Chronic Lymphocytic Leukemia (CLL) is a slow‑progressing cancer of mature lymphocytes, leading to immune dysfunction and abnormal blood counts. Understanding its symptoms, diagnosis, staging, and management is essential for nursing, pathology, and clinical practice.
Introduction
Chronic Lymphocytic Leukaemia (CLL) is a type of cancer that primarily affects the blood and bone marrow. It is characterised by the gradual accumulation of functionally incompetent lymphocytes, a type of white blood cell. CLL is the most common form of leukaemia in adults, particularly in Western countries, and is considered a chronic disease due to its slow progression in most cases.
Epidemiology and Demographics
CLL predominantly affects older adults, with the median age at diagnosis being around 70 years. It is rare in individuals below the age of 40 and extremely uncommon in children. The disease shows a higher prevalence in males compared to females, with a male-to-female ratio of approximately
While CLL is the most common leukaemia in Europe, North America, and Australia, its incidence in Asian populations, including India, is lower. However, with increasing life expectancy and improved diagnostic facilities, the reported cases in India are gradually rising.
The exact cause of CLL remains unknown, but several risk factors have been identified, including:
- Age: The risk increases with age.
- Gender: Males are more commonly affected.
- Family history: Having a first-degree relative with CLL increases the risk.
- Ethnicity: Higher prevalence in Caucasians.
- Genetic factors: Certain genetic mutations and chromosomal abnormalities are associated with increased risk.
- Environmental exposures: Exposure to certain chemicals, such as herbicides and insecticides, may play a role, though evidence is limited.
Pathophysiology
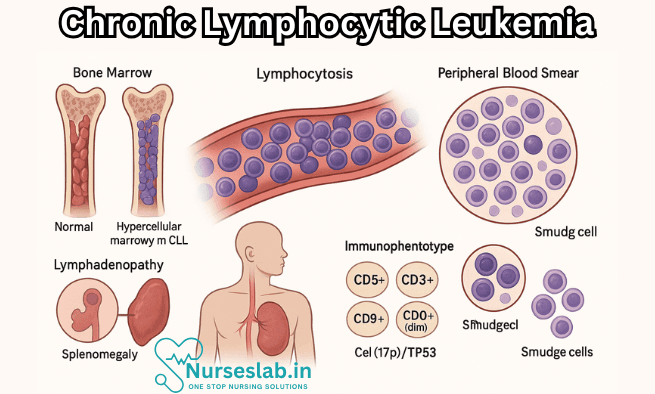
CLL is a clonal disorder of B lymphocytes, which are a subset of white blood cells involved in the immune response. In CLL, these lymphocytes undergo malignant transformation, leading to their uncontrolled proliferation and accumulation in the blood, bone marrow, lymph nodes, spleen, and sometimes the liver. The malignant cells are typically mature-looking but functionally defective, resulting in compromised immunity.
The underlying pathogenesis involves genetic mutations and chromosomal abnormalities. Common genetic changes in CLL include deletions of chromosomes 13q, 11q, and 17p, as well as trisomy 12. The most significant of these is deletion 17p, which involves the loss of the TP53 gene, associated with a poorer prognosis and resistance to standard therapies. Other molecular abnormalities, such as mutations in the IGHV, NOTCH1, and SF3B1 genes, also influence disease behaviour and treatment outcomes.
Clinical Presentation
CLL is often asymptomatic in its early stages and may be discovered incidentally during routine blood tests for unrelated conditions. When symptoms do occur, they are usually related to the accumulation of malignant lymphocytes and the resulting suppression of normal blood cell production. Common clinical features include:
- Lymphadenopathy: Painless swelling of lymph nodes, usually in the neck, armpits, or groin.
- Splenomegaly: Enlargement of the spleen, which may cause a feeling of fullness or discomfort in the left upper abdomen.
- Hepatomegaly: Enlargement of the liver (less common).
- Fatigue: A common and often debilitating symptom, resulting from anaemia or the disease process itself.
- Frequent infections: Due to immune suppression, patients are more susceptible to bacterial, viral, and fungal infections.
- Unexplained weight loss, fever, and night sweats: These are considered ‘B-symptoms’ and may indicate more advanced disease.
- Easy bruising or bleeding: As a result of low platelet counts (thrombocytopenia).
In some cases, CLL may transform into a more aggressive form of lymphoma, known as Richter’s transformation, which presents with rapidly enlarging lymph nodes, fever, and weight loss.
Diagnosis
The diagnosis of CLL is based on a combination of clinical findings, blood tests, and specialised investigations:
- Complete Blood Count (CBC): Elevated lymphocyte count (>5,000/μL) is a hallmark of CLL.
- Peripheral Blood Smear: Shows mature-appearing lymphocytes and characteristic ‘smudge’ cells.
- Immunophenotyping by Flow Cytometry: Confirms the presence of clonal B cells expressing markers such as CD19, CD20, CD23, and CD5.
- Bone Marrow Examination: Not always necessary for diagnosis, but may be performed to assess the extent of marrow involvement.
- Cytogenetic and Molecular Studies: Identify chromosomal abnormalities and mutations that have prognostic and therapeutic implications.
Staging of CLL is performed using the Rai or Binet systems, which assess the extent of lymphadenopathy, organomegaly, and cytopenias (anaemia, thrombocytopenia) to categorise disease severity and guide treatment decisions.
Natural History and Prognosis
The course of CLL is highly variable. Some patients have indolent disease that remains stable for many years without requiring treatment, while others experience rapid progression. Several factors influence prognosis, including:
- Genetic and molecular markers: Presence of high-risk mutations (e.g., TP53) indicates poorer outcomes.
- Stage at diagnosis: Advanced stage disease is associated with shorter survival.
- Patient age and comorbidities: Older age and other health problems can complicate treatment and affect prognosis.
- Response to therapy: Patients who respond well to initial treatment generally have better outcomes.
Median overall survival can range from more than 10 years in low-risk patients to less than 3 years in those with high-risk disease.
Treatment Strategies
Treatment of CLL is highly individualised and depends on several factors, including disease stage, patient age, overall health, genetic markers, and patient preferences. The main goals of therapy are to control symptoms, improve quality of life, and prolong survival. Importantly, not all patients require immediate treatment; a ‘watch and wait’ approach is often adopted for those with early-stage, asymptomatic disease.
Watch and Wait
Patients with early-stage disease and no symptoms are closely monitored without active treatment. This approach avoids unnecessary side effects of therapy, as early intervention has not been shown to improve survival in asymptomatic individuals.
Indications for Treatment
Treatment is initiated when one or more of the following criteria are met:
- Rapidly increasing lymphocyte count
- Symptomatic lymphadenopathy or splenomegaly
- Severe or worsening cytopenias (anaemia, thrombocytopenia)
- Constitutional symptoms (fever, night sweats, weight loss)
- Autoimmune complications not responsive to standard therapies
First-Line Therapies
The choice of first-line treatment depends on patient fitness and genetic features of the disease:
- Chemotherapy: Traditional regimens include fludarabine, cyclophosphamide, and rituximab (FCR). However, these are now less commonly used in older or unfit patients due to toxicity.
- Targeted Therapy: The advent of targeted agents has revolutionised CLL treatment. These include Bruton’s tyrosine kinase (BTK) inhibitors (e.g., ibrutinib, acalabrutinib), BCL-2 inhibitors (e.g., venetoclax), and phosphoinositide 3-kinase (PI3K) inhibitors. These agents are often preferred in patients with high-risk genetic features or those unable to tolerate chemotherapy.
- Monoclonal Antibodies: Rituximab, obinutuzumab, and ofatumumab are monoclonal antibodies targeting CD20, used alone or in combination with other agents.
Relapsed or Refractory Disease
Patients who relapse or do not respond to initial therapy may receive alternative targeted agents or participate in clinical trials. Allogeneic stem cell transplantation is considered in select younger patients with high-risk disease, but this approach carries significant risks.
Supportive Care
Supportive care is a critical component of CLL management and includes:
- Prevention and treatment of infections: Vaccinations, prophylactic antibiotics, and prompt treatment of infections.
- Management of cytopenias: Blood transfusions, growth factors, and treatment of autoimmune complications.
- Psychosocial support: Counselling and support groups to address the emotional and psychological impact of living with a chronic cancer.
Complications of CLL
CLL and its treatment are associated with several complications, including:
- Infections: Due to immunosuppression, infections are a leading cause of morbidity and mortality.
- Autoimmune phenomena: Autoimmune haemolytic anaemia and immune thrombocytopenia are relatively common.
- Richter’s transformation: Transformation to an aggressive lymphoma occurs in 2–10% of patients.
- Secondary cancers: Increased risk of skin cancers, lung cancer, and other malignancies.
- Treatment-related toxicities: Chemotherapy and targeted agents can cause a range of side effects, including myelosuppression, cardiac complications, and increased risk of bleeding.
Living with CLL: Quality of Life and Psychosocial Aspects
A diagnosis of CLL can have a profound impact on a patient’s quality of life. The chronic nature of the disease, uncertainty about prognosis, and the need for ongoing monitoring or treatment can cause significant psychological distress. Fatigue, anxiety, depression, and concerns about employment or family responsibilities are common.
Support from family, friends, and healthcare professionals is crucial. Patient education, access to counselling services, and participation in support groups can help individuals cope with the challenges of living with CLL. In India, cultural factors and social stigma may add additional layers of complexity, underscoring the importance of culturally sensitive care.
Nursing Care of Patients with Chronic Lymphocytic Leukemia (CLL)
The slow progression of the disease means patients may live for many years with CLL, but nursing care remains crucial for symptom management, infection prevention, education, and overall quality of life.
Assessment of the Patient with CLL
Effective nursing care begins with thorough assessment, including:
- History Taking: Symptoms such as lymphadenopathy, fatigue, fever, night sweats, unintentional weight loss, and recurrent infections are common. Detailed history regarding onset, duration, and progression of symptoms, as well as previous medical and family history, is essential.
- Physical Examination: Focus on lymph node enlargement, splenomegaly, hepatomegaly, pallor, petechiae, and signs of infection.
- Laboratory Investigations: Monitor complete blood count (CBC), lymphocyte count, immunoglobulin levels, and molecular markers. Bone marrow biopsy and flow cytometry are diagnostic tools.
Goals of Nursing Care
- Prevent and manage infections
- Promote comfort and manage symptoms
- Provide psychological support and education
- Monitor for disease progression and complications
- Support adherence to therapy and follow-up appointments
Nursing Interventions
1. Infection Prevention and Control
CLL patients are at high risk of infection due to immune dysfunction.
- Hand Hygiene: Adhere strictly to infection control protocols. Teach patients and families about proper handwashing techniques.
- Isolation Precautions: Implement protective isolation if neutropenia is present. Limit visitors with active infections.
- Monitor for Signs of Infection: Regular assessment for fever, cough, sore throat, and urinary symptoms. Report any abnormal findings promptly.
- Vaccination: Encourage annual influenza and pneumococcal vaccines. Live vaccines are generally contraindicated.
- Environmental Control: Maintain a clean environment. Avoid fresh flowers, raw fruits, and vegetables during periods of neutropenia.
2. Symptom Management
- Fatigue: Encourage energy conservation techniques. Balance activity with rest periods. Assess for anemia and provide transfusions as prescribed.
- Pain Management: Assess pain regularly using appropriate scales. Administer analgesics as needed and monitor for effectiveness and side effects.
- Bleeding Precautions: Monitor for signs of bleeding (petechiae, ecchymosis, hematuria). Avoid invasive procedures when possible. Use soft toothbrushes and avoid rectal temperatures or suppositories.
- Gastrointestinal Symptoms: Address nausea, vomiting, and anorexia with antiemetics, small frequent meals, and nutritional support.
- Lymphadenopathy and Organomegaly: Monitor for discomfort or restricted mobility due to enlarged lymph nodes or spleen. Provide comfort measures and educate regarding safe movement.
3. Psychological and Emotional Support
- Anxiety and Uncertainty: Offer emotional support, listen actively, and encourage expression of feelings.
- Education: Provide information about the disease process, prognosis, treatment options (e.g., chemotherapy, targeted therapies, immunotherapy), and potential side effects.
- Coping Strategies: Refer to counseling, social work, or support groups as needed. Encourage participation in decision-making and care planning.
- End-of-Life Considerations: For advanced disease, discuss advance directives and palliative care options in a sensitive and patient-centered manner.
4. Monitoring for Complications
- Regular Laboratory Monitoring: Track trends in CBC, renal and liver function, and markers of disease progression.
- Tumor Lysis Syndrome: Monitor for metabolic abnormalities during initiation of therapy (hyperuricemia, hyperkalemia, hypocalcemia, hyperphosphatemia). Ensure adequate hydration.
- Autoimmune Complications: Be alert for signs of hemolytic anemia or idiopathic thrombocytopenic purpura.
- Secondary Malignancies: Educate patients about the risk of other cancers due to immunosuppression or therapy.
5. Support for Treatment and Medication Adherence
- Chemotherapy and Targeted Therapy: Assess and manage side effects of drugs such as fludarabine, cyclophosphamide, rituximab, ibrutinib, and others.
- Oral Medication Adherence: Educate patients on the importance of taking medications as prescribed. Use pillboxes or reminders if necessary.
- Infusion Reactions: Monitor for allergic or infusion-related reactions during monoclonal antibody therapy. Have emergency medications available.
- Follow-up Appointments: Stress the importance of regular follow-up for disease monitoring and early detection of complications.
Patient and Family Education
Education is vital for empowering patients and their families:
- Explain the chronic nature of CLL and the expectation for long-term management.
- Discuss the purpose and potential side effects of prescribed treatments.
- Teach the recognition of infection, bleeding, and other warning signs that require immediate medical attention.
- Educate about nutrition, safe exercise, and other lifestyle modifications.
- Share available community resources and support networks.
Coordination of Care
CLL management requires a multidisciplinary approach:
- Collaborate with physicians, pharmacists, nutritionists, social workers, and other specialists.
- Arrange for home health services if indicated, especially during periods of immunosuppression or after intensive therapy.
- Communicate effectively with the healthcare team to ensure continuity of care and share updates regarding the patient’s condition.
Special Considerations for Older Adults
Since most CLL patients are older adults, nurses should:
- Assess for comorbidities such as diabetes, hypertension, cardiovascular disease, and renal impairment, which may affect treatment choices and tolerance.
- Evaluate cognitive function and the ability to participate in self-care.
- Adjust education and support strategies for visual, auditory, or mobility impairments.
Ethical and Legal Considerations
- Respect patient autonomy and informed consent in all treatment decisions.
- Maintain confidentiality and privacy regarding diagnosis and treatment.
- Recognize cultural and spiritual preferences, and incorporate them into care planning as appropriate.
REFERENCES
- American Society of Clinical Oncology. Leukemia — Chronic Lymphocytic — Introduction. https://www.cancer.net/cancer-types/leukemia-chronic-lymphocytic-cll/introduction.
- Kaushansky K, et al., eds. Chronic lymphocytic leukemia. In: Williams Hematology. 10th ed. McGraw Hill; 2021. https://accessmedicine.mhmedical.com.
- CLL Society. Information and Management. https://cllsociety.org/cll-information-and-management/. Multiple pages reviewed.
- Genetic and Rare Disease Information Center (GARD): Chronic lymphocytic leukemia. https://rarediseases.info.nih.gov/diseases/6104/chronic-lymphocytic-leukemia.
- Hallek M. Chronic Lymphocytic Leukemia: 2025 Update on the Epidemiology, Pathogenesis, Diagnosis, and Therapy. Am J Hematol. 2025 Mar;100(3):450-480. doi: 10.1002/ajh.27546. Epub 2025 Jan 28. PMID: 39871707; PMCID: PMC11803567.
- Niederhuber JE, et al., eds. Chronic lymphocytic leukemia. In: Abeloff’s Clinical Oncology. 6th ed. Elsevier; 2020. https://www.clinicalkey.com.
- Merck Manuals. Chronic Lymphocytic Leukemia. https://www.merckmanuals.com/home/blood-disorders/leukemias/chronic-lymphocytic-leukemia-cll?query=chronic%20lymphocytic%20leukemia.
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





