomatosis is a well-known complication.
- Pancreatic Cancer: May extend to the peritoneum and other serous surfaces.
- Breast Cancer: Especially the lobular subtype, can cause peritoneal and pleural involvement.
- Lung Cancer: Commonly associated with pleural carcinomatosis.
Prognosis
Carcinomatosis is generally a marker of advanced disease and is often associated with a poor prognosis. The extent of disease spread, the type of primary cancer, and the patient’s overall health all influence survival. For example, peritoneal carcinomatosis from ovarian cancer may respond better to therapy than that from pancreatic or gastric cancer, where survival is frequently measured in months.
Management Strategies
Treatment of carcinomatosis must be individualized, taking into account the patient’s symptoms, underlying cancer type, and overall goals of care.
Symptom Management
- Palliative care: Central to the management of carcinomatosis, aiming to improve quality of life by addressing pain, ascites, bowel obstruction, and other distressing symptoms.
- Drainage procedures: Therapeutic paracentesis (removal of fluid from the abdomen) or thoracentesis (from the chest) can relieve discomfort.
- Nutritional support: Addressing cachexia and maintaining strength.
Chemotherapy
Systemic chemotherapy may slow progression and shrink tumor burden. In select cases, “intraperitoneal chemotherapy” (direct administration into the abdominal cavity) offers additional benefit, especially in ovarian cancer.
Surgical Options
Aggressive surgical procedures such as cytoreductive surgery may be attempted to remove visible tumor deposits, particularly when followed by hyperthermic intraperitoneal chemotherapy (HIPEC). This approach may offer survival benefits in selected patients but is not suitable for all due to morbidity and patient selection criteria.
Targeted and Immunotherapies
Recent advances in oncology have led to the development of molecular targeted therapies and immunotherapies, which may offer new hope in treating some forms of carcinomatosis, especially when tumor-specific pathways are identified.
Supportive and Psychosocial Care
The diagnosis of carcinomatosis brings physical, emotional, and psychological challenges. Patients and families benefit from psychosocial support, counseling, and coordination of care among oncology, palliative, and other specialties. Advanced care planning and clear communication are essential.
Nursing Care of Patients with Carcinomatosis
Nursing care for patients with carcinomatosis must be holistic, compassionate, and tailored to address both physical and psychosocial needs, with the overarching goal of optimizing quality of life.
Assessment and Early Recognition
A thorough and ongoing assessment is the cornerstone of effective nursing care in carcinomatosis. Nurses should gather a comprehensive history and monitor for signs and symptoms, which may include:
- Abdominal distention and pain (especially in peritoneal carcinomatosis)
- Dyspnea, cough, or chest discomfort (pleural involvement)
- Ascites or pleural effusions
- Weight loss and cachexia
- Altered bowel or bladder habits
- Mental status changes (meningeal carcinomatosis)
- Fatigue and reduced mobility
- Nausea, vomiting, and loss of appetite
Continuous assessment should also include vital signs, fluid balance, pain levels, and psychological well-being. Early recognition of complications such as bowel obstruction, infections, or fluid overload is essential for prompt intervention.
Symptom Management
Symptom burden is often high in carcinomatosis, and effective management is central to nursing care.
Pain Management
Pain may stem from tumor infiltration, organ distention, or secondary complications. Nursing interventions include:
- Regular assessment using validated pain scales
- Administering prescribed analgesics (opioids, non-opioids, adjuvants)
- Monitoring for side effects and efficacy
- Non-pharmacological techniques such as guided imagery, relaxation, and repositioning
- Educating patients and families about pain control options
Ascites and Effusions
Ascites and pleural effusions are common and can cause discomfort and respiratory distress.
- Monitor for symptoms and measure abdominal girth or fluid drainage as appropriate
- Assist in paracentesis or thoracentesis procedures
- Evaluate for infection or leakage at drainage sites
- Educate patients on signs of fluid overload and when to seek help
Gastrointestinal Symptoms
Nausea, vomiting, constipation, or bowel obstruction may be present.
- Administer antiemetics and prokinetic agents as ordered
- Encourage small, frequent meals and assess dietary preferences
- Monitor bowel movements and prevent constipation with laxatives or stool softeners as prescribed
- Provide mouth care to combat dry mouth or taste changes
Respiratory Distress
Patients with pleural carcinomatosis may develop dyspnea or cough.
- Maintain upright or semi-Fowler’s position for comfort
- Administer supplemental oxygen as needed
- Encourage deep breathing and relaxation exercises
- Assess for signs of hypoxia or respiratory failure
Fatigue and Weakness
Fatigue is a prevalent and distressing symptom.
- Encourage balanced rest and activity periods
- Assist with activities of daily living to preserve energy
- Promote sleep hygiene and manage contributing factors such as anemia or electrolyte imbalances
Palliative and Supportive Care
Given the advanced nature of carcinomatosis, palliative care is integral. This extends beyond pain and symptom control to include psychosocial and spiritual support.
- Facilitate advance care planning and discussions about goals of care
- Provide emotional support to patients and their families
- Refer to counseling, chaplaincy, or social work services as needed
- Promote dignity, autonomy, and informed decision-making
- Support end-of-life care and hospice referral where appropriate
Nurses should be skilled in recognizing distress, grief, and anxiety, and provide a listening ear or appropriate referrals. Family meetings and regular communication help align care with patient wishes.
Nutrition and Hydration
Patients with carcinomatosis often suffer from poor appetite, cachexia, or difficulties with oral intake.
- Assess nutritional status regularly and consult dietitians as appropriate
- Encourage nutrient-rich, palatable foods and frequent small meals
- Manage symptoms that impede intake (e.g., nausea, dry mouth)
- Monitor for dehydration and discuss the risks and benefits of artificial hydration at the end of life
Prevention of Complications
Due to their fragile condition, patients are at risk for a range of complications:
- Infection: Monitor for fever, wound or drainage site infection, and sepsis. Implement infection control measures and educate families.
- Venous Thromboembolism (VTE): Encourage gentle mobility, utilize compression devices if appropriate, and monitor for signs of deep vein thrombosis or pulmonary embolism.
- Pressure Injuries: Reposition frequently, use pressure-relieving devices, and maintain skin integrity.
- Bowel Obstruction: Monitor for abdominal pain, vomiting, constipation, and distention. Report promptly to the medical team.
- Delirium: Assess mental status, minimize unnecessary medications, and provide a calm environment.
Patient and Family Education
Education is an ongoing process that empowers both patient and family to participate in care:
- Explain the nature and prognosis of carcinomatosis in clear, compassionate language
- Teach symptom monitoring and management strategies
- Discuss medication regimens, side effects, and the importance of adherence
- Provide information on available resources, support groups, and palliative care options
- Encourage questions and address concerns promptly to reduce anxiety
Communication and Advocacy
Nurses play a vital role in advocating for the needs, rights, and wishes of patients:
- Facilitate open, honest, and culturally sensitive communication between patients, families, and the healthcare team
- Advocate for interventions that align with the patient’s goals and values
- Ensure informed consent for procedures and treatments
- Assist in navigating complex healthcare systems and accessing appropriate services
Psychosocial and Spiritual Support
Facing a diagnosis of carcinomatosis is emotionally taxing for both patients and their loved ones:
- Acknowledge and validate feelings of fear, sadness, anger, or grief
- Support coping mechanisms and resilience
- Facilitate connections with spiritual or community resources as desired
- Offer bereavement support for families after the patient’s death
Interdisciplinary Collaboration
Effective care relies on a coordinated, interdisciplinary approach:
- Collaborate with physicians, pharmacists, dietitians, physical therapists, social workers, and palliative care teams
- Participate in care conferences and discharge planning meetings
- Maintain accurate and up-to-date documentation to ensure continuity of care
Ethical Considerations
Ethical dilemmas frequently arise in the care of patients with carcinomatosis, involving issues such as treatment limitations, withdrawal of care, and the right to refuse interventions. Nurses should:
- Respect patient autonomy and right to self-determination
- Facilitate advance directives and living wills
- Promote integrity and transparency in all interactions
- Seek guidance from ethics committees in complex cases
REFERENCES
- Batool A, Kasi A. Leptomeningeal Carcinomatosis. https://www.ncbi.nlm.nih.gov/books/NBK499862/. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
- Szadkowska MA, Pałucki J, Cieszanowski A. Diagnosis and treatment of peritoneal carcinomatosis – a comprehensive overview. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9995246/. Pol J Radiol. 2023 Feb;88:e89-e97.
- Desai JP, Moustarah F. Peritoneal Metastasis. https://www.ncbi.nlm.nih.gov/books/NBK541114/). In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
- Guo W, Chen H. 68. https://pubmed.ncbi.nlm.nih.gov/33048036/Ga FAPI PET/CT Imaging in Peritoneal Carcinomatosis. https://pubmed.ncbi.nlm.nih.gov/33048036/. Radiology. 2020 Dec;297(3):521. .
- Kajal D and Levine D. The Peritoneum. In: Rumack CM and Levine D, eds. Diagnostic Ultrasound. 6th ed. Philadelphia: Elsevier; 2024. 582-615.
- Coccolini F, Gheza F, Lotti M, Virzì S, Iusco D, Ghermandi C, Melotti R, Baiocchi G, Giulini SM, Ansaloni L, Catena F. Peritoneal carcinomatosis. World J Gastroenterol. 2013 Nov 7;19(41):6979-94. doi: 10.3748/wjg.v19.i41.6979. PMID: 24222942; PMCID: PMC3819534.
- Kumar A, Mantri SN. Lymphangitic Carcinomatosis. https://www.ncbi.nlm.nih.gov/books/NBK560921/. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
- McMullen JRW, Selleck M, Wall NR, Senthil M. Peritoneal carcinomatosis: limits of diagnosis and the case for liquid biopsy. Oncotarget. 2017 Jun 27;8(26):43481-43490. doi: 10.18632/oncotarget.16480. PMID: 28415645; PMCID: PMC5522163.
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





