Chronic Traumatic Encephalopathy (CTE) is a degenerative brain disorder that has captured the attention of medical professionals, athletes, and the public alike. Often associated with repeated head trauma, CTE’s insidious progression and lingering effects challenge our understanding of the human brain, raising difficult questions about the costs of high-impact sports and the lasting consequences of injury.
Understanding Chronic Traumatic Encephalopathy
Chronic Traumatic Encephalopathy is a progressive neurodegenerative condition thought to result from repeated blows to the head. Historically, the disorder was first described in boxers and was known as “punch-drunk syndrome” or dementia pugilistica. However, the scope of Chronic Traumatic Encephalopathy has widened dramatically over the past decades, as evidence now implicates repetitive head injuries sustained in a variety of activities, from American football and soccer to military service and domestic violence.
Causes and Risk Factors
At the heart of CTE’s development lies repeated trauma. These traumas do not always need to result in full-blown concussions; even sub-concussive impacts—hits that are below the threshold for clinical concussion—may contribute to the gradual decline. The cumulative effect of these injuries over years, particularly without adequate recovery time, is believed to trigger pathological changes within the brain.
Risk factors for Chronic Traumatic Encephalopathy include:
- Frequency and severity of head impacts: The risk rises with increased exposure to head trauma over time.
- Occupation or activity: Participation in high-contact sports (e.g., football, boxing, hockey), military service with exposure to blast injuries, and situations involving repeated physical violence.
- Age of first exposure: Some studies suggest that starting contact sports before age 12 may heighten risks.
- Duration of exposure: Longer careers in high-impact activities mean greater cumulative risk.
Pathophysiology: What Happens in the Brain?
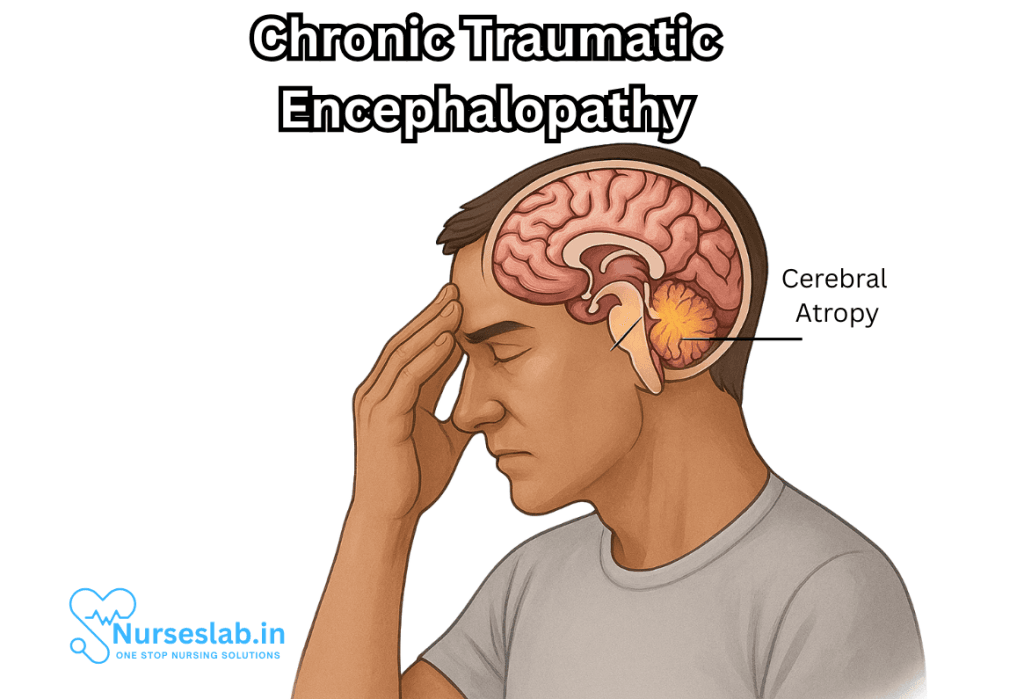
Chronic Traumatic Encephalopathy is characterized by the abnormal accumulation of the protein tau in the brain. Tau is a protein normally involved in stabilizing microtubules within neurons, but when it becomes defective, it forms tangles that disrupt normal brain function. In Chronic Traumatic Encephalopathy, tau pathology is often found around small blood vessels and deep within the folds of the brain’s cortex.
Over time, these changes trigger neurodegeneration, marked by:
- Loss of brain mass and shrinkage of critical regions, such as the frontal and temporal lobes.
- Scarring and atrophy.
- Disruption of neural circuits responsible for mood, cognition, and behavior.
The progression of CTE is slow, often taking years or decades to manifest, making early detection challenging.
Signs and Symptoms
The clinical presentation of Chronic Traumatic Encephalopathy can be subtle in its early stages. Symptoms tend to emerge years after the initial trauma, sometimes long after a person has ceased exposure to head injury. The major signs and symptoms include:
Behavioral and Mood Disturbances
- Depression, hopelessness, and apathy
- Impulsivity, irritability, and aggression
- Increased risk of substance abuse
- Emotional instability and suicidal thoughts
Cognitive Impairment
- Memory loss and confusion
- Difficulty concentrating and organizing thoughts
- Impaired judgment and decision-making
- Progressive dementia in advanced cases
Physical Symptoms
- Problems with balance and coordination
- Speech difficulties
- Motor impairment (less common than other symptoms)
It is crucial to note that these symptoms are not unique to Chronic Traumatic Encephalopathy and can overlap with other neurological or psychiatric conditions, which complicates diagnosis.
Diagnosis: Challenges and Advances
Diagnosing CTE remains one of the greatest hurdles in neuroscience. Currently, definitive diagnosis can only be made post-mortem, through neuropathological examination of the brain for tau deposits. Researchers are striving to develop reliable in vivo diagnostic tools, such as advanced imaging techniques and biomarkers, but these are not yet widely available or validated.
In living patients, diagnosis is based on medical history, history of repetitive head trauma, neurological examination, and exclusion of other diseases. Neuropsychological testing, MRI, and PET scans may be used to assess cognitive and structural changes, though none are definitive for Chronic Traumatic Encephalopathy.
Treatment and Management
There is no cure for CTE. Management focuses on alleviating symptoms and supporting the patient’s quality of life. Treatment strategies include:
- Medications: Antidepressants, mood stabilizers, and other drugs to address psychiatric symptoms.
- Therapies: Cognitive behavioral therapy, counseling, and rehabilitation.
- Support services: Structured routines, family education, and community resources.
- Prevention: Reducing exposure to head trauma, improving helmet technology, rule changes in sports, and education about the risks.
Family members and caregivers play a vital role in managing daily life and supporting those affected.
Societal Impact and Public Awareness
The growing recognition of CTE has prompted a cultural reckoning, especially in professional and youth sports. High-profile cases of former athletes suffering from CTE-related symptoms have led to lawsuits, policy changes, and greater scrutiny of sports organizations. The NFL, NHL, and other bodies have implemented concussion protocols, improved equipment standards, and altered game rules to reduce risk.
Beyond sports, CTE awareness has raised concerns in military and domestic contexts, underlining the need for comprehensive prevention and intervention strategies.
Nursing Care of Patients with Chronic Traumatic Encephalopathy (CTE)
Due to the complex and multifaceted nature of this condition, nursing care for patients with CTE demands a patient-centered, multidisciplinary approach, emphasizing both physical and emotional wellbeing.
Assessment and Nursing Diagnosis
Nursing assessment for individuals with suspected or confirmed CTE should be thorough and holistic, involving:
- Detailed history of traumatic brain injuries, including sports, military, or accident exposures
- Neurological assessment, focusing on cognition, speech, motor skills, and coordination
- Mental health evaluation for mood disorders, anxiety, or psychosis
- Functional evaluation of Activities of Daily Living (ADLs)
- Identification of safety risks—falls, self-harm, aggression
Potential nursing diagnoses include:
- Risk for injury related to impaired cognition or motor function
- Disturbed thought processes
- Impaired social interaction
- Risk for self-harm or violence
- Interrupted family processes
Planning and Interventions
Effective nursing care for CTE patients encompasses both direct physical care and emotional support. Interventions should aim to:
- Promote safety
- Support cognitive and behavioral functioning
- Manage comorbidities
- Educate and support families and caregivers
1. Ensuring Patient Safety
Environmental Modifications:
- Remove hazards to prevent falls—keep floors uncluttered, install grab bars, ensure adequate lighting.
- Supervise high-risk activities.
- Provide assistive devices as necessary (wheelchairs, walkers).
Managing Aggression and Impulsivity:
- Monitor for triggers that may lead to agitation or aggression.
- Use de-escalation techniques—calm voice, clear instructions, and positive reinforcement.
- Consider pharmacological interventions in collaboration with medical team if severe.
Monitoring for Self-Harm:
- Regularly assess for suicidal thoughts or behaviors.
- Implement suicide precautions if necessary—remove sharp objects, ensure close supervision.
2. Supporting Cognitive Functioning
Cognitive Rehabilitation:
- Engage patient in memory exercises and cognitive games
- Use calendars, reminders, and routines to support orientation
- Break tasks into simple, manageable steps
Communication Strategies:
- Speak slowly and clearly; use short sentences
- Allow extra time for response
- Repeat information as needed; use written instructions
Occupational Therapy Collaboration:
- Refer to occupational therapist for specialized cognitive and functional training
3. Managing Mood and Behavior
Psychoeducation:
- Educate patient and family about CTE symptoms and prognosis
- Discuss strategies to cope with mood swings, depression, or anxiety
Psychological Support:
- Encourage participation in individual or group therapy
- Connect with psychiatric professionals for evaluation and medication
Behavioral Modification:
- Implement reward systems for positive behaviors
- Redirect negative behaviors with constructive activities
4. Family and Caregiver Support
CTE often affects the entire family unit due to the patient’s decline in function and behavioral changes.
Education and Counseling:
- Provide practical information about disease progression and prognosis
- Teach management of difficult behaviors and communication techniques
Respite Care:
- Arrange for temporary relief for caregivers to prevent burnout
Community Resources:
- Connect families to support groups, social work, and legal resources for long-term care planning
5. Promoting Independence and Quality of Life
Encouraging Independence:
- Foster involvement in decisions about care and daily routines
- Support participation in familiar hobbies and interests
Physical Activity:
- Promote safe, regular exercise as tolerated to maintain strength and flexibility
- Coordinate with physical therapy for individualized programs
Nutrition and Hydration:
- Monitor for swallowing difficulties and implement safe feeding techniques
- Encourage balanced, nutritious meals
6. Managing Advanced CTE and Palliative Care
As CTE progresses, patients may require more advanced care, including palliative or hospice support.
- Assess for pain and discomfort—manage with appropriate medications
- Provide comfort measures and emotional support
- Respect patient and family wishes regarding end-of-life decisions
Interdisciplinary Collaboration
Nursing care for CTE patients is most effective when integrated with the expertise of neurologists, psychiatrists, psychologists, occupational and physical therapists, social workers, and speech therapists. Regular team meetings ensure continuity of care, address emerging issues, and foster holistic patient management.
Documentation and Evaluation
Nurses must document all assessments, interventions, and outcomes meticulously. Periodic evaluations, including feedback from the patient and family, help adapt care plans to meet evolving needs and optimize quality of life.
Challenges in Nursing Care
- Lack of definitive diagnostic criteria before death complicates management
- Stigma and misunderstanding about CTE may lead to missed or delayed care
- Caregiver stress and burnout are significant concerns
- Behavioral disturbances may require specialized management strategies
REFERENCES
- Adams JW, Alvarez VE, Mez J, et al. Lewy Body Pathology and Chronic Traumatic Encephalopathy Associated With Contact Sports. https://pmc.ncbi.nlm.nih.gov/articles/PMC6097837/. J Neuropathol Exp Neurol. 2018;77(9):757-768.
- Katz DI, et al. National Institute of Neurological Disorders and Stroke consensus diagnostic criteria for traumatic encephalopathy syndrome. Neurology. 2021; doi:10.1212/WNL.0000000000011850.
- Munakomi S, Puckett Y. Chronic Traumatic Encephalopathy. https://www.ncbi.nlm.nih.gov/books/NBK541013/. [2024 Oct 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-.
- National Health Service (U.K.). Chronic traumatic encephalopathy. https://www.nhs.uk/conditions/chronic-traumatic-encephalopathy/. Last reviewed 12/29/2025.
- Bieniek KF, et al. The second NINDS/NIBIB consensus meeting to define neuropathological criteria for the diagnosis of chronic traumatic encephalopathy. Journal of Neuropathology and Experimental Neurology. 2021; doi:10.1093/jnen/nlab001.
- National Library of Medicine (U.S.). Traumatic Brain Injury. https://medlineplus.gov/traumaticbraininjury.html. Last updated 2/12/2024.
- Halicki MJ, et al. Blood-based biomarkers in the diagnosis of chronic traumatic encephalopathy: Research to date and future directions. International Journal of Molecular Sciences. 2023; doi:10.3390/ijms241612556.
- Vink R, Corrigan F. Chronic traumatic encephalopathy: genes load the gun and repeated concussion pulls the trigger. https://pubmed.ncbi.nlm.nih.gov/35142676/. Neural Regen Res. 2022;17(9):1963-1964.
- Ruchika F, et al. Understanding the molecular progression of chronic traumatic encephalopathy in traumatic brain injury, aging and neurodegenerative disease. International Journal of Molecular Sciences. 2023; doi:10.3390/ijms24031847.
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





