Carotid body tumors are growths in the blood vessels near your carotid arteries. These growths are typically benign (noncancerous), but may affect nearby nerves and blood vessels if they grow large. Healthcare providers often use surgery and embolization to treat carotid body tumors.
Introduction
Carotid body tumours (CBTs), also known as paragangliomas of the carotid body, represent a rare but clinically significant group of neoplasms arising from the paraganglionic tissue located at the bifurcation of the common carotid artery. Although traditionally considered benign, these tumours pose considerable diagnostic and therapeutic challenges due to their intricate anatomy, potential for local invasion, and rare instances of malignancy. The management of CBTs requires multidisciplinary expertise spanning otolaryngology, vascular surgery, radiology, and oncology.
Epidemiology of Carotid Body Tumors
Incidence and Prevalence
CBTs are rare neoplasms, with an estimated incidence ranging from 1 in 30,000 to 1 in 1,000,000 individuals annually. They account for approximately 60% of all head and neck paragangliomas. The true prevalence may be underestimated due to asymptomatic cases and diagnostic challenges.
Demographics
CBTs can occur at any age but are most commonly diagnosed between the third and sixth decades of life. There is a slight female predominance reported in some studies, though this is not universally observed. Bilateral tumours are noted in 5-10% of cases, particularly in hereditary syndromes.
Geographical Distribution
Higher prevalence rates are observed in populations residing at high altitudes, such as the Andean region, possibly due to chronic hypoxic stimulation. In India, CBTs remain rare but are increasingly recognised due to improved imaging and awareness.
Etiology and Risk Factors
Genetic Contributors
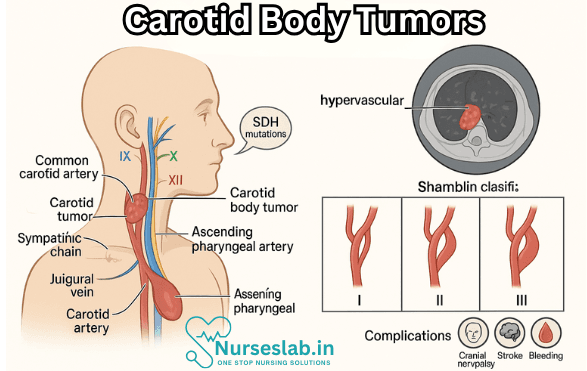
A subset of CBTs arises in the context of hereditary paraganglioma syndromes, most notably those involving mutations in the succinate dehydrogenase (SDH) gene complex (SDHB, SDHC, SDHD). Familial cases often present with bilateral or multiple tumours and carry a higher risk of malignancy. Genetic counselling and testing are recommended for patients with a family history or multifocal disease.
Environmental Factors
Chronic hypoxia, as seen in individuals living at high altitudes or with chronic lung disease, is implicated in the pathogenesis of CBTs. The carotid body undergoes hypertrophy and hyperplasia in response to sustained hypoxic conditions, potentially predisposing to neoplastic transformation.
Other Risk Factors
Additional factors include advancing age, female gender, and exposure to certain environmental toxins, although evidence remains limited and inconclusive.
Pathophysiology
Tumour Development
CBTs originate from paraganglionic chief cells, which possess neuroendocrine properties. Tumourigenesis is believed to result from a combination of genetic mutations, chronic hypoxic stimulation, and aberrant cellular proliferation. Mutations in SDH genes disrupt mitochondrial function, leading to accumulation of succinate and activation of hypoxia-inducible pathways that drive neoplastic growth.
Progression and Biological Behaviour
Most CBTs are slow-growing and benign; however, approximately 6-12% display malignant behaviour, characterised by local invasion and distant metastasis. Malignancy is defined by the presence of metastases rather than histological features alone. The potential for vascular invasion and cranial nerve involvement underscores the importance of early diagnosis and intervention.
Clinical Presentation
Symptoms and Signs
CBTs typically present as a painless, slowly enlarging mass in the lateral neck, at the level of the carotid bifurcation. The classical finding is a firm, mobile mass that moves horizontally but not vertically, due to its fixation between the carotid arteries.
- Local Symptoms: Neck swelling, pulsatile mass, bruit on auscultation.
- Neurological Symptoms: Cranial nerve palsies (IX, X, XI, XII) manifesting as dysphagia, hoarseness, shoulder weakness, or tongue deviation.
- Vascular Symptoms: Rarely, syncope due to carotid sinus compression, or symptoms of carotid artery occlusion.
- Systemic Symptoms: Most CBTs are non-functional; however, a small subset may secrete catecholamines, leading to hypertension, palpitations, and headaches.
Physical Examination
On examination, the mass is typically located at the anterior border of the sternocleidomastoid muscle, is non-tender, and may transmit pulsations. Cranial nerve deficits should be specifically assessed.
Diagnostic Evaluation
Imaging Modalities
- Ultrasound: Useful for initial assessment, revealing a well-defined, highly vascularised mass at the carotid bifurcation.
- Computed Tomography (CT): Provides anatomical detail, demonstrates splaying of the internal and external carotid arteries (“lyre sign”), and assesses local invasion.
- Magnetic Resonance Imaging (MRI): Superior soft tissue contrast, shows characteristic “salt and pepper” appearance due to flow voids and haemorrhage. MR angiography delineates vascular anatomy and feeding vessels.
- Digital Subtraction Angiography (DSA): Gold standard for vascular mapping, used for preoperative planning and embolisation.
Laboratory Investigations
Biochemical testing for catecholamines and their metabolites (e.g., plasma metanephrines) is indicated in cases with suspected functional tumours or familial syndromes.
Histopathological Examination
Definitive diagnosis requires histological evaluation, typically performed post-excision. CBTs display nests (“zellballen”) of chief cells surrounded by sustentacular cells, with immunohistochemical staining for chromogranin, synaptophysin, and S-100 protein.
Differential Diagnosis
The differential diagnosis of a neck mass at the carotid bifurcation includes:
- Jugular or vagal paraganglioma
- Branchial cleft cyst
- Thyroid nodule or goitre
- Lymphadenopathy (reactive or neoplastic)
- Carotid artery aneurysm
- Metastatic lymph node
Distinction from these entities relies on clinical features, imaging characteristics, and histopathology.
Management Strategies
Surgical Approaches
Surgical excision remains the mainstay of treatment for most CBTs. The decision to operate depends on tumour size, location, growth rate, patient age, comorbidities, and presence of symptoms. Preoperative embolisation may reduce intraoperative blood loss and facilitate resection.
- Resection Techniques: Tumours are classified by Shamblin’s criteria (I-III) based on size and vascular involvement:
- Type I: Small, easily resectable without vessel involvement
- Type II: Larger, partially encasing vessels
- Type III: Large, intimately adherent or encasing carotid arteries, requiring vessel reconstruction
- Cranial Nerve Preservation: Meticulous dissection is essential to preserve cranial nerves and minimise morbidity.
- Vascular Control: May require temporary or permanent carotid artery ligation or reconstruction in advanced cases.
Radiological Management
Radiotherapy is considered for unresectable tumours, high surgical risk patients, or recurrent disease. Modern stereotactic radiotherapy offers improved local control with reduced morbidity.
Medical Management
Pharmacological therapy is reserved for functional tumours secreting catecholamines, with alpha- and beta-blockade administered preoperatively. Molecular targeted therapies are under investigation but not yet standard practice.
Observation
Active surveillance may be appropriate for small, asymptomatic, slow-growing tumours in elderly or high-risk patients, with regular imaging and clinical assessment.
Complications and Prognosis
Complications
- Surgical: Cranial nerve injury, stroke, haemorrhage, carotid artery damage, infection.
- Non-Surgical: Tumour recurrence, progression, malignant transformation, local invasion.
Prognosis and Outcomes
The prognosis for CBTs is generally favourable, with five-year survival rates exceeding 90% for benign tumours. Malignant CBTs carry a poorer prognosis, with increased risk of recurrence and metastasis. Long-term follow-up is essential due to the potential for late recurrence.
Factors associated with adverse outcomes include large tumour size, bilateral or multifocal disease, SDHB mutations, incomplete resection, and presence of malignancy.
Nursing Care of Patients with Carotid Body Tumours
Nursing care plays a vital role in the multidisciplinary management of patients with carotid body tumours, from initial assessment and diagnosis to perioperative care and long-term follow-up.
Nursing Assessment
A thorough nursing assessment lays the foundation for effective care. Key components include:
- Health History: Elicit information regarding the duration and progression of neck mass, presence of pain, respiratory difficulties, voice changes, swallowing difficulties, or cranial nerve deficits. Investigate family history of paragangliomas or related syndromes.
- Physical Examination: Assess for palpable neck masses, tracheal deviation, bruit over the mass, and signs of nerve involvement (e.g., tongue deviation, hoarseness, shoulder droop).
- Psychosocial Assessment: Evaluate patient and family anxiety, understanding of diagnosis, and coping mechanisms.
- Preoperative Evaluation: Determine baseline neurological status, airway patency, and cardiovascular stability, as these tumours may rarely secrete catecholamines, leading to hypertension or other systemic effects.
Nursing Diagnosis
Nursing diagnoses for patients with carotid body tumours may include:
- Ineffective airway clearance related to tumour compression.
- Risk for impaired tissue perfusion (cerebral or peripheral) related to vascular compromise during surgery.
- Acute pain related to tumour or surgical intervention.
- Risk for infection related to surgical intervention.
- Impaired verbal communication related to cranial nerve involvement.
- Anxiety and fear related to diagnosis, treatment, and potential complications.
Preoperative Nursing Care
Preparation for surgery is crucial, as carotid body tumours are often removed surgically due to risks of growth and local invasion. Preoperative nursing care involves:
- Patient Education: Explain the surgical procedure, expected outcomes, potential risks (e.g., stroke, nerve injury, hemorrhage), and postoperative expectations. Use visual aids and encourage questions to ensure understanding.
- Preoperative Testing: Assist with scheduling and preparation for imaging studies (CT, MRI, angiography), blood tests, ECG, and other relevant investigations.
- Optimizing Medical Status: Collaborate with the healthcare team to manage hypertension or other comorbidities. Monitor for and address any signs of catecholamine excess if the tumour is functional.
- Informed Consent: Verify that the patient (or legal guardian) has provided informed consent after understanding the risks and benefits.
- Psychological Support: Provide reassurance, address fears, and offer resources for counseling or support groups if needed.
Intraoperative Nursing Care
Intraoperative nursing care is typically the responsibility of perioperative nursing staff and includes:
- Patient Safety: Ensure patient identification, correct site and side, and adherence to universal protocols.
- Monitoring: Continuous monitoring of vital signs, neurological status, and cardiac function. Be alert for sudden changes, especially hypertension, hypotension, or arrhythmias.
- Assisting the Surgical Team: Prepare equipment for vascular control, including shunts, clamps, and suction. Have blood products available in case of hemorrhage.
- Documentation: Maintain accurate records of intraoperative events, medications administered, and responses to interventions.
Postoperative Nursing Care
Postoperative care is critical to minimize complications and promote recovery. Key nursing interventions include:
Airway and Breathing
- Monitor for airway obstruction due to swelling or hematoma formation. Be vigilant for stridor, respiratory distress, or decreased oxygen saturation.
- Maintain head elevation at 30-45 degrees to reduce neck swelling and support airway patency.
- Encourage gentle coughing and deep breathing exercises to prevent atelectasis.
Circulation
- Monitor blood pressure, heart rate, and neurological status closely, as manipulation of the carotid artery may affect cerebral perfusion or precipitate stroke.
- Assess for signs of bleeding or hematoma at the surgical site, which may indicate vascular injury.
Pain Management
- Administer prescribed analgesics and assess pain levels frequently. Use both pharmacologic and non-pharmacologic methods (e.g., cold compress, relaxation techniques).
- Monitor for complications related to opioid use, such as respiratory depression or constipation, and intervene as needed.
Neurological Assessment
- Conduct frequent neurological checks, including level of consciousness, cranial nerve function, motor and sensory assessments.
- Report any new deficits, such as facial droop, limb weakness, dysarthria, or altered mental status, immediately to the medical team.
Infection Control
- Maintain aseptic technique during dressing changes.
- Monitor for signs of infection at the incision site: redness, swelling, warmth, purulent discharge, or fever.
- Educate the patient and family on wound care and signs of infection to watch for after discharge.
Management of Nerve Injury
- Assess for hoarseness, difficulty swallowing, shoulder weakness, or tongue deviation, which may indicate damage to cranial nerves (IX, X, XI, or XII).
- Collaborate with speech and occupational therapists for rehabilitation if nerve injury is present.
Patient Education and Discharge Planning
- Teach the patient and caregivers about medication regimens, wound care, activity restrictions, and follow-up appointments.
- Provide written instructions tailored to the patient’s literacy level and language needs.
- Educate about the importance of reporting neurological changes, signs of infection, or bleeding.
- Encourage participation in support groups or counseling if coping difficulties arise.
Long-Term Nursing Management
Carotid body tumours may recur or, in rare cases, metastasize. Long-term follow-up is essential to monitor for recurrence and address late complications. Nursing roles in long-term management include:
- Follow-Up Care: Reinforce the importance of regular clinic visits, imaging studies, and laboratory tests as scheduled by the healthcare provider.
- Survivorship and Quality of Life: Address persistent pain, nerve deficits, or psychological impacts that can affect daily living. Coordinate referrals to social work, physical therapy, and mental health services as needed.
- Genetic Counseling: For patients with familial or multiple paragangliomas, provide information on genetic screening and counseling for the patient and at-risk relatives.
- Health Promotion: Encourage a healthy lifestyle, including smoking cessation, balanced nutrition, and regular exercise, to optimize overall well-being.
Potential Complications and Nursing Interventions
Hemorrhage: Due to the highly vascular nature of the tumour, there is a significant risk of bleeding during and after surgery. Nurses should monitor for expanding neck hematoma, hypotension, tachycardia, or decreased hemoglobin, and be prepared to initiate emergency protocols.
Stroke: Manipulation of the carotid artery may dislodge plaque or cause thrombosis, leading to cerebral ischemia or stroke. Nurses should monitor for sudden neurological changes, including confusion, unilateral weakness, speech difficulties, or vision changes.
Cranial Nerve Injury: Damage to the nearby cranial nerves can result in swallowing difficulties, speech impairment, tongue deviation, and shoulder weakness. Early identification and referral to rehabilitation services can improve outcomes.
Infection: Strict adherence to aseptic technique and patient education can reduce the risk of surgical site infection.
REFERENCES
- Kakamad FH, Mustafa MN, Yasin SW. Carotid body tumor: characteristics and surgical outcome. J Cardiothorac Surg. 2024 Jul 31;19(1):473.
- Demir T, Uyar I, Demir HB, et al. Five-year Follow-up of a Patient With Bilateral Carotid Body Tumors After Unilateral Surgical Resection. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4188141/. Am J Case Rep. 2014;15:426-430. Published 2014 Oct 3.
- Gad A, Sayed A, Elwan H, et al. Carotid Body Tumors: A Review of 25 Years Experience in Diagnosis and Management of 56 Tumors. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4180692/. Ann Vasc Dis. 2014;7(3):292-299.
- Liu J, Mu H, Zhang W. Diagnosis and treatment of carotid body tumors. Am J Transl Res. 2021 Dec 15;13(12):14121-14132. PMID: 35035757; PMCID: PMC8748146.
- Gaillard F, Baba Y. Carotid body tumor. https://radiopaedia.org/articles/carotid-body-tumour?lang=us. Reference article, Radiopaedia.org.
- Wieneke JA, Smith A. Paraganglioma: Carotid Body Tumor. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2791477/. Head Neck Pathol. 2009;3(4):303-306.
- Nayak A, Parida PK, Aswathi KV, Preetam C, Pradhan P, Samal DK, Mohanty S, Adhya AK. Carotid Body Tumors: Institutional Experience of 10 Cases and a Review of Literature. Indian J Otolaryngol Head Neck Surg. 2023 Jun;75(2):1282-1289.
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles. s





