Cephalic disorders happen when something disrupts the development of a fetus’ central nervous system. This part of the nervous system includes the brain and spinal cord, both of which are critical parts of how your body works. These conditions range from minor to severe, and sometimes, their effects are deadly. Some are treatable, but this varies.
Introduction:
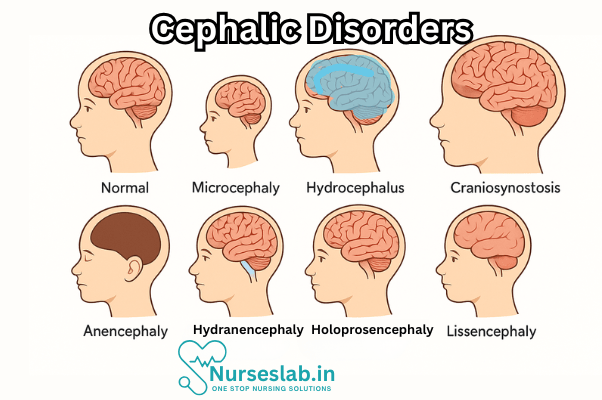
Cephalic disorders are a group of congenital conditions that affect the structure, development, and function of the head and brain. These disorders arise during the early stages of embryonic development, often resulting in significant neurological and physical impairments. Cephalic disorders encompass a diverse spectrum of conditions, ranging from mild cranial abnormalities to severe malformations incompatible with life.
The burden of cephalic disorders is considerable, with implications for affected individuals, families, and healthcare systems. In India and globally, ongoing research and advances in medical technology are reshaping the landscape of diagnosis and management.
Classification and Types of Cephalic Disorders
Cephalic disorders represent a heterogeneous group of conditions characterised by abnormalities in the formation and development of the head, skull, and brain. The major types include:
Anencephaly
Anencephaly is a severe neural tube defect in which major portions of the brain, skull, and scalp fail to develop. Infants with anencephaly are usually born without a forebrain and cerebrum, the regions responsible for cognition, sensation, and voluntary movement. This condition is universally fatal, with most affected infants dying shortly after birth.
Microcephaly
Microcephaly is defined by a significantly smaller head circumference compared to age- and sex-matched peers. It often reflects underlying brain underdevelopment or damage. Children with microcephaly may experience intellectual disability, developmental delays, seizures, and motor impairments. The severity of symptoms can vary widely.
Macrocephaly
Macrocephaly refers to an abnormally large head size, which may result from excess cerebrospinal fluid (hydrocephalus), brain overgrowth, or other structural anomalies. While some cases are benign, others may indicate underlying pathology requiring investigation.
Holoprosencephaly
Holoprosencephaly is a complex disorder where the embryonic forebrain fails to divide into two distinct hemispheres. This leads to varying degrees of craniofacial and neurological abnormalities, ranging from mild facial defects to profound brain malformation and functional impairment.
Craniosynostosis
Craniosynostosis involves the premature fusion of one or more cranial sutures, the fibrous joints between the bones of the skull. This restricts normal skull growth and can result in abnormal head shape, increased intracranial pressure, and neurological deficits if untreated.
Other Cephalic Disorders
- Hydranencephaly: Replacement of cerebral hemispheres by fluid-filled sacs.
- Porencephaly: Formation of cysts or cavities within the cerebral hemispheres.
- Encephalocele: Protrusion of brain tissue and membranes through openings in the skull.
- Schizencephaly: Abnormal slits or clefts in the cerebral hemispheres.
Each disorder presents unique challenges in terms of diagnosis, management, and prognosis, necessitating a tailored approach to care.
Causes and Risk Factors
The aetiology of cephalic disorders is multifactorial, involving genetic, environmental, and maternal factors. Understanding these contributors is essential for prevention and early intervention.
Genetic Factors
Many cephalic disorders are linked to genetic mutations or chromosomal abnormalities. For instance, holoprosencephaly is associated with mutations in genes such as SHH, ZIC2, and PTCH1. Craniosynostosis can occur as part of syndromic conditions like Crouzon or Apert syndrome, resulting from mutations in fibroblast growth factor receptor (FGFR) genes. Inheritance patterns vary, with some conditions being sporadic and others exhibiting autosomal dominant or recessive transmission.
Environmental Factors
Environmental exposures during pregnancy can significantly influence the risk of cephalic disorders. Teratogenic substances such as alcohol, certain medications (e.g., antiepileptic drugs), and toxins may disrupt normal neural development. Maternal exposure to pesticides, heavy metals, and radiation has also been implicated in increased risk.
Maternal Health
Poor maternal nutrition, especially folic acid deficiency, is a well-established risk factor for neural tube defects like anencephaly. Chronic medical conditions such as diabetes and obesity can further elevate the risk. Maternal age, both advanced and very young, is associated with a higher incidence of some cephalic disorders.
Infections
Intrauterine infections, notably with Zika virus, cytomegalovirus, rubella, and toxoplasma, can disrupt normal brain development and increase the likelihood of microcephaly and other cephalic disorders. Screening for infectious diseases during pregnancy is therefore crucial.
Toxins and Other Risk Factors
Exposure to environmental toxins, including lead and mercury, can adversely affect foetal brain development. Additionally, trauma, radiation, and certain drugs taken during pregnancy may contribute to cephalic abnormalities. Multifactorial interactions often underlie the manifestation of these disorders, making risk assessment complex.
Clinical Presentation and Symptoms
The clinical manifestations of cephalic disorders vary widely depending on the specific condition, severity, and underlying cause. Common features include:
Developmental Delays
Children with cephalic disorders often exhibit delayed milestones in motor, speech, and cognitive domains. These delays may become apparent within the first few months of life and can range from mild to profound.
Neurological Deficits
Neurological symptoms may include seizures, spasticity, hypotonia, visual or auditory impairment, and difficulties with coordination and balance. In severe cases, disorders such as anencephaly result in absence of higher brain function.
Physical Manifestations
- Abnormal Head Shape: Microcephaly (small head), macrocephaly (large head), or misshapen skull (craniosynostosis).
- Craniofacial Abnormalities: Facial deformities, cleft lip/palate, or abnormal spacing of facial features.
- Hydrocephalus: Accumulation of cerebrospinal fluid leading to increased head size and pressure symptoms.
- Motor Impairments: Weakness, abnormal reflexes, and difficulties with movement.
Additional symptoms may include feeding difficulties, behavioural issues, and growth retardation. The presence and severity of these features guide further evaluation and management.
Diagnostic Approaches
Early and accurate diagnosis of cephalic disorders is essential for optimal management and counselling. Diagnostic strategies include:
Prenatal Screening
Routine antenatal care includes screening for congenital anomalies. Ultrasound examination between 18–22 weeks of gestation can identify major structural abnormalities like anencephaly, holoprosencephaly, and craniosynostosis. Maternal serum alpha-fetoprotein (AFP) levels may be elevated in neural tube defects.
Imaging Modalities
- Ultrasonography: First-line tool for prenatal and postnatal detection of cranial and brain anomalies.
- Magnetic Resonance Imaging (MRI): Provides detailed visualisation of brain structure and pathology, useful in complex cases.
- Computed Tomography (CT): Used to assess bone abnormalities in craniosynostosis and other skull defects.
Genetic Testing
Advances in molecular genetics enable identification of chromosomal abnormalities and gene mutations associated with cephalic disorders. Techniques include karyotyping, chromosomal microarray analysis, and targeted gene sequencing. Genetic counselling is recommended for affected families.
Clinical Evaluation
A thorough clinical assessment is essential, incorporating history, physical examination, developmental assessment, and evaluation of associated anomalies. Multidisciplinary involvement, including paediatricians, neurologists, and geneticists, improves diagnostic accuracy and care planning.
Treatment and Management
Management of cephalic disorders is tailored to the specific diagnosis, severity, and individual needs. Treatment approaches include medical interventions, surgical options, supportive care, and rehabilitation.
Medical Interventions
Medical management focuses on symptom control and prevention of complications. Anticonvulsants may be used for seizure control, while nutritional support is essential for children with feeding difficulties. Hormonal therapies and other medications may be indicated in select cases.
Surgical Options
- Craniosynostosis: Surgical correction (cranioplasty) to release fused sutures and permit normal skull growth, often performed in infancy.
- Hydrocephalus: Placement of a ventriculoperitoneal shunt to divert excess cerebrospinal fluid and relieve intracranial pressure.
- Encephalocele: Surgical repair to reposition brain tissue and close skull defects.
Surgical intervention may also be considered for cosmetic reasons or to improve function and prevent secondary complications.
Supportive Care
Supportive care is integral to improving quality of life and maximising developmental potential. This includes physical, occupational, and speech therapy; special education services; assistive devices; and psychosocial support for families. Nutritional management, respiratory support, and management of comorbidities are also essential.
Rehabilitation
Rehabilitative services aim to optimise functional outcomes and independence. Early intervention programmes, especially in cases of developmental delay, are associated with better long-term results. Family education and involvement are crucial components of rehabilitation.
Prognosis and Long-Term Outcomes
The prognosis for cephalic disorders depends on the type, severity, and associated complications. While some conditions are fatal, others permit survival with varying degrees of disability.
Quality of Life
Children with mild or moderate cephalic disorders may achieve significant developmental progress with appropriate medical and rehabilitative support. However, severe cases often result in profound intellectual, motor, and sensory impairments, limiting independence and social participation.
Survival Rates
- Anencephaly: Universally fatal, with death occurring within hours or days of birth.
- Microcephaly: Survival rates vary; prognosis depends on underlying cause and severity.
- Holoprosencephaly: Severe forms are often incompatible with life, while milder cases may survive with disabilities.
- Craniosynostosis: With timely surgical intervention, most children lead relatively normal lives.
Complications
Potential complications include recurrent seizures, feeding difficulties, respiratory problems, increased intracranial pressure, and risk of infections. These can impact growth, development, and overall health, necessitating ongoing medical supervision.
Nursing Care of Patients with Cephalic Disorders
Providing effective nursing care to patients with cephalic disorders requires specialized knowledge, multidisciplinary collaboration, and a compassionate, patient-centered approach.
Nursing Interventions
The specific nursing interventions for patients with cephalic disorders are guided by the type and severity of the condition, as well as the patient’s age and associated symptoms.
Promoting Neurological Function
- Monitor neurological status closely and report any changes immediately to the medical team.
- Administer prescribed medications for seizures, spasticity, or pain as indicated.
- Provide positioning and support to minimize pressure on the head and prevent further neurological impairment.
- Facilitate early intervention services for cognitive and motor development.
Managing Feeding and Nutrition
- Assess for feeding difficulties, which are common in infants with cephalic disorders due to poor suck and swallow coordination.
- Collaborate with speech and occupational therapists for feeding support.
- Provide enteral nutrition if oral feeding is unsafe or insufficient.
- Monitor weight gain and hydration status regularly.
Providing Respiratory Support
- Monitor for airway obstruction or aspiration, particularly in patients with craniofacial abnormalities.
- Maintain airway patency using appropriate positioning and suctioning as needed.
- Administer supplemental oxygen or respiratory support if indicated.
Preventing Infection
- Practice meticulous hygiene, especially in patients with open cranial defects or shunts.
- Monitor for signs of infection at surgical sites or shunt entry points.
- Educate families about signs and symptoms of infection and when to seek medical attention.
Pain and Comfort Management
- Assess for pain using age- and developmentally-appropriate pain scales.
- Administer analgesics as ordered and employ non-pharmacological comfort measures such as swaddling, gentle touch, and soothing environments.
- Minimize stimuli and promote rest as needed.
Supporting Mobility and Physical Development
- Facilitate physical therapy to promote muscle strength and prevent contractures.
- Provide splints or orthotic devices as prescribed.
- Assist with range-of-motion exercises and positioning for comfort and function.
Family Support and Education
Caring for a child with a cephalic disorder can be emotionally and physically overwhelming for families. Nurses play a vital role in supporting and educating families throughout the care continuum.
- Provide honest, compassionate communication about the diagnosis, prognosis, and expected outcomes.
- Offer education on the specific disorder, including management strategies, home care, and signs of complications.
- Guide families to community resources, early intervention programs, and support groups.
- Encourage family participation in care, fostering their skills and confidence.
- Respect cultural, religious, and personal beliefs when discussing care options and future planning.
Multidisciplinary Collaboration
Effective management of cephalic disorders requires a team approach. Nurses collaborate with:
- Neonatologists and pediatricians for medical management and monitoring.
- Neurosurgeons and craniofacial teams for surgical interventions, such as shunt placement or cranial reconstruction.
- Physical, occupational, and speech therapists for developmental support.
- Social workers and psychologists for emotional and psychosocial support.
- Genetic counselors for family planning and risk assessment.
Ethical and End-of-Life Considerations
Some cephalic disorders, such as anencephaly, are incompatible with long-term survival. Nurses are instrumental in providing compassionate end-of-life care, which may include:
- Managing symptoms and ensuring comfort through palliative measures.
- Supporting families in decision-making and bereavement.
- Facilitating spiritual care and honoring family wishes.
REFERENCES
- John Hopkins, Cephalic Disorders, https://www.hopkinsmedicine.org/health/conditions-and-diseases/cephalic-disorders
- Bhandari J, Thada PK. Neural Tube Disorders. https://www.ncbi.nlm.nih.gov/books/NBK555903/. [Updated 2022 Aug 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-.
- Developmental Diseases of the Nervous System. In: Ropper AH, Samuels MA, Klein JP, Prasad S, eds. Adams and Victor’s Principles of Neurology. 11th ed. McGraw Hill; 2019.
- Gressens P, Passemard S, Huppi PS. Normal and Abnormal Brain Development. In: Fanaroff and Martin’s Neonatal-Perinatal Medicine: Diseases of the Fetus and Infant. 11th ed. Elsevier; 2020:914.
- Lyons K. Smith’s Recognizable Patterns of Human Malformation. Elsevier – Health Science; 2021. Multiple sections reviewed.
- Cephalic Disorder: Types & Care, https://www.acibademhealthpoint.com/cephalic-disorder-types-care/
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





