Central serous retinopathy occurs when fluid builds up behind the retina in your eye. The fluid can cause your retina to detach, leading to vision problems. The condition is often associated with stress and corticosteroid use. Many cases resolve on their own, but you should seek medical attention to make sure vision problems aren’t permanent.
Introduction
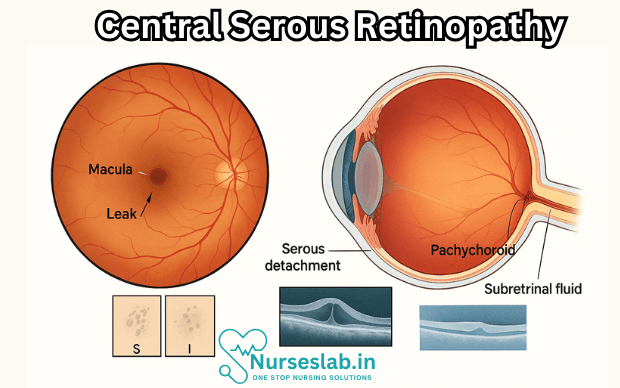
Central Serous Retinopathy (CSR), also known as Central Serous Chorioretinopathy (CSCR), is an ophthalmic condition characterized by the accumulation of serous fluid under the retina, leading to a localized detachment of the neurosensory retina at the macula. This disease primarily affects the central vision, which is critical for tasks such as reading, recognizing faces, and driving. While it is generally considered a self-limiting and benign condition, CSR can cause significant visual impairment, especially if recurrent or chronic.
Epidemiology
CSR predominantly affects adults between 20 and 50 years of age, with a higher prevalence in males compared to females (male-to-female ratio ranging from 6:1 to 10:1 in various studies). The condition is more commonly reported in individuals of Asian and Caucasian descent, though it can occur in all ethnic groups. Incidence rates vary, but estimates suggest an annual incidence of approximately 10 per 1,00,000 individuals. CSR is considered the fourth most common non-surgical retinopathy after diabetic retinopathy, branch retinal vein occlusion, and age-related macular degeneration.
Risk Factors
The aetiology of CSR is multifactorial, with several risk factors identified:
- Psychological Stress: High levels of stress and Type-A personality traits have been consistently linked to CSR. Stress may trigger hormonal changes that increase susceptibility.
- Glucocorticoid Use: Both endogenous (e.g., Cushing’s syndrome) and exogenous (oral, inhaled, topical, or injectable steroids) corticosteroids are associated with a higher risk of developing CSR.
- Pregnancy: CSR can occur during pregnancy, possibly due to hormonal fluctuations and increased endogenous corticosteroid levels.
- Hypertension: Systemic hypertension has been correlated with CSR, though the relationship is not completely understood.
- Obstructive Sleep Apnoea: Sleep disorders, particularly obstructive sleep apnoea, have been implicated as risk factors.
- Other Associations: Use of psychopharmacological medications, autoimmune disorders, Helicobacter pylori infection, and certain systemic illnesses have also been suggested as contributing factors.
Pathophysiology
The pathogenesis of CSR is complex and not fully elucidated. The prevailing theory involves dysfunction of the choroidal circulation and the retinal pigment epithelium (RPE):
- Choroidal Hyperpermeability: Increased permeability of the choroidal vessels leads to leakage of fluid through the RPE into the subretinal space.
- RPE Dysfunction: The RPE, which normally pumps fluid out of the subretinal space, becomes compromised and unable to maintain the fluid balance, resulting in serous detachment of the neurosensory retina.
- Hormonal Influences: Elevated levels of endogenous corticosteroids and catecholamines may exacerbate vascular permeability and RPE dysfunction.
- Sympathetic Overdrive: Chronic stress and related hormonal changes are believed to contribute to the disease process.
Clinical Presentation
CSR typically presents with the sudden onset of painless visual disturbances in one eye, though bilateral involvement is possible in up to 10% of cases. Key symptoms and signs include:
- Blurred or Dim Vision: Patients often notice a central or paracentral area of blurred vision, described as a “grey spot” or “smudge.”
- Metamorphopsia: Distortion of straight lines, making them appear wavy or bent.
- Micropsia: Objects may appear smaller than they are.
- Relative Scotoma: A partial loss of vision or a blind spot in the central visual field.
- Colour Vision Changes: Some patients report dullness or desaturation of colours.
- Reduced Contrast Sensitivity: Difficulty distinguishing between shades or contrasts.
On clinical examination, a shallow detachment of the neurosensory retina at the macula may be observed. The anterior segment is usually unremarkable, and intraocular pressure is within normal limits.
Diagnostic Workup
Accurate diagnosis of CSR is essential for appropriate management. The following investigations are commonly utilised:
- Optical Coherence Tomography (OCT): This non-invasive imaging modality provides cross-sectional images of the retina, clearly showing serous elevation of the neurosensory retina and subretinal fluid. It is also valuable for monitoring disease progression and response to therapy.
- Fundus Fluorescein Angiography (FFA): FFA is used to identify leakage points at the level of the RPE. The classic finding is a “smokestack” or “inkblot” pattern of fluorescein dye leakage.
- Indocyanine Green Angiography (ICGA): This imaging technique provides detailed visualisation of the choroidal circulation, highlighting areas of choroidal hyperpermeability.
- Autofluorescence Imaging: Useful for detecting RPE changes and chronicity of disease.
Other investigations may be performed to rule out alternative diagnoses, especially if atypical features are present.
Differential Diagnosis
The clinical features of CSR may resemble several other retinal diseases, necessitating a careful differential diagnosis. Conditions to consider include:
- Age-related Macular Degeneration (AMD)
- Polypoidal Choroidal Vasculopathy
- Choroidal Neovascularisation
- Retinal Detachment
- Vogt-Koyanagi-Harada Disease
- Uveitis
A detailed history, clinical examination, and appropriate imaging help distinguish CSR from these entities.
Classification
CSR can be classified based on duration and recurrence:
- Acute CSR: Symptoms last less than 3-4 months. Most cases resolve spontaneously within this period.
- Chronic CSR: Persistence of subretinal fluid or recurrent episodes lasting more than 3-4 months. Chronic CSR may cause permanent damage to the photoreceptors and the RPE, resulting in irreversible vision loss.
- Recurrent CSR: Multiple episodes of CSR separated by periods of complete or near-complete recovery.
Management
The management of CSR depends on the duration, severity, and impact on vision, as well as the presence of risk factors and the patient’s occupational demands.
Observation and Conservative Measures
Most cases of acute CSR resolve spontaneously within 3-4 months, with restoration of vision. Therefore, observation is the mainstay in the initial phase. Patients are advised to:
- Avoid or minimise psychological stress and adopt stress-reduction techniques (e.g., yoga, meditation, counselling).
- Discontinue corticosteroids where medically feasible, after consultation with the prescribing physician.
- Monitor vision at home using an Amsler grid.
Regular follow-up visits are scheduled to assess resolution of subretinal fluid and visual recovery.
Medical Therapy
Various medications have been tried in the management of CSR, especially in chronic or recurrent cases:
- Mineralocorticoid Receptor Antagonists: Drugs like eplerenone and spironolactone have shown promise in reducing subretinal fluid by modulating choroidal vascular permeability.
- Adrenergic Blockers: Beta-blockers and other agents targeting the sympathetic nervous system have been explored, with mixed results.
- Other Agents: Non-steroidal anti-inflammatory drugs, acetazolamide, and other agents have been trialled, though evidence is limited.
Laser and Photodynamic Therapy
Interventions are considered in chronic or visually significant CSR:
- Focal Laser Photocoagulation: Direct laser treatment to extrafoveal leakage points can accelerate resolution but is reserved for non-subfoveal lesions due to the risk of scarring and vision loss.
- Photodynamic Therapy (PDT): Verteporfin PDT is used for chronic or recurrent CSR, particularly when the leakage site is subfoveal. Low-dose or half-fluence protocols minimise collateral damage to the retina.
Other Modalities
Emerging treatments include subthreshold micropulse laser therapy, anti-VEGF injections, and novel pharmacological agents. However, these are generally reserved for refractory cases or clinical trials.
Prognosis
The prognosis of acute CSR is generally favourable, with most patients experiencing spontaneous resolution and recovery of near-normal vision within a few months. However:
- Up to 30-50% of patients may experience recurrence.
- Chronic or recurrent CSR can result in permanent damage to the photoreceptors and RPE, leading to lasting visual deficits.
- Some patients may report persistent subtle visual disturbances, such as reduced contrast sensitivity or metamorphopsia, even after resolution of fluid.
Timely diagnosis and appropriate management are crucial to minimise the risk of chronicity and vision loss.
Complications
Potential complications of CSR include:
- Permanent central vision loss, especially in chronic or recurrent cases.
- Development of secondary choroidal neovascularisation.
- Psychosocial impact due to visual impairment, particularly in individuals with high occupational or lifestyle demands.
Prevention
There are no definitive preventive strategies for CSR. However, mitigating modifiable risk factors may reduce the risk of occurrence or recurrence:
- Control systemic risk factors such as hypertension and sleep apnoea.
- Avoid unnecessary corticosteroid use.
- Manage psychological stress through relaxation techniques and lifestyle modification.
Nursing Care of a Patient with Central Serous Retinopathy
As vision is an essential aspect of daily living, CSR can be distressing for the patient, even though it frequently resolves spontaneously. Nurses play a pivotal role in the holistic care, education, support, and monitoring of patients with CSR.
Nursing Assessment
The nursing assessment for a patient with CSR should be comprehensive, focusing on physical, psychological, and social domains:
- Visual Assessment: Measure visual acuity using a Snellen chart or equivalent. Document the onset, duration, and progression of symptoms.
- Risk Factor Identification: Assess for history of corticosteroid use, recent stressors, hypertension, or autoimmune disease.
- Pain and Discomfort: While CSR is usually painless, assess for eye discomfort, photophobia, or other ocular symptoms.
- Psychological Status: Evaluate the patient’s anxiety, coping mechanisms, and impact on quality of life due to sudden vision changes.
- Medication Review: Document all medications, especially steroids or psychostimulants which may contribute to CSR.
Nursing Diagnoses
Based on the assessment, common nursing diagnoses may include:
- Disturbed Sensory Perception (Visual) related to retinal changes
- Anxiety related to sudden visual impairment and fear of vision loss
- Knowledge Deficit regarding CSR, its prognosis, and management
- Risk for Injury related to impaired vision
- Ineffective Coping related to stress and emotional response to CSR
Nursing Interventions
Nursing interventions focus on supporting the patient, preventing complications, and promoting visual recovery.
1. Visual Safety and Environment Modification
- Ensure adequate lighting in the patient’s environment to minimize accidents due to reduced vision.
- Remove tripping hazards and maintain clear pathways in the patient’s room or home.
- Encourage the use of assistive devices (e.g., magnifiers, large-print materials) as needed.
- Educate patient and family about compensatory strategies for activities of daily living.
2. Patient and Family Education
- Explain the nature of CSR, typical course, and generally favorable prognosis to reduce anxiety.
- Discuss the importance of regular ophthalmologic follow-up, as untreated or recurrent CSR may lead to permanent vision loss.
- Provide information about possible triggers (e.g., stress, steroids) and how to avoid them.
- Educate about the warning signs of complications, such as persistent or worsening vision loss, and when to seek medical attention.
3. Emotional and Psychological Support
- Offer reassurance and empathetic listening to address fear and anxiety related to sudden visual changes.
- Refer to counseling or support groups if the patient exhibits significant distress or difficulty coping.
- Encourage expression of feelings and provide guidance in using positive coping strategies, such as relaxation techniques or mindfulness.
4. Monitoring and Managing Medical Therapy
- Coordinate with the healthcare team to review the necessity of corticosteroid therapy or other contributory medications; advocate for discontinuation or reduction if appropriate.
- Monitor for adverse effects of therapies, such as photodynamic therapy or anti-VEGF injections, if employed for chronic or severe cases.
- Ensure adherence to prescribed treatment and follow-up schedules.
5. Lifestyle and Stress Management
- Educate about the role of stress in triggering or exacerbating CSR and discuss practical ways to manage stress (e.g., exercise, sleep hygiene, time management).
- Advise patients to avoid self-medication with corticosteroids or over-the-counter drugs linked to CSR.
- Encourage a healthy diet and address modifiable cardiovascular risk factors, such as hypertension or diabetes.
6. Coordination of Care
- Act as a liaison between the patient and ophthalmologist, primary physician, and other specialists as needed.
- Assist in scheduling appointments and ensuring continuity of care.
- Provide resources for visual rehabilitation if there is persistent visual impairment.
Evaluation of Outcomes
Nursing care is evaluated based on the patient’s adaptation to visual changes, the resolution of psychological distress, and the avoidance of complications:
- Patient demonstrates safe ambulation and performs daily activities with minimal risk of injury.
- Patient verbalizes understanding of CSR, its benign nature, and self-care measures.
- Anxiety levels are reduced, and the patient exhibits effective coping strategies.
- Patient attends follow-up visits and adheres to medical advice.
- No evidence of secondary complications, such as persistent subretinal fluid or chronic vision loss.
Discharge Planning and Long-Term Support
Discharge planning should involve:
- Clear instructions on follow-up appointments and indications for urgent medical review.
- Provision of contact information for community resources and low-vision support services.
- Education materials tailored to the patient’s visual needs (audio information, large print, or digital formats).
- Guidance for family members on how to assist with vision-related challenges and emotional support.
Special Considerations
- CSR can be recurrent—patients should be counseled about the possibility of relapse and be vigilant for symptoms.
- In occupational contexts, advice may be needed regarding driving and work-related visual demands during acute episodes.
- Chronic or atypical cases may require referral for advanced therapies or visual rehabilitation.
- Individualized care is essential; cultural, linguistic, and personal preferences should always be considered.
REFERENCES
- Getahun, H., Apte, R.S. Therapeutic interventions for chronic central serous chorioretinopathy: a comprehensive assessment of systematic reviews. Int J Retin Vitr 11, 34 (2025). https://doi.org/10.1186/s40942-025-00660-x
- American Academy of Ophthalmology. What is central serous chorioretinopathy. https://www.aao.org/eye-health/diseases/what-is-central-serous-retinopathy Last reviewed 10/9/2024.
- American Society of Retinal Specialists. Central serous chorioretinopathy. https://www.asrs.org/patients/retinal-diseases/21/central-serous-chorioretinopathy.
- Gupta A, Tripathy K. Central Serous Chorioretinopathy. [Updated 2023 Aug 25]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/sites/books/NBK558973/
- Feenstra HMA, van Dijk EHC, Cheung CMG, et al. Central serous chorioretinopathy: An evidence-based treatment guideline. https://pubmed.ncbi.nlm.nih.gov/38301969/. Prog Retin Eye Res. 2024 Jul;101:101236.
- Zhang, X., Lim, C.Z.F., Chhablani, J. et al. Central serous chorioretinopathy: updates in the pathogenesis, diagnosis and therapeutic strategies. Eye and Vis 10, 33 (2023). https://doi.org/10.1186/s40662-023-00349-y
- Fung AT, Yang Y, Kam AW. Central serous chorioretinopathy: A review. https://pubmed.ncbi.nlm.nih.gov/36597282/. Clin Exp Ophthalmol. 2023 Apr;51(3):243-270.
- Feenstra HMA, van Dijk EHC, Cheung CMG, Ohno-Matsui K, Lai TYY, Koizumi H, Central serous chorioretinopathy: An evidence-based treatment guideline. Prog Retin Eye Res. 2024 Jul;101:101236. doi: 10.1016/j.preteyeres.2024.101236. Epub 2024 Feb 1. PMID: 38301969.
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





