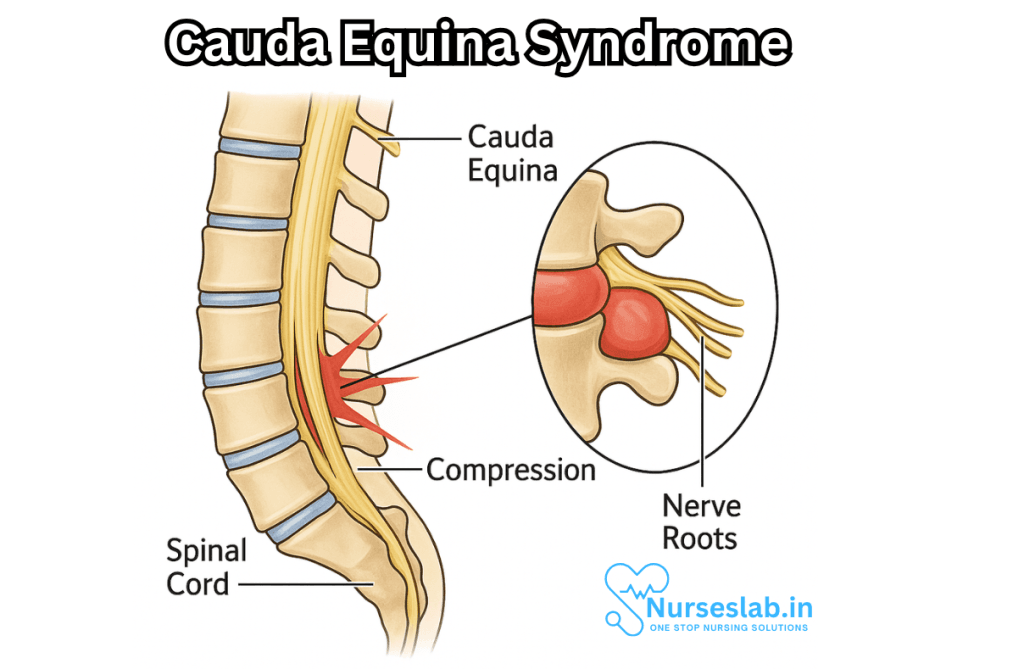
Cauda Equina Syndrome (CES) stands as one of the most significant neurological emergencies encountered in clinical practice, demanding swift recognition and intervention. Named after the “horse’s tail”—the literal translation of the Latin term “cauda equina”—this syndrome arises from compression of the bundle of nerve roots located at the lower end of the spinal cord. The cauda equina is responsible for sending and receiving messages to and from the lower limbs and pelvic organs. When these nerves are compressed, it can result in severe and sometimes irreversible neurological deficits.
What is the Cauda Equina?
The spinal cord, an extension of the central nervous system, ends roughly at the level of the first or second lumbar vertebra in adults. Below this point lies a fan of nerve roots, resembling a horse’s tail, known as the cauda equina. These nerves supply motor and sensory function to the legs, bladder, bowel, and sexual organs. The integrity of the cauda equina is thus vital for normal lower body functioning.
Cauda Equina Syndrome Defined
Cauda Equina Syndrome refers to a constellation of signs and symptoms resulting from compression, inflammation, or injury of the cauda equina nerve roots. The syndrome is rare but potentially devastating if untreated. It most commonly manifests as a combination of low back pain, sciatica, saddle anesthesia (loss of sensation in areas that would contact a saddle), bladder and/or bowel dysfunction, and varying degrees of lower limb weakness or sensory changes.
Causes of Cauda Equina Syndrome
CES can occur due to a variety of etiologies, many of which involve structural compromise of the spinal canal at the lumbar level. Major causes include:
- Herniated Lumbar Disc: The most prevalent cause, especially in adults aged 30-50, a herniated disc at the L4-L5 or L5-S1 level can impinge upon the cauda equina roots if the disc material protrudes centrally and severely.
- Spinal Stenosis: Degenerative narrowing of the spinal canal can lead to nerve compression, particularly in the elderly.
- Trauma: Fractures, dislocations, or other traumatic injuries to the lumbar spine can directly compress the cauda equina.
- Tumors or Neoplasms: Primary or metastatic tumors within the spinal canal may exert mass effect on the nerve roots.
- Infection: Epidural abscesses or other localized infections can cause swelling and compression.
- Spinal Hemorrhage: Bleeding within the spinal canal, though rare, can rapidly compromise neural structures.
- Iatrogenic Causes: Surgical complications or spinal anesthesia procedures may inadvertently damage the cauda equina.
Signs and Symptoms
CES can present in a classic or incomplete form, and not all patients will display all signs. However, several key features are highly suggestive:
- Severe low back pain: Often acute and associated with radicular pain radiating down one or both legs (sciatica).
- Saddle anesthesia: Numbness or altered sensation in the inner thighs, buttocks, and perineal region—the classic “saddle” distribution.
- Bladder dysfunction: Ranging from urinary retention (inability to pass urine), incontinence, or changes in the sensation of bladder fullness. Urinary retention is particularly concerning.
- Bowel dysfunction: Fecal incontinence or constipation due to loss of control over the anal sphincter and pelvic floor muscles.
- Sexual dysfunction: Erectile dysfunction or loss of genital sensation may be present.
- Motor weakness: Varying degrees of weakness in the lower limbs, sometimes leading to gait disturbances or difficulty standing up from a chair.
- Reflex changes: Diminished knee-jerk or ankle reflexes may be observed.
The presence of urinary retention or saddle anesthesia, especially in the context of recent severe back pain, should always raise suspicion for CES.
Diagnosis
Timely diagnosis is crucial in CES, as delays in treatment can result in permanent neurological damage. The diagnostic process involves:
- Clinical assessment: A focused history and thorough neurological examination are the starting points. Clinicians should specifically inquire about changes in bladder, bowel, or sexual function and test sensation in the perineal region.
- Imaging: The gold standard is Magnetic Resonance Imaging (MRI) of the lumbosacral spine, which can quickly and accurately identify the site and cause of nerve compression.
- Other investigations: In selected cases, additional tests such as computed tomography (CT) or myelography may be warranted, especially when MRI is unavailable or contraindicated.
- Bladder scanning: Measurement of post-void residual urine can help assess urinary retention.
Management and Treatment
Cauda Equina Syndrome is a surgical emergency. The principal goal of management is to relieve pressure on the cauda equina nerves as soon as possible to prevent or reverse neurological deficits.
- Emergency surgery: Decompressive surgery, most commonly via laminectomy and removal of the offending lesion (such as herniated disc material), should be performed ideally within 24 to 48 hours of symptom onset.
- Medical management: Pre-operative and post-operative treatment may include pain control, anti-inflammatory medications, and management of any infections if present (antibiotics for abscesses).
- Rehabilitation: Physical and occupational therapy are essential for maximizing recovery of function and independence.
- Bladder and bowel care: Catheterization, bowel management programs, and patient education are often required.
Timely intervention can make the difference between full recovery and lifelong disability.
Prognosis
Outcomes in CES largely depend on the rapidity of diagnosis and decompression. Patients treated within the first 24 to 48 hours have a significantly better chance of regaining bladder, bowel, and lower limb function. However, some deficits may persist, especially if initial symptoms included urinary retention or profound numbness.
Chronic complications can include persistent pain, sexual dysfunction, and functional limitations. Psychosocial support, counseling, and long-term rehabilitation may be necessary for optimal adjustment and quality of life.
Prevention and Awareness
While not all cases of CES are preventable—particularly those due to tumors or trauma—early recognition and prompt treatment of lumbar disc herniation and spinal infections can reduce risk. Raising awareness among healthcare professionals and the public about the urgency of certain “red flag” symptoms, such as sudden bladder or bowel dysfunction and saddle anesthesia, is key.
Living with Cauda Equina Syndrome
For those who live with the sequelae of CES, adaptation is both a physical and emotional journey. Support groups, rehabilitation, assistive devices, and comprehensive care plans can greatly enhance quality of life. Advocacy organizations and online communities provide resources, education, and a sense of solidarity for individuals and families affected by this rare condition.
Nursing Care of Patients with Cauda Equina Syndrome
Nursing professionals play a pivotal role in the multidisciplinary management of patients diagnosed with CES, from early recognition and acute intervention to rehabilitation and supportive care.
Nursing Assessment
The first step in nursing care is a thorough and prompt assessment, as early detection can significantly influence patient outcomes.
- Neurological Assessment: Monitor for changes in motor strength, sensory level, reflexes, and the presence of saddle anesthesia. Check for foot drop, muscle weakness, and gait disturbances.
- Pain Evaluation: Assess the character, intensity, and radiation of pain. Document any changes and effectiveness of pain management interventions.
- Bladder and Bowel Function: Inquire about and document any urinary retention, incontinence, changes in urinary stream, or loss of urge. Assess for bowel incontinence or constipation and monitor for abdominal distension.
- Skin Integrity: Evaluate the patient’s skin, particularly in insensate areas, for pressure injuries due to impaired sensation and mobility.
- Psychosocial Assessment: Assess the impact of symptoms on the patient’s emotional well-being, fears about prognosis, and support systems available.
Acute Nursing Interventions
Immediate nursing actions focus on patient safety, pain control, and preparation for potential surgical intervention.
- Immobilization and Safety: Maintain spinal alignment and educate patients on movement restrictions to prevent further nerve damage. Ensure the bed is in a low position and call bell is within reach.
- Pain Management: Administer prescribed analgesics, including opioids or non-steroidal anti-inflammatory drugs as ordered. Use non-pharmacological techniques such as positioning, cold packs, and relaxation strategies.
- Preoperative Preparation: If surgical decompression is anticipated, prepare the patient by ensuring informed consent is obtained, fasting protocols are followed, and preoperative checklists are completed. Establish intravenous access and monitor vital signs.
- Monitoring Neurological Status: Frequently monitor and document neurological function. Report any changes to the healthcare provider immediately.
- Bladder Management: Assess for urinary retention. Catheterization may be required if the patient is unable to void. Strictly monitor input and output, and watch for signs of urinary tract infection.
- Bowel Management: Prevent constipation by encouraging fiber intake (if allowed), adequate hydration, and administering stool softeners or laxatives as ordered.
Postoperative and Ongoing Nursing Care
After surgical intervention or in non-operative management, nursing care shifts to rehabilitation, complication prevention, and patient education.
Mobility and Rehabilitation
- Assist with gradual mobilization, following physiotherapy guidance to prevent deconditioning and encourage independence.
- Teach safe movement techniques to avoid falls and further injury.
- Use mobility aids as required and ensure the patient’s environment is obstacle-free.
Bladder and Bowel Care
- Intermittent Catheterization: Teach the patient and family intermittent self-catheterization if long-term bladder dysfunction persists.
- Bladder Training: Implement bladder training protocols, including timed voiding and double voiding techniques.
- Monitor for Autonomic Dysreflexia: Recognize and respond to signs of autonomic dysreflexia in patients with significant neurogenic bladder or bowel involvement.
- Bowel Regimen: Establish a consistent bowel regimen with diet modifications, scheduled toileting, and use of appropriate medications.
Skin Care and Pressure Injury Prevention
- Perform regular skin assessments and reposition the patient at least every two hours to prevent pressure injuries.
- Use specialized mattresses or cushions for those at high risk.
- Educate the patient and caregivers on the importance of daily skin checks, particularly in areas of reduced sensation.
Pain and Spasticity Management
- Continue to assess and treat pain, with a combination of pharmacological and non-pharmacological interventions.
- Monitor for and manage muscle spasms, which may require specific medications such as muscle relaxants.
Psychological and Emotional Support
- Recognize the psychological impact of CES, including anxiety, depression, and adjustment difficulties.
- Offer supportive listening, counseling referrals, and encourage involvement of family or support groups.
- Facilitate discussions around realistic goal setting and coping strategies.
Patient and Family Education
Education is a cornerstone in empowering patients and families to manage life after CES.
- Understanding the Condition: Explain CES, its causes, symptoms, and expected course, using language tailored to the patient’s level of understanding.
- Recognizing Red Flags: Teach early warning signs of deterioration, such as increased weakness, numbness, or changes in bladder/bowel habits, requiring immediate medical attention.
- Self-care Techniques: Instruct on appropriate bladder and bowel management, skin care, and mobility exercises.
- Medication Adherence: Emphasize the importance of taking medications as prescribed, being aware of potential side effects, and keeping follow-up appointments.
- Community Resources: Provide information about rehabilitation services, support groups, and assistive devices available in the community.
Complications and Preventive Strategies
Patients with CES are at risk for multiple complications, and vigilant nursing care is required to prevent or minimize these.
- Urinary Tract Infections: Prevention includes proper peri-care, sterile technique with catheterization, and adequate hydration.
- Bowel Obstruction or Impaction: Prevented by a regular bowel program, ample hydration, and dietary fiber.
- Pressure Ulcers: Avoided through frequent repositioning, skin checks, and pressure-relieving devices.
- Venous Thromboembolism (VTE): Preventive strategies include early mobilization, compression stockings, and pharmacological prophylaxis as ordered.
- Falls: Minimized by maintaining a safe environment, using assistive devices, and educating patients on fall prevention strategies.
Interdisciplinary Collaboration
Optimal outcomes for CES patients depend on effective collaboration among healthcare professionals. Nurses liaise with neurosurgeons, orthopedic surgeons, physiotherapists, occupational therapists, social workers, psychologists, and urologists. Through regular communication and care conferences, the team ensures comprehensive and coordinated care.
REFERENCES
- American Academy of Orthopaedic Surgeons. Cauda Equina Syndrome. https://orthoinfo.aaos.org/en/diseases–conditions/cauda-equina-syndrome/#:~:text=Cauda%20equina%20syndrome%20. Last reviewed 8/2022.
- Cauda equina syndrome. (2017).
https://www.cedars-sinai.edu/Patients/Health-Conditions/Cauda-Equina-Syndrome.aspx - American Academy of Orthopaedic Surgeons. Herniated Disk in the Lower Back.. https://orthoinfo.aaos.org/en/diseases–conditions/herniated-disk-in-the-lower-back/. Last reviewed 1/2022.
- American Association of Neurological Surgeons. Cauda Equina Syndrome. https://www.aans.org/en/Patients/Neurosurgical-Conditions-and-Treatments/Cauda-Equina-Syndrome. Last updated 12/3/2021.
- Rider LS, Marra EM. Cauda Equina and Conus Medullaris Syndromes. https://www.ncbi.nlm.nih.gov/books/NBK537200/. 2023 Aug 7. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
- Mayo Clinic Staff. (2016). Herniated disk:Symptoms and causes.
http://www.mayoclinic.org/diseases-conditions/herniated-disk/symptoms-causes/dxc-20271249
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





