Drowning from Within: The Silent Threat of Cardiogenic Pulmonary Edema
Introduction
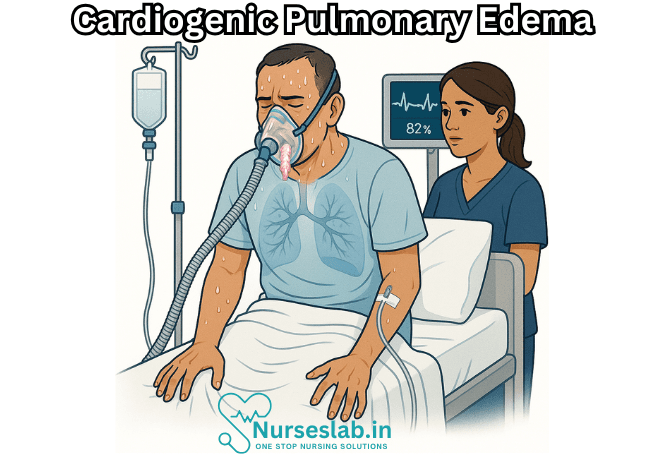
Cardiogenic pulmonary edema is a serious and potentially life-threatening condition characterized by the accumulation of fluid in the lungs due to elevated pressure in the pulmonary capillaries, most commonly resulting from cardiac dysfunction. This medical emergency is frequently associated with acute decompensated heart failure and requires prompt recognition and treatment. Understanding its underlying mechanisms, clinical presentations, and management is crucial for healthcare professionals and caregivers alike.
Pathophysiology
The fundamental cause of cardiogenic pulmonary edema is an increase in hydrostatic pressure within the pulmonary circulation, typically secondary to left ventricular failure. When the left ventricle is unable to effectively pump blood forward, pressure backs up into the left atrium and subsequently into the pulmonary veins and capillaries. As the hydrostatic pressure surpasses oncotic pressure, fluid seeps out of the capillaries into the interstitial space and, eventually, the alveoli.
Several cardiac conditions may precipitate this event:
- Acute Myocardial Infarction: Damage to the heart muscle impairs ventricular contractility, leading to failure.
- Chronic Heart Failure: Progressive weakening of the ventricular muscles over time.
- Severe Hypertension: Sudden increases in systemic blood pressure can overwhelm left ventricular function.
- Valvular Heart Disease: Disorders such as mitral stenosis or regurgitation result in abnormal pressure dynamics.
- Arrhythmias: Rapid or irregular heartbeats may compromise cardiac output.
The consequence is a cascade of events that disrupts gas exchange, leading to hypoxemia and respiratory distress. In severe cases, the accumulation of fluid within the alveolar space may result in respiratory failure.
Clinical Manifestations
Cardiogenic pulmonary edema presents with a spectrum of signs and symptoms, often developing suddenly and progressing rapidly. The classic presentation includes:
- Dyspnea: Shortness of breath, initially on exertion and later at rest.
- Orthopnea: Difficulty breathing when lying flat, prompting patients to sleep propped up.
- Paroxysmal Nocturnal Dyspnea: Sudden episodes of breathlessness that awaken patients from sleep.
- Tachypnea: Increased respiratory rate.
- Cough: Often productive of frothy, sometimes blood-tinged sputum due to capillary rupture.
- Crackles: Auscultation reveals inspiratory crackles or rales, particularly at the lung bases.
- Peripheral Cyanosis: Bluish coloration of lips and extremities due to hypoxia.
- Diaphoresis: Excessive sweating, reflecting sympathetic activation.
In severe cases, patients may experience distress, agitation, confusion, or even loss of consciousness. The rapid accumulation of fluid can make the situation dire within minutes to hours.
Diagnostic Evaluation
Accurate and timely diagnosis of cardiogenic pulmonary edema is essential for initiating appropriate therapy. The evaluation typically involves:
Clinical Assessment
A thorough history and physical examination provide key clues: prior history of heart disease, hypertension, or valvular problems; recent onset of respiratory symptoms; and findings such as elevated jugular venous pressure, peripheral edema, and S3 heart sound.
Laboratory Studies
- B-type Natriuretic Peptide (BNP) or NT-proBNP: Elevated levels suggest cardiac origin of dyspnea.
- Cardiac Troponins: To assess for acute myocardial injury.
- Renal Function Tests: To gauge end-organ perfusion and potential complications.
Imaging
- Chest X-ray: Reveals bilateral alveolar infiltrates, enlarged cardiac silhouette, and vascular redistribution.
- Echocardiography: Assesses ventricular function, valve abnormalities, and estimates pulmonary pressures.
Electrocardiography (ECG)
Identifies arrhythmias, ischemic changes, or evidence of previous myocardial infarction.
Differential Diagnosis
While cardiogenic pulmonary edema is primarily due to cardiac causes, distinguishing it from non-cardiogenic pulmonary edema (such as acute respiratory distress syndrome, ARDS) is vital. Non-cardiogenic etiologies involve increased capillary permeability rather than hydrostatic pressure.
Key differentiating features include:
- History of cardiac disease in cardiogenic cases.
- Absence of left heart failure in non-cardiogenic cases.
- BNP levels tend to be higher in cardiogenic edema.
Management Strategies
Treatment of cardiogenic pulmonary edema is based on urgent stabilization and correction of underlying cardiac dysfunction.
Immediate Interventions
- Oxygen Therapy: High-flow oxygen or mechanical ventilation may be necessary to combat hypoxemia.
- Positioning: Sitting the patient upright reduces venous return and pulmonary congestion.
- Continuous Monitoring: Cardiac rhythm, oxygen saturation, and vital signs.
Pharmacological Therapy
- Diuretics: Intravenous loop diuretics (such as furosemide) to reduce fluid overload.
- Vasodilators: Medications such as nitroglycerin or sodium nitroprusside lower cardiac preload and afterload.
- Inotropes: For cases of severe ventricular dysfunction, agents like dobutamine may improve contractility.
- Morphine: Occasionally used to decrease anxiety and venous return, though its use is now more restricted.
- Antihypertensives: If severe hypertension is present, medications to lower blood pressure are indicated.
Treating the Underlying Cause
Identifying and addressing the precipitating cardiac event is crucial. This may involve:
- Revascularization for acute myocardial infarction (such as percutaneous coronary intervention).
- Correction of valvular lesions through surgery or percutaneous interventions.
- Management of arrhythmias with antiarrhythmic drugs or electrical cardioversion.
Advanced Therapies
In refractory cases, advanced treatments such as mechanical circulatory support (intra-aortic balloon pump, ventricular assist devices), or even extracorporeal membrane oxygenation (ECMO), may be considered. These are reserved for patients with life-threatening cardiac failure not responsive to standard therapy.
Complications
Failure to promptly manage cardiogenic pulmonary edema can result in dire consequences:
- Acute respiratory failure requiring mechanical ventilation.
- Multi-organ dysfunction due to hypoperfusion.
- Cardiac arrest.
- Death.
Prognosis
The prognosis for cardiogenic pulmonary edema depends largely on the underlying cause, severity of cardiac dysfunction, and speed of intervention. With prompt and appropriate treatment, many patients recover fully; however, recurrent episodes may signal advanced heart failure and carry a poorer long-term outlook.
In chronic settings, ongoing management with optimized heart failure therapy, lifestyle modifications, and regular follow-up is vital to reduce recurrence and improve quality of life.
Prevention
Prevention hinges on effective control of cardiac risk factors:
- Optimal management of hypertension, diabetes, and coronary artery disease.
- Adherence to prescribed heart failure medications.
- Dietary modifications to limit salt and fluid intake.
- Regular exercise and weight management.
- Avoidance of precipitants such as excessive alcohol consumption or medication noncompliance.
Nursing Care of Patients with Cardiogenic Pulmonary Edema
Nurses play a pivotal role in the multidisciplinary management of patients experiencing cardiogenic pulmonary edema, providing both acute and ongoing care to optimize patient outcomes.
Assessment and Monitoring
Timely assessment and continuous monitoring are essential for early detection and management of clinical deterioration.
Initial Assessment
- Assess airway, breathing, and circulation (ABCs).
- Monitor respiratory rate, depth, and pattern.
- Check oxygen saturation (SpO₂) using pulse oximetry.
- Evaluate level of consciousness and mental status.
- Monitor heart rate, blood pressure, and rhythm (via ECG).
- Obtain baseline weight for fluid balance monitoring.
- Monitor fluid intake and output strictly.
Ongoing Monitoring
- Frequent reassessment of respiratory and cardiac status.
- Continuous ECG and SpO₂ monitoring in acute phase.
- Monitor for signs of worsening hypoxemia or shock.
- Assess for response to interventions (clinical and laboratory data).
Nursing Interventions
The priorities in nursing care for cardiogenic pulmonary edema are airway management, optimizing oxygenation, reducing cardiac workload, managing fluid volume, and providing patient comfort and psychological support.
Airway Management and Oxygenation
- Position the patient in high Fowler’s position to facilitate lung expansion and reduce venous return to the heart.
- Administer supplemental oxygen as prescribed to maintain SpO₂ above 94%—this may involve nasal cannula, face mask, or non-rebreather mask in severe cases.
- Prepare for and assist with advanced airway management (e.g., continuous positive airway pressure [CPAP], bilevel positive airway pressure [BiPAP], or intubation and mechanical ventilation) if indicated and as ordered.
- Suction airway, if necessary, to clear secretions and prevent aspiration.
Medication Administration and Monitoring
- Administer diuretics (e.g., furosemide) to reduce fluid overload and pulmonary congestion as ordered.
- Administer vasodilators (e.g., nitroglycerin) and/or inotropes (e.g., dobutamine) as prescribed for blood pressure and cardiac contractility management.
- Monitor for side effects of medications (hypotension, electrolyte imbalances, arrhythmias).
- Ensure IV access is patent and all infusions are correctly titrated.
Fluid Management
- Strictly measure and record intake and output.
- Monitor for signs of fluid overload: increasing edema, jugular venous distension, weight gain.
- Adjust fluid and sodium intake as per physician’s orders.
- Monitor laboratory values for electrolytes, renal function, and cardiac enzymes.
Cardiac Monitoring and Support
- Continuous ECG monitoring to detect arrhythmias.
- Monitor blood pressure at regular intervals.
- Report any changes in rhythm, hypotension, or signs of shock immediately.
- Assist with echocardiograms or other diagnostic procedures as needed.
Patient Comfort and Psychological Support
- Reassure and provide emotional support to alleviate anxiety and fear.
- Maintain a calm, quiet environment to reduce stress and cardiac workload.
- Educate the patient and family about the disease process and care plan.
- Encourage family presence and involvement in care when appropriate.
- Address pain management as prescribed, especially if the patient has concurrent ischemic heart disease.
Patient and Family Education
Education is crucial in preventing recurrence and promoting self-care.
- Instruct the patient and family about the signs and symptoms of worsening heart failure or pulmonary edema, such as increasing shortness of breath, cough, weight gain, or swelling.
- Educate about the importance of medication adherence, dietary restrictions (particularly sodium and fluid), and regular follow-up appointments.
- Provide written and verbal instructions tailored to the patient’s comprehension level.
- Teach about lifestyle modifications, including smoking cessation, moderation of alcohol intake, and appropriate levels of physical activity.
- Encourage weight monitoring daily and report significant changes to healthcare providers promptly.
Complications and Nursing Actions
Cardiogenic pulmonary edema can rapidly deteriorate and lead to complications such as severe hypoxemia, respiratory failure, arrhythmias, cardiogenic shock, multi-organ failure, and death.
- Be vigilant for signs of worsening hypoxemia: restlessness, confusion, cyanosis, declining SpO₂.
- Monitor for chest pain or ECG changes indicating acute myocardial infarction.
- Report any urine output less than 30 mL/hr.
- Prepare for advanced resuscitative measures as necessary.
Interdisciplinary Collaboration
Optimal outcomes are achieved through teamwork. Nurses should coordinate with:
- Physicians and cardiologists for medication and intervention management.
- Respiratory therapists for advanced airway and ventilatory support.
- Pharmacists for safe medication administration and monitoring.
- Physical therapists for early mobilization as the patient’s condition allows.
- Dietitians for nutrition planning and sodium/fluid restriction.
Discharge Planning and Follow-Up
Early and thorough discharge planning can reduce the risk of readmission.
- Assess patient and family readiness for discharge and understanding of care instructions.
- Coordinate home care services if required (e.g., visiting nurse for medication monitoring, wound care if applicable, or weight monitoring).
- Arrange for timely follow-up with primary care provider or cardiologist.
- Provide emergency contact information and instructions on when to seek immediate care.
REFERENCES
- Brakenhielm E, González A, Díez J. Role of Cardiac Lymphatics in Myocardial Edema and Fibrosis: JACC Review Topic of the Week. https://pubmed.ncbi.nlm.nih.gov/32762908/. J Am Coll Cardiol. 2020 Aug 11;76(6):735-744.
- CDC. Heart Failure. https://www.cdc.gov/heartdisease/heart_failure.htm.
- Hu D, Li L, Li S, et al. Lymphatic system identification, pathophysiology and therapy in the cardiovascular diseases. https://pubmed.ncbi.nlm.nih.gov/31181226/. J Mol Cell Cardiol. 2019 Aug;133:99-111.
- Iqbal MA, Gupta M. Cardiogenic Pulmonary Edema. [Updated 2023 Apr 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK544260/
- Merck Manual Consumer Version. Heart Failure. https://www.merckmanuals.com/home/heart-and-blood-vessel-disorders/heart-failure/heart-failure-hf?query=renal%20edema.
- Merck Manual Professional Version. Edema. https://www.merckmanuals.com/professional/cardiovascular-disorders/symptoms-of-cardiovascular-disorders/edema#v1144211.
- Nielsen NR, Rangarajan KV, Mao L, et al. A murine model of increased coronary sinus pressure induces myocardial edema with cardiac lymphatic dilation and fibrosis. https://pubmed.ncbi.nlm.nih.gov/32142379/. Am J Physiol Heart Circ Physiol. 2020 Apr 1;318(4):H895-H907.
- StatPearls. Cardiogenic Pulmonary Edema. https://www.ncbi.nlm.nih.gov/books/NBK544260/.
- Zanza C, Saglietti F, Tesauro M, Longhitano Y, Savioli G, Balzanelli MG, Romenskaya T, Cofone L, Pindinello I, Racca G, Racca F. Cardiogenic Pulmonary Edema in Emergency Medicine. Adv Respir Med. 2023 Oct 13;91(5):445-463. doi: 10.3390/arm91050034. PMID: 37887077; PMCID: PMC10604083.
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





