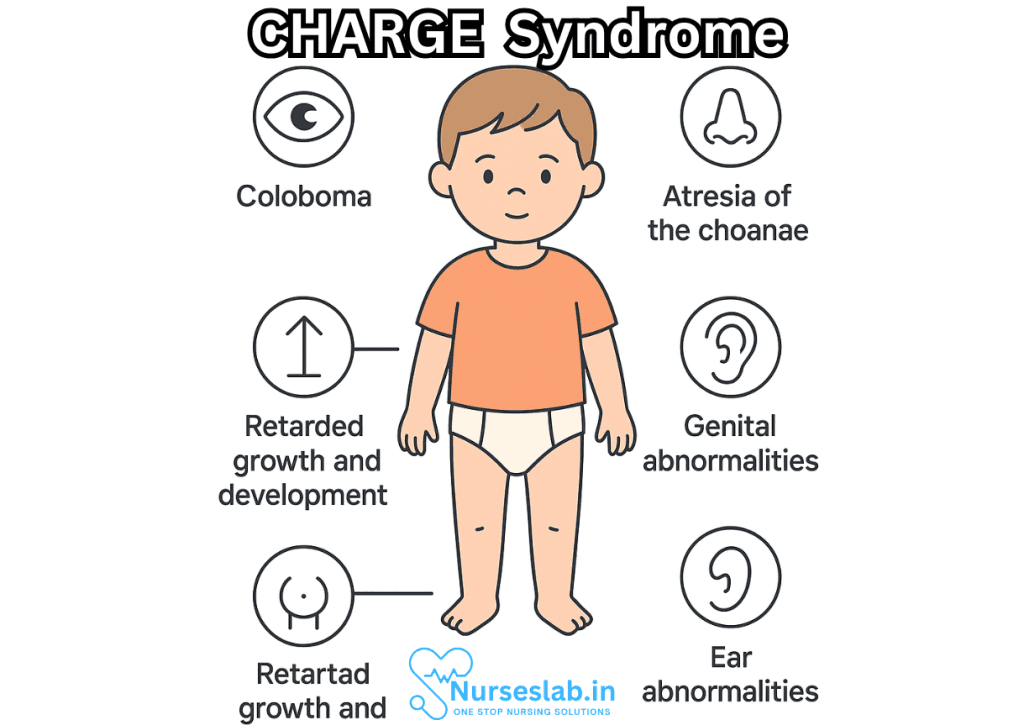
CHARGE syndrome is a rare and complex genetic disorder that affects multiple organ systems and presents with a wide range of physical and developmental challenges. The name “CHARGE” is an acronym that reflects the key features commonly seen in affected individuals: Coloboma, Heart defects, Atresia of the choanae, Retardation of growth and development, Genital abnormalities, and Ear abnormalities and deafness. First described in medical literature in the late 1970s, CHARGE syndrome has since been recognized as a distinct clinical entity with varied manifestations and a significant impact on quality of life.
What is CHARGE Syndrome?
CHARGE syndrome is considered a genetic disorder with physical abnormalities and developmental delays. It occurs in approximately 1 in 8,500 to 1 in 15,000 live births, though the actual incidence may be higher due to underdiagnosis or misclassification. The syndrome is highly variable—no two individuals are affected in exactly the same way, and the severity of symptoms can range from mild to profound.
Features of CHARGE Syndrome: The Meaning Behind the Acronym
The term “CHARGE” stands for six main clinical features, though many patients may show additional symptoms.
- Coloboma of the eye: Coloboma refers to a missing piece of tissue in structures of the eye, such as the iris, retina, choroid, or optic disc. This feature can result in vision impairment, ranging from mild to blindness, and is present in roughly 80–90% of individuals diagnosed with CHARGE syndrome.
- Heart defects: Congenital heart defects are found in around 75–85% of people with CHARGE syndrome. These defects can include atrial or ventricular septal defects, tetralogy of Fallot, patent ductus arteriosus, and other complex malformations. The severity of heart disease varies and can be life-threatening.
- Atresia of the choanae: Choanal atresia denotes a blockage of the nasal passages, which can be unilateral or bilateral. Bilateral atresia, in particular, can cause critical breathing difficulties in newborns, requiring immediate intervention.
- Retardation of growth and development: Growth retardation is common, with many children exhibiting low birth weight and short stature. Developmental delays, including motor, cognitive, and speech delays, are present in a majority of cases.
- Genital abnormalities: Genital hypoplasia, or underdevelopment of the genital organs, is often seen, especially in males, who may have micropenis, undescended testes, or other anomalies. Females may have hypoplastic labia or other reproductive differences.
- Ear abnormalities and deafness: These can include external ear malformations (such as “lop ear” or “cup ear”), middle and inner ear defects, and hearing loss, which may range from mild to profound. Hearing loss is found in up to 90% of affected individuals.
Many other features may be present, such as cleft lip/palate, facial palsy, feeding difficulties, tracheoesophageal fistula, and skeletal abnormalities.
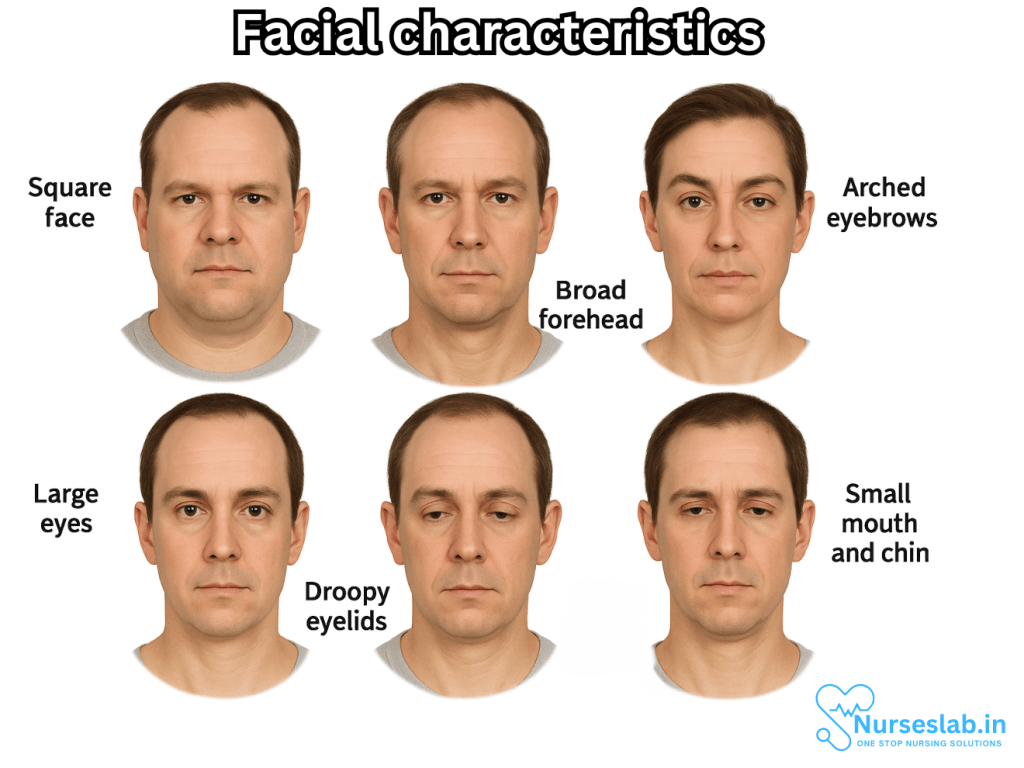
Facial characteristics
Children diagnosed with CHARGE syndrome have unique facial features that include:
- Square face.
- Broad forehead.
- Arched eyebrows.
- Large eyes.
- Droopy eyelids.
- Small mouth and chin.
- Asymmetrical face.
Genetic Causes of CHARGE Syndrome
Most cases of CHARGE syndrome are caused by mutations in the CHD7 gene located on chromosome 8q12.2. The CHD7 gene encodes a protein involved in chromatin remodeling—a process essential for turning genes on and off during development. The majority of mutations arise de novo, meaning they are new changes in the affected individual and not inherited from parents.
Though CHD7 mutations account for about two-thirds of clinically diagnosed cases, some individuals meeting diagnostic criteria do not have detectable CHD7 mutations, suggesting that other genetic or environmental factors may play a role.
Diagnosis of CHARGE Syndrome
Diagnosis is based on clinical features and may be confirmed by genetic testing. Because of its variability, not all individuals will have every classic feature, and the diagnosis may evolve as a child grows and develops. The most widely-used criteria for diagnosis include:
- Major features: Coloboma, choanal atresia, cranial nerve abnormalities, and ear anomalies.
- Minor features: Heart defects, genital hypoplasia, growth deficiency, orofacial clefts, tracheoesophageal fistula, and others.
A diagnosis of “typical CHARGE syndrome” usually requires the presence of several major features and some minor features, or identification of a pathogenic CHD7 mutation.
Clinical Presentation and Associated Complications
CHARGE syndrome affects virtually every aspect of health. The range of complications includes:
- Newborn breathing difficulties due to choanal atresia, laryngeal anomalies, or cranial nerve dysfunction.
- Feeding problems from cleft palate, swallowing difficulties, or poor muscle tone.
- Recurrent infections, especially of the ears, sinuses, and respiratory tract.
- Delayed growth and short stature, often complicated by feeding issues and hormonal deficiencies.
- Hearing and vision impairments that significantly impact learning and communication.
- Developmental delays and intellectual disability, which may be mild or profound.
- Behavioral challenges, including autism spectrum features, attention deficit, and sensory processing difficulties.
- Physical malformations such as facial asymmetry, limb differences, and scoliosis.
Management and Treatment Approaches
Because CHARGE syndrome is so variable, management must be individualized and multidisciplinary. Early and aggressive intervention can make a significant difference in outcomes.
- Medical management begins at birth, often with airway support, heart surgery if needed, and feeding assistance (such as gastrostomy).
- Hearing and vision support includes hearing aids, cochlear implants, communication devices, and vision therapy as appropriate.
- Physical, occupational, and speech therapy help address motor delays, feeding problems, and communication challenges.
- Surgical interventions may be required to correct choanal atresia, heart defects, cleft palate, genital anomalies, and other structural problems.
- Developmental support with early intervention programs and individualized education plans (IEPs).
- Psychosocial and behavioral support for families and children to help manage emotional, social, and behavioral difficulties.
Families of children with CHARGE syndrome often benefit from genetic counseling, support groups, and specialized resources.
Prognosis and Quality of Life
The prognosis for individuals with CHARGE syndrome depends on the severity of malformations and associated health problems. Advances in medical care have improved survival and long-term outcomes. Many children now survive into adulthood, though they may require ongoing medical, educational, and social support.
Quality of life can be significantly enhanced by early intervention, tailored therapies, and strong family and community support networks. Individuals may live independently or with minimal assistance, pursue education, and participate in meaningful social and recreational activities.
Living with CHARGE Syndrome: Stories of Resilience
Families and individuals living with CHARGE syndrome face many challenges, but resilience and adaptability are recurring themes in their stories. Support from healthcare professionals, educators, and advocacy organizations helps families navigate complex medical, developmental, and social landscapes. With the right resources, children and adults with CHARGE syndrome can thrive, learn new skills, and build meaningful relationships.
Nursing Care of Patients with CHARGE Syndrome
Nursing care for patients with CHARGE Syndrome is holistic, family-centered, and often lifelong. Nurses serve as advocates, coordinators, educators, and direct caregivers. The following sections outline common challenges in CHARGE Syndrome and evidence-based strategies for nursing management.
1. Assessment and Monitoring
Comprehensive Initial Assessment:
- Obtain a detailed history, including prenatal, perinatal, and family history.
- Assess for diagnostic criteria: coloboma, heart defects, choanal atresia or stenosis, growth retardation, genital anomalies, and ear abnormalities.
- Conduct thorough physical examinations, with particular attention to feeding ability, respiratory function, cardiac status, and neurodevelopmental milestones.
Ongoing Monitoring:
- Regularly monitor growth parameters (weight, height, head circumference).
- Monitor for developmental delays and refer for early intervention as needed.
- Assess for new symptoms or complications, such as infections, feeding or breathing difficulties, and behavioral changes.
2. Multidisciplinary Collaboration
CHARGE Syndrome requires a team approach:
- Coordinate care with physicians (pediatricians, cardiologists, ENT specialists, ophthalmologists, geneticists, endocrinologists).
- Work closely with allied health professionals (speech therapists, occupational therapists, physiotherapists, audiologists).
- Facilitate referrals and communication among various team members for seamless care transitions.
3. Respiratory and Airway Management
Many patients experience airway anomalies such as choanal atresia, laryngeal clefts, or tracheoesophageal fistulae.
- Monitor for signs of airway obstruction: cyanosis, stridor, labored breathing, apnea.
- Maintain clear airways through suctioning and appropriate positioning.
- Prepare for and assist with surgical interventions if required (e.g., choanal atresia repair).
- Educate families on signs of respiratory distress and the use of home equipment if necessary (e.g., suction devices, oxygen).
- Collaborate with respiratory therapists for the management of chronic or complex airway needs.
4. Feeding, Nutrition, and Growth
Feeding difficulties are very common and can be life-threatening, especially in infancy.
- Assess feeding ability: evaluate for swallowing dysfunction, aspiration risk, cranial nerve deficits, and oral-motor coordination.
- Support alternative feeding methods (e.g., nasogastric, gastrostomy, or jejunostomy tubes) as indicated.
- Monitor for adequate caloric intake, hydration, and growth.
- Collaborate with dietitians and speech-language pathologists for individualized nutrition plans and feeding therapy.
- Educate caregivers on safe feeding practices and tube care if applicable.
5. Cardiac Care
Congenital heart defects are present in up to 75% of patients.
- Monitor for signs of heart failure: tachypnea, poor feeding, failure to thrive, cyanosis.
- Administer cardiac medications as prescribed and monitor for side effects.
- Educate families on the importance of routine cardiac evaluations and signs of cardiac decompensation.
- Support families pre- and post-operatively during surgical interventions.
6. Sensory Impairments
- Facilitate regular vision and hearing screenings.
- Assist with the acquisition and maintenance of adaptive devices such as glasses, hearing aids, cochlear implants, and communication boards.
- Promote sensory integration through occupational therapy and encourage multi-sensory learning experiences.
- Support families in understanding and adapting to their child’s sensory needs.
7. Developmental and Educational Support
- Assess neurodevelopmental progress and provide early intervention referrals.
- Encourage play therapy, cognitive stimulation, and social interaction opportunities.
- Collaborate with educators to develop individualized education plans (IEPs) that address learning needs and accommodations.
8. Psychosocial Support and Family Education
CHARGE Syndrome impacts the entire family. Nurses provide essential support by:
- Offering counseling and psychological support to patients, siblings, and parents.
- Connecting families with resources, support groups, and advocacy organizations.
- Providing clear, honest education about the syndrome, its prognosis, and expected challenges.
- Empowering families through training and education on complex care needs, equipment usage, and emergency preparedness.
9. Management of Genital and Urinary Anomalies
- Assist in the monitoring and management of genital differences, which may require surgical intervention or hormone therapy.
- Encourage regular urological assessments and monitoring for urinary tract infections.
- Support discussions about sexual development and reproductive health as patients mature.
10. Prevention and Management of Infections
Children with CHARGE Syndrome are at higher risk for recurrent infections due to anatomical anomalies and immune dysfunction.
- Encourage adherence to immunization schedules.
- Monitor for early signs of infection and intervene promptly.
- Educate families about infection control practices at home and in the community.
11. Transition to Adulthood
As individuals with CHARGE Syndrome age, they require ongoing support through transitions.
- Prepare adolescents and families for transition to adult healthcare services.
- Promote self-advocacy and independence in age-appropriate ways.
- Support vocational and social integration efforts through collaboration with community agencies.
Ethical and Cultural Considerations
Nurses must be sensitive to the diverse values, beliefs, and cultural backgrounds of families affected by CHARGE Syndrome. Shared decision-making, respect for autonomy, and cultural competence are key elements. It is important to recognize and address any language barriers and to collaborate with interpreters or cultural mediators when necessary.
Documentation and Communication
Accurate, timely, and comprehensive documentation is essential in the care of CHARGE Syndrome patients. Nurses should ensure that all assessments, interventions, and patient/family instructions are well-documented and communicated clearly to all members of the healthcare team.
REFERENCES
- National Library of Medicine. CHARGE Syndrome. https://medlineplus.gov/genetics/condition/charge-syndrome/.
- Bergman JE, Janssen N, Hoefsloot LH, Jongmans MC, Hofstra RM, van Ravenswaaij-Arts CM. CHD7 mutations and CHARGE syndrome: the clinical implications of an expanding phenotype. J Med Genet. 2011 May;48(5):334-42. doi: 10.1136/jmg.2010.087106.
- National Organization for Rare Disorders, Inc. CHARGE Syndrome. https://rarediseases.org/rare-diseases/charge-syndrome/.
- Zentner GE, Layman WS, Martin DM, Scacheri PC. Molecular and phenotypic aspects of CHD7 mutation in CHARGE syndrome. Am J Med Genet A. 2010 Mar;152A(3):674-86. doi: 10.1002/ajmg.a.33323.
- The CHARGE Syndrome Foundation. Overview. https://www.chargesyndrome.org/about-charge/overview/.
- Hale CL, Niederriter AN, Green GE, Martin DM. Atypical phenotypes associated with pathogenic CHD7 variants and a proposal for broadening CHARGE syndrome clinical diagnostic criteria. Am J Med Genet A. 2016 Feb;170A(2):344-354. doi: 10.1002/ajmg.a.37435
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





