Chronic migraine is defined as headache occurring on 15 or more days per month for over three months, with at least eight days showing migraine features. Understanding its triggers, symptoms, diagnosis, and management is essential in neurology, nursing, and clinical practice.
Migraines are much more than just severe headaches; they are complex neurological conditions that can significantly impact an individual’s daily life. Among the various types of migraine disorders, chronic migraine is particularly debilitating, affecting millions of people worldwide.
Introduction
Migraine is a common neurological disorder characterised by recurrent episodes of moderate to severe headache, often accompanied by other symptoms such as nausea, vomiting, and sensitivity to light and sound. When migraine attacks become frequent and persistent, the condition may progress to what is known as chronic migraine disease.
Chronic migraine is not only physically disabling but also carries profound psychological, social, and economic burdens. With increasing awareness and research, our understanding of chronic migraine has evolved, leading to better diagnostic tools and more effective treatment strategies.
Definition and Diagnostic Criteria
What is Chronic Migraine?
Chronic migraine (CM) is a specific subtype of migraine defined by the frequency and duration of headache episodes. According to the International Classification of Headache Disorders, 3rd edition (ICHD-3), chronic migraine is diagnosed when a person experiences headaches on 15 or more days per month for more than three months, with at least eight of those days involving features of migraine headaches. This distinguishes chronic migraine from episodic migraine, where headache attacks occur less frequently—typically fewer than 15 days per month.
- Chronic Migraine: ≥15 headache days per month (for >3 months), with ≥8 days having migraine features
- Episodic Migraine: <15 headache days per month
Differences from Episodic Migraine
While both chronic and episodic migraines share similar symptoms, the key difference lies in the frequency and chronicity of attacks. Chronic migraine often leads to a more significant reduction in quality of life, increased risk of medication overuse, and greater healthcare utilisation compared to episodic migraine. The transition from episodic to chronic migraine is known as “migraine chronification,” a process influenced by various biological, psychological, and environmental factors.
Epidemiology and Prevalence
Who is Affected?
Chronic migraine is a global health concern, affecting approximately 1-2% of the general population. It is more prevalent among women than men, with a female-to-male ratio of about 3:1. The condition typically develops in individuals between the ages of 30 and 50, although it can occur at any age, including adolescence and older adulthood.
Global and Regional Statistics
- Worldwide, an estimated 80 crore (800 million) people suffer from migraine disorders, with a smaller but significant proportion meeting the criteria for chronic migraine.
- In India, migraine prevalence ranges from 10% to 15% of the population, and chronic migraine accounts for approximately 1-3% of all headache disorders.
- Chronic migraine is a leading cause of disability, ranking among the top neurological disorders in terms of years lived with disability (YLDs).
These statistics highlight the substantial personal and societal burden imposed by chronic migraine, underscoring the need for effective prevention, diagnosis, and management strategies.
Causes and Risk Factors
Genetic Contributors
Research indicates a strong genetic predisposition to migraine. Individuals with a family history of migraine, especially first-degree relatives, are at a higher risk of developing both episodic and chronic forms. Certain genetic mutations have been identified in rare familial migraine syndromes, but the genetics of chronic migraine are generally polygenic and multifactorial.
Environmental and Lifestyle Factors
- Stress: Chronic stress is a common trigger and risk factor for migraine chronification.
- Sleep disturbances: Poor sleep quality, insomnia, or irregular sleep patterns can contribute to increased headache frequency.
- Dietary factors: Skipping meals, dehydration, and consumption of trigger foods (such as chocolate, cheese, processed meats, and caffeine) are frequently reported by migraine sufferers.
- Hormonal influences: Fluctuations in oestrogen levels, especially during menstruation, pregnancy, or menopause, can affect migraine patterns, particularly in women.
- Medication overuse: Frequent use of acute headache medications (analgesics, triptans, ergotamines) can paradoxically worsen headaches, leading to medication overuse headache and chronic migraine.
- Other factors: Obesity, physical inactivity, and exposure to environmental pollutants may also increase the risk.
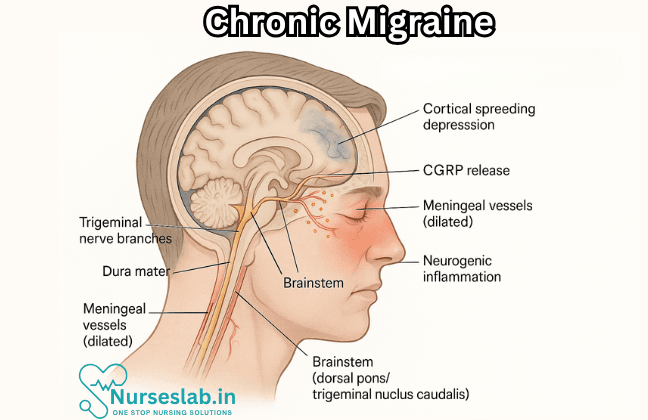
Pathophysiological Mechanisms
The precise mechanisms underlying chronic migraine remain incompletely understood. However, it is believed to involve alterations in the central nervous system, including increased cortical excitability, abnormal pain processing, and dysfunction of the brainstem and hypothalamic regions. Neuroinflammation, changes in neurotransmitter levels (such as serotonin and calcitonin gene-related peptide), and impaired inhibitory pathways are also implicated in migraine chronification.
Symptoms and Clinical Presentation
Common Symptoms
The hallmark symptom of chronic migraine is frequent, recurrent headache. These headaches typically have the following characteristics:
- Moderate to severe intensity
- Throbbing or pulsating quality
- Unilateral (one side of the head), but may be bilateral
- Worsening with physical activity
- Associated with nausea and/or vomiting
- Photophobia (sensitivity to light) and phonophobia (sensitivity to sound)
- Duration: 4–72 hours per attack, but in chronic migraine, some headaches may be continuous or nearly continuous
Less Common Symptoms
- Aura: Visual disturbances (flashing lights, blind spots), sensory changes, or speech difficulties preceding or accompanying the headache in some patients
- Neck pain or stiffness
- Dizziness or vertigo
- Allodynia (pain from normally non-painful stimuli, such as brushing hair)
Comorbidities
Chronic migraine often coexists with other medical and psychiatric conditions, which can complicate diagnosis and management. Common comorbidities include:
- Depression and anxiety disorders
- Sleep disorders (insomnia, sleep apnoea)
- Chronic pain syndromes (fibromyalgia, temporomandibular joint disorder)
- Gastrointestinal disturbances (irritable bowel syndrome)
Diagnosis
Diagnostic Process
Diagnosing chronic migraine is primarily a clinical process, based on a detailed patient history and assessment of headache patterns. There are no definitive laboratory tests or imaging studies to confirm the diagnosis, but investigations may be used to exclude secondary causes of chronic headache (such as tumours, infections, or vascular abnormalities).
- Patient history: Frequency, duration, and characteristics of headaches; associated symptoms; medication use; family history; lifestyle factors
- Headache diary: Patients may be asked to maintain a headache diary, documenting the number of headache days, severity, triggers, and response to treatment
- Physical and neurological examination: To rule out other neurological conditions
- Imaging: MRI or CT scan may be recommended if there are atypical features or red flags (sudden onset, neurological deficits, age >50, history of cancer)
Diagnostic Tools and Challenges
Several validated questionnaires and scales, such as the Migraine Disability Assessment (MIDAS) and Headache Impact Test (HIT-6), are used to assess the severity and impact of migraine. However, diagnosis can be challenging due to overlapping symptoms with other headache disorders, patient recall bias, and the stigmatisation of migraine as “just a headache”. Timely and accurate diagnosis is crucial for effective management and prevention of complications.
Treatment Options
Management of chronic migraine requires a comprehensive, individualised approach that addresses both acute attacks and long-term prevention. The goals of treatment are to reduce the frequency, severity, and duration of headaches, improve quality of life, and minimise the risk of medication overuse and side effects.
1. Acute (Abortive) Treatments
- Analgesics: Paracetamol, non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen are commonly used for mild to moderate attacks.
- Triptans: Serotonin receptor agonists (e.g., sumatriptan, rizatriptan) are effective for moderate to severe migraines, but should be used judiciously to avoid medication overuse.
- Ergot derivatives: Less commonly used due to side effects and contraindications.
- Antiemetics: For nausea and vomiting (e.g., domperidone, metoclopramide).
2. Preventive (Prophylactic) Treatments
- Beta-blockers: Propranolol, metoprolol
- Antiepileptics: Topiramate, valproate
- Tricyclic antidepressants: Amitriptyline, nortriptyline
- Calcium channel blockers: Flunarizine, verapamil
- OnabotulinumtoxinA (Botox): Approved for chronic migraine prevention; administered as injections every 12 weeks
- CGRP monoclonal antibodies: Erenumab, fremanezumab, galcanezumab—recently approved, these target the calcitonin gene-related peptide pathway involved in migraine attacks
3. Non-Pharmacological Therapies
- Cognitive behavioural therapy (CBT): Helps manage stress, coping strategies, and mood disorders
- Biofeedback and relaxation techniques: Useful in reducing headache frequency and severity
- Physical therapy: For associated neck pain, muscle tension
- Acupuncture: Some evidence for benefit in selected patients
4. Lifestyle Modifications
- Consistent sleep schedule
- Regular meals and hydration
- Exercise (e.g., yoga, walking, swimming)
- Identifying and avoiding triggers
- Stress management (meditation, mindfulness)
5. Management of Medication Overuse
Patients who overuse acute medications may develop medication overuse headache, complicating chronic migraine management. Gradual withdrawal under medical supervision, combined with preventive treatments, is recommended.
Living with Chronic Migraine
Impact on Quality of Life
Chronic migraine can have profound and far-reaching effects on all aspects of life. The unpredictability and frequency of attacks may result in missed work or school days, reduced productivity, and social withdrawal. Many patients experience feelings of frustration, isolation, and helplessness, particularly when their condition is misunderstood or minimised by others.
- Work and School: Frequent absences, reduced efficiency, and potential loss of employment or educational opportunities
- Family and Relationships: Strain on relationships due to inability to participate in family activities or fulfil responsibilities
- Mental Health: High rates of depression, anxiety, and sleep disturbances are reported among chronic migraine sufferers
- Financial Burden: Direct costs (medications, doctor visits) and indirect costs (loss of income, caregiver support)
Coping Strategies
- Practising self-care and prioritising mental health
- Joining support groups or patient advocacy organisations
- Open communication with employers, educators, and family members about the nature of the condition
- Developing a personalised migraine action plan with healthcare providers
Nursing Care for Patients with Chronic Migraine
Nurses play a crucial role in the holistic management of these patients, offering not only clinical interventions but also emotional and educational support.
Nursing Assessment
A thorough nursing assessment is pivotal for individualized care planning and ongoing evaluation. The assessment should involve:
Patient History
- Frequency, duration, and intensity of headaches
- Associated symptoms (aura, photophobia, phonophobia, nausea)
- Identifiable triggers
- Medication history, including over-the-counter and prescription drugs
- Impact on daily activities, work, and social life
- Psychosocial assessment: mood disorders, coping mechanisms, support systems
Physical Examination
- Vital signs
- Neurological assessment
- Assessment for medication side effects
- Signs of dehydration or malnutrition
Pain Assessment Tools
Nurses can utilize standardized pain assessment tools such as the Visual Analog Scale (VAS), Numeric Rating Scale (NRS), or Migraine Disability Assessment (MIDAS) questionnaire to quantify pain and disability.
Nursing Diagnosis
Common nursing diagnoses for patients with chronic migraine may include:
- Acute or chronic pain related to neurological dysfunction
- Ineffective coping related to chronic illness
- Disturbed sleep pattern due to pain or stress
- Risk for social isolation related to frequent attacks
- Knowledge deficit regarding migraine management and triggers
- Risk for medication overuse and related complications
Nursing Interventions
Holistic nursing interventions focus on both symptom management and the prevention of future attacks. Interventions may be classified as pharmacological, non-pharmacological, educational, and supportive.
Pharmacological Management
While nurses do not prescribe medication, they play a critical role in administering therapies and educating patients about their proper use.
- Ensure timely and correct administration of prescribed medications (preventive and abortive treatments)
- Monitor for adverse drug reactions, particularly with triptans, NSAIDs, and preventive agents such as beta-blockers, antiepileptics, and antidepressants
- Educate patients about risks of medication overuse headache (MOH)
Non-Pharmacological Management
Non-drug interventions are essential for long-term management and improving quality of life.
- Encourage regular sleep patterns and good sleep hygiene
- Promote stress reduction techniques: mindfulness, relaxation exercises, yoga, and meditation
- Facilitate trigger identification and avoidance: maintain a headache diary, nutritional counseling
- Apply cold compresses or heat to relieve pain
- Advise on the importance of adequate hydration and balanced diet
- Guide patients in gentle physical exercises to improve overall well-being
Education and Self-Management
Empowering patients with knowledge is a cornerstone of nursing care.
- Teach patients to recognize early signs and symptoms of migraine attacks
- Instruct on proper use and storage of medications
- Provide guidance on maintaining a headache diary for tracking patterns and triggers
- Educate families about supporting the patient during attacks
- Discuss the importance of regular follow-up and communication with healthcare providers
Psychosocial Support
Chronic migraine often leads to emotional distress, anxiety, and depression.
- Offer counseling or referral to mental health professionals as needed
- Facilitate support group participation for shared experiences and coping strategies
- Encourage open communication about feelings and concerns
- Foster a supportive environment to reduce stigma and feelings of isolation
Management of Acute Migraine Attacks
During an acute episode, immediate nursing interventions can help alleviate symptoms and prevent complications.
- Provide a quiet, dark room to minimize sensory stimulation
- Administer prescribed abortive medications promptly
- Monitor vital signs and neurological status
- Offer cool compresses or massage as per patient preference
- Assist with antiemetic administration if nausea or vomiting is present
Collaboration and Referral
Migraines often require multidisciplinary management. Nurses should collaborate closely with physicians, neurologists, psychologists, dietitians, and physical therapists.
- Facilitate referrals for advanced treatments (e.g., botulinum toxin injections, nerve blocks, cognitive behavioral therapy)
- Coordinate with dietitians for nutritional counseling
- Work with physical therapists to develop exercise and rehabilitation plans
- Communicate with pharmacists regarding medication safety and interactions
Monitoring and Evaluation
Continuous monitoring and evaluation are vital to ensure effective management and identify areas for improvement.
- Track frequency, intensity, and duration of migraine attacks
- Monitor patient adherence to medication and lifestyle modifications
- Assess for reduction in disability and improvement in quality of life
- Adjust care plans based on patient feedback and evolving needs
Patient and Family Education
Education is crucial not only for patients but also for their families.
- Provide information about the nature of chronic migraine and its impact
- Teach family members how to assist during acute attacks
- Discuss the importance of emotional support and understanding
- Encourage participation in educational sessions or workshops
Prevention Strategies
Preventing migraine progression and complications is a primary goal.
- Emphasize adherence to prescribed preventive therapies
- Support lifestyle modifications that reduce risk factors
- Encourage regular physical activity within patient’s tolerance
- Teach relaxation and coping techniques
- Promote regular follow-up visits for ongoing assessment and adjustment of care
Documentation
Accurate documentation ensures continuity of care and provides legal protection.
- Record all assessments, interventions, and patient responses
- Document medication administration, side effects, and patient education
- Update care plans based on changes in patient condition
REFERENCES
- Voelker R. What Is Chronic Migraine? JAMA. 2025;333(24):2216. doi:10.1001/jama.2025.4612
- Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3e https://pubmed.ncbi.nlm.nih.gov/29368949/. Cephalalgia. 2018;38(1):1-211.
- Kesserwani H. Migraine Triggers: An Overview of the Pharmacology, Biochemistry, Atmospherics, and Their Effects on Neural Networks. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8088284/. Cureus. 2021;13(4):e14243.
- Pescador Ruschel MA, De Jesus O. Migraine Headache. https://www.ncbi.nlm.nih.gov/books/NBK560787. [Updated 2022 Jul 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-.
- Hovaguimian A, Roth J. Management of chronic migraine BMJ 2022; 379 :e067670 doi:10.1136/bmj-2021-067670
- Schwedt TJ, Hentz JG, Sahai-Srivastava S, et al. Patient-Centered Treatment of Chronic Migraine With Medication Overuse: A Prospective, Randomized, Pragmatic Clinical Trial . https://pubmed.ncbi.nlm.nih.gov/35169011/. Neurology. 2022;98(14):e1409-e1421.
- Ropper AH, et al. Headache and other craniofacial pains. In: Adams and Victor’s Principles of Neurology. 12th ed. McGraw Hill; 2023. https://accessmedicine.mhmedical.com.
- Shankar Kikkeri N, Nagalli S. Migraine with Aura. https://www.ncbi.nlm.nih.gov/books/NBK554611/. [Updated 2022 Jul 5]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-.
- Charles AC, et al. Calcitonin gene-related peptide-targeting therapies are a first-line option for the prevention of migraine: An American Headache Society position statement update. Headache. 2024; doi:10.1111/head.14692.
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





