Introduction
Jaw implants, also known as mandibular implants or chin augmentation implants, represent a significant advancement in facial aesthetic and reconstructive surgery. Designed to enhance the jawline’s definition, correct asymmetries, or restore the natural contour lost due to trauma or congenital conditions, jaw implants have gained popularity among individuals seeking a more balanced and harmonious facial profile.
What are Jaw Implants?
Jaw implants are synthetic prosthetic devices placed surgically along the mandible (lower jaw) to augment its structure or restore its symmetry. They are typically made from biocompatible materials such as silicone, porous polyethylene (Medpor), or expanded polytetrafluoroethylene (ePTFE). These materials are well-tolerated by the body and designed to integrate securely with the surrounding bone and tissue.
Indications for Jaw Implants
Jaw implants are recommended for various purposes, including:
- Cosmetic Enhancement: To create a stronger, more defined jawline, especially for individuals with a weak or receding chin or jaw.
- Correction of Facial Asymmetry: To balance facial proportions affected by congenital deformities, trauma, or prior surgeries.
- Reconstructive Purposes: Following the removal of tumors, injuries, or bone loss due to medical conditions.
- Gender-Affirming Surgery: As part of facial masculinization or feminization procedures for transgender and non-binary individuals.
Candidacy: Who is a Good Candidate?
Ideal candidates for jaw implants are individuals who:
- Are in good general health and free from conditions that could compromise healing (such as uncontrolled diabetes or active infections).
- Have realistic expectations about the procedure and its outcomes.
- Lack significant bone loss that could impact implant placement.
- Are non-smokers or willing to quit before and after the procedure to optimize healing.
A thorough consultation with a board-certified oral and maxillofacial surgeon or plastic surgeon is essential. During this meeting, the surgeon will review the patient’s medical history, perform a physical examination, and may order imaging studies (e.g., X-rays, CT scans) to assess bone structure and determine the most appropriate implant size and shape.
Types of Jaw Implants
Jaw implants can be categorized based on their specific anatomical placement and intended outcomes:
- Chin Implants (Genioplasty): Placed at the front of the jaw to enhance chin prominence.
- Mandibular Angle Implants: Positioned at the back corners of the jaw to broaden and define the jawline.
- Custom Jaw Implants: Tailored to the individual’s anatomy for more complex cases or significant asymmetries.
The selection of implant type and material will be discussed in detail with the patient, considering their goals and anatomical needs.
The Surgical Procedure: Step-by-Step
1. Preoperative Preparation
Before surgery, patients will undergo a comprehensive evaluation. They may be advised to:
- Undergo lab testing or medical evaluation.
- Adjust current medications as recommended by the surgeon.
- Avoid certain medications that increase bleeding risk (e.g., aspirin, non-steroidal anti-inflammatory drugs).
- Stop smoking and avoid alcohol as directed.
2. Anesthesia
Jaw implant surgery is typically performed under general anesthesia, ensuring the patient is completely asleep and pain-free. In some less extensive cases, local anesthesia with sedation may be an option.
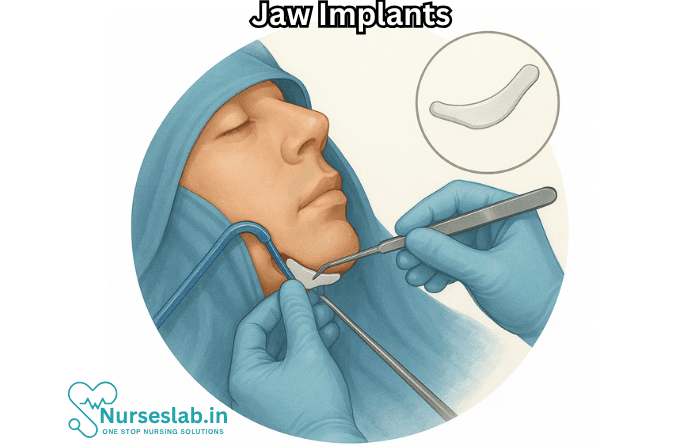
3. Incision and Implant Placement
The surgeon makes small, well-concealed incisions either inside the mouth (intraoral approach) or under the chin. The intraoral approach is preferred for minimizing visible scarring.
- An internal pocket is carefully created within the tissue overlying the jawbone.
- The selected implant is inserted and positioned precisely to achieve the desired augmentation or correction.
- In custom implant procedures, preoperative 3D imaging may be used to ensure a perfect fit.
- The implant is often secured with tiny screws or sutures to prevent shifting.
4. Closing the Incision
The surgeon closes the incision with dissolvable or removable sutures. If the incision is inside the mouth, it usually heals quickly and leaves minimal scarring.
5. Immediate Postoperative Care
After surgery, the patient is monitored in a recovery area before being discharged home, often on the same day for outpatient procedures.
Recovery Process
Recovery from jaw implants surgery varies but generally follows this timeline:
- First 48 Hours: Swelling, bruising, and mild discomfort are common. Pain medication and cold compresses help manage symptoms.
- First Week: Patients are advised to eat soft foods and avoid strenuous activity. Good oral hygiene is crucial, especially if incisions were inside the mouth.
- Follow-Up Visits: The surgeon will schedule visits to monitor healing and remove any non-dissolvable sutures if used.
- Full Recovery: Most swelling subsides within 2-4 weeks. Final results become apparent after several months.
Patients should avoid activities that may risk trauma to the jaw during the healing period. The surgeon will provide personalized instructions for care and recovery.
Risks and Potential Complications
As with any surgical procedure, jaw implant surgery has associated risks. These may include:
- Infection at the implant site
- Bleeding or hematoma formation
- Pain or numbness due to nerve injury
- Implant shifting or displacement
- Scarring (more likely with external incisions)
- Allergic reactions to implant materials (rare)
- Asymmetry or unsatisfactory cosmetic result
- Need for revision surgery
Selecting an experienced, board-certified surgeon significantly reduces these risks.
Expected Results and Longevity
Jaw implants provide immediate and long-lasting enhancement. The materials used are durable and can last for decades. Most patients are highly satisfied with the results, noting improved facial balance and self-confidence.
Final outcomes depend on individual anatomy, the type of implant, and strict adherence to post-operative care instructions.
Alternatives to Jaw Implants
For those hesitant about implants, alternative options include:
- Dermal Fillers: Temporary volumizing agents can add mild to moderate definition to the jawline.
- Fat Grafting: Uses the patient’s own fat to augment jaw structures.
- Orthognathic Surgery: For severe skeletal discrepancies, corrective jaw surgery may be recommended.
Each option has distinct advantages and limitations, and a skilled surgeon can help guide the best choice for the patient.
Nursing Care of Patients with Jaw Implants
Nursing care plays a pivotal role throughout the perioperative and postoperative process, ensuring patient safety, fostering healing, and minimizing complications. This document serves as a comprehensive guide to the nursing management of patients with jaw implants.
Preoperative Nursing Care
Patient Assessment and Preparation
- Medical History: Obtain a thorough history, including allergies, chronic illnesses (e.g., diabetes, bleeding disorders), previous surgeries, and current medications.
- Dental and Maxillofacial Assessment: Evaluate the oral cavity for signs of infection, poor dentition, or mucosal lesions. Collaboration with dental specialists is essential.
- Psycho-social Support: Assess the patient’s understanding of the procedure, expectations, and emotional readiness. Provide education about the surgery, possible outcomes, and potential complications.
- Preoperative Instructions:
- Advise on fasting if general anesthesia is planned.
- Instruct on oral hygiene measures to reduce infection risk (e.g., antiseptic mouthwash).
- Review and adjust medications as needed (e.g., anticoagulant management).
Immediate Postoperative Nursing Care
Monitoring and Assessment
- Vital Signs: Closely monitor blood pressure, pulse, respiratory rate, and oxygen saturation. Be alert for signs of shock or hypoxia.
- Airway Management: Swelling, bleeding, or hematoma formation can compromise the airway. Keep suction equipment and emergency airway supplies readily available.
- Pain Management: Administer prescribed analgesics and assess pain levels frequently. Encourage the use of cold compresses to reduce swelling and discomfort.
- Observation for Complications:
- Bleeding from the surgical site
- Signs of infection (fever, erythema, purulent discharge)
- Implant mobility or extrusion
- Nerve involvement (numbness, tingling, altered sensation)
Wound and Oral Care
- Inspect the surgical site for bleeding or signs of infection.
- Maintain strict aseptic technique during dressing changes or irrigation.
- Encourage or assist with gentle oral hygiene, avoiding the surgical site initially as per surgeon’s instructions.
- Advise the use of prescribed antiseptic mouthwashes and avoid commercial mouthwashes containing alcohol.
Diet and Hydration
- Start with clear fluids as tolerated. Gradually advance to a soft or pureed diet, avoiding hard, chewy, or spicy foods that can injure the surgical site.
- Monitor for signs of dehydration and encourage adequate fluid intake.
- Provide nutritional supplements if oral intake is compromised.
Ongoing Postoperative Nursing Care
Infection Prevention
- Teach proper hand hygiene and oral care techniques.
- Administer prophylactic antibiotics as prescribed.
- Monitor for fever, localized redness, swelling, or discharge.
- Promptly report any suspected infection to the surgical team.
Pain and Swelling Management
- Continue pain assessments using appropriate scales and administer analgesics as scheduled or as needed.
- Educate on the use of ice packs during the first 24–48 hours to minimize swelling. Heat application may be recommended later to resolve bruising or stiffness.
Support for Speech and Communication
- Jaw surgery and implants may temporarily impact speech. Offer communication aids as necessary (e.g., writing boards, picture charts).
- Refer to a speech therapist if difficulties persist or as part of the multidisciplinary care plan.
Facilitating Healing and Rehabilitation
- Encourage gentle jaw movements as allowed by the surgical team to prevent stiffness and promote function.
- Educate on signs of malocclusion or implant displacement, such as difficulty chewing or changes in bite alignment.
- Arrange follow-up appointments for suture removal, radiographic assessment, and ongoing evaluation of implant integration.
Patient Education and Discharge Planning
Home Care Instructions
- Provide written and verbal instructions on oral hygiene, medication schedules, and dietary modifications.
- Advise on avoiding trauma to the operative site and refraining from strenuous physical activity until cleared by the surgeon.
- Instruct patients on signs and symptoms that require immediate medical attention (e.g., persistent bleeding, severe pain, high fever, difficulty breathing).
Medication Management
- Ensure understanding of prescribed antibiotics, analgesics, and any adjunct medications.
- Discuss potential side effects and the importance of completing antibiotic courses.
Follow-up and Long-term Care
- Reinforce the importance of attending all scheduled follow-up visits for ongoing assessment and monitoring of implant integration.
- Encourage routine dental checkups and communication with healthcare providers regarding any oral changes.
- Address psychological aspects, as changes in appearance or function can impact self-image and confidence.
Management of Potential Complications
Infection
Infection is among the most serious complications. Early recognition and intervention are vital. Nursing staff should monitor for swelling, redness, warmth, pain, and discharge. If infection is suspected, notify the surgical team promptly and prepare for wound cultures, possible drainage, and intravenous antibiotics.
Bleeding and Hematoma
Persistent bleeding requires immediate medical attention. Nursing interventions include applying gentle pressure, monitoring vital signs for shock, and ensuring IV access if transfusion becomes necessary.
Implant Failure or Displacement
Monitor for abnormal movement, pain, or functional changes. Patients should avoid applying pressure to the site, and any suspected failure warrants urgent evaluation.
Nerve Injury
Numbness, paresthesia, or altered sensation is possible, particularly with mandibular implants. Document all neurological findings and provide support and reassurance. Referral to a specialist may be required for persistent symptoms.
Special Considerations
Pediatric and Geriatric Populations
Children and older adults may require additional support for communication, nutrition, and medication management. Tailor care plans to developmental or age-related needs.
Patients with Co-morbidities
Patients with diabetes, immunosuppression, or bleeding disorders are at higher risk for complications. Close monitoring, strict glycemic control, and coordination with other specialists are essential.
Role of Multidisciplinary Team
Collaboration and Communication
Optimal outcomes are achieved through collaboration among surgeons, nurses, dentists, speech therapists, nutritionists, and social workers. Regular team meetings and comprehensive documentation ensure coordinated, patient-centered care.
REFERENCES
- American Society of Plastic Surgeons. Facial Implants. https://www.plasticsurgery.org/cosmetic-procedures/facial-implants
- International Society of Aesthetic Plastic Surgery. Facial Implants. https://www.isaps.org/discover/patients-home/procedures/face-head-procedures/facial-implants/.
- The Cleveland Clinic. (2020) Facial implant surgery.
https://my.clevelandclinic.org/cosmetic-plastic-surgery/procedures/facial-implants-chin-surgery#results-tab - The Aesthetic Society. Facial Implants. https://www.theaestheticsociety.org/procedures/head-face/facial-implants. Last reviewed 4/28/2020.
- Dental and craniomaxillofacial implant surgery. Journal of Oral and Maxillofacial Surgery. 2023; https://www.clinicalkey.com.
- Dental implant procedures. American Academy of Periodontology. https://www.perio.org/for-patients/periodontal-treatments-and-procedures/dental-implant-procedures/.
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





