Introduction
Laparoscopy, also known as minimally invasive surgery or keyhole surgery, is a modern surgical technique that allows doctors to access the inside of the abdomen and pelvis without making large incisions in the skin. By using a specialized instrument called a laparoscope—a long, thin tube with a high-intensity light and a high-resolution camera at the front—surgeons can diagnose or treat various medical conditions with minimal trauma to the patient. This procedure represents a significant advancement over traditional open surgeries, offering quicker recovery times, reduced pain, and lower risk of complications.
The History and Evolution of Laparoscopy
The origins of laparoscopy date back to the early 20th century, when it was first used for diagnostic purposes. Over the decades, technological advances have refined the tools and techniques, leading to the widespread adoption of laparoscopic procedures in the 1980s and beyond. Today, laparoscopy is a standard approach in gynecology, general surgery, urology, and other medical specialties.
Indications for Laparoscopy
Laparoscopy can be performed for diagnostic or therapeutic purposes. Common indications include:
- Diagnosis of unexplained abdominal or pelvic pain
- Evaluation of infertility or reproductive health
- Biopsy of suspicious tissue or masses
- Treatment of conditions such as endometriosis, ovarian cysts, or ectopic pregnancy
- Gallbladder removal (cholecystectomy)
- Appendix removal (appendectomy)
- Hernia repair
- Treatment of some cancers (e.g., colorectal cancer)
- Assessment and management of adhesions (scar tissue)
Preoperative Preparation
Initial Assessment
Before the procedure, the patient undergoes a thorough evaluation, including medical history, physical examination, and necessary diagnostic tests (such as blood work, imaging studies, or electrocardiogram). The surgical team also discusses the risks, benefits, and alternatives to laparoscopy with the patient.
Fasting and Medication
Patients are usually advised not to eat or drink anything for 6–8 hours before the surgery. Some medications may need to be stopped or adjusted prior to the procedure, depending on the individual’s health status and the nature of the surgery.
Anesthesia
Laparoscopy is typically performed under general anesthesia, ensuring the patient remains asleep and pain-free during the operation.
The Laparoscopy Procedure: Step-by-Step
1. Patient Positioning and Preparation
The patient is positioned—often lying on their back—and the abdomen is cleansed with an antiseptic solution. Sterile drapes are placed to maintain a clean environment.
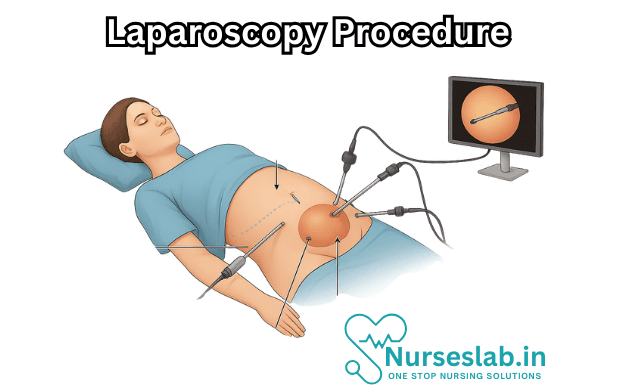
2. Creating Access: Incision and Trocar Placement
A small incision, usually about 1–2 centimeters, is made near the navel. A trocar, which is a sharp-pointed surgical instrument, is inserted through this incision. This device serves as a portal for the laparoscope and other instruments.
3. Insufflation of the Abdomen
Carbon dioxide gas is then gently pumped into the abdominal cavity. This process, called insufflation, inflates the abdomen and creates space for the surgeon to see and manipulate organs without risk of injury.
4. Insertion of the Laparoscope
The laparoscope is inserted through the trocar. The camera transmits real-time images to a video monitor, allowing the surgical team to visualize the internal organs in detail.
5. Placement of Additional Instruments
Depending on the type of surgery, one or more additional small incisions may be made to allow the insertion of specialized surgical instruments. These ports are placed strategically to provide optimal access to the target organs.
6. Surgical Intervention
The surgeon performs the necessary diagnostic or therapeutic procedures—such as removing the gallbladder, repairing a hernia, or taking a biopsy sample—using the long, thin instruments. Precision and dexterity are essential, as the surgeon is operating while viewing the magnified image on the monitor.
7. Removal of Instruments and Closure
Once the procedure is complete, the instruments and trocars are carefully withdrawn. The carbon dioxide gas is released from the abdomen, and the small incisions are closed with sutures, surgical glue, or adhesive strips. A sterile dressing is applied.
Postoperative Care and Recovery
In the Recovery Room
After surgery, the patient is transferred to a recovery area, where vital signs are closely monitored. Most patients are awake within an hour and can sit up and drink fluids once fully alert.
Pain and Discomfort
Mild to moderate pain or discomfort around the incision sites and in the shoulders (due to residual carbon dioxide irritating the diaphragm) is common. Pain relief medication is provided as needed.
Hospital Stay and Discharge
Many laparoscopic procedures are performed on an outpatient basis, allowing patients to go home the same day. More complex surgeries may require a brief hospital stay of one or two days.
At-Home Recovery
Complete recovery usually takes between a few days and two weeks, depending on the nature of the surgery and individual patient factors. Patients are advised to gradually resume normal activities while avoiding heavy lifting or strenuous exercise for several weeks.
Complications and Risks
While laparoscopy is generally safe, as with any surgery, there are potential risks and complications. These may include:
- Bleeding or infection at the incision sites
- Damage to internal organs (such as the bowel, bladder, or blood vessels)
- Adverse reaction to anesthesia
- Blood clots (deep vein thrombosis)
- Hernia at the incision site
- Pneumonia (rare)
- Adhesions or scar tissue formation
It is essential for patients to recognize warning signs after surgery—such as persistent fever, increasing pain, redness or discharge from wounds, difficulty breathing, or swelling in the legs—and to seek prompt medical attention if any of these occur.
Benefits of Laparoscopy
Compared to traditional open surgery, laparoscopy offers multiple advantages:
- Smaller incisions, resulting in less pain and minimal scarring
- Shorter hospital stays and faster return to normal activities
- Lower risk of infection and other complications
- Improved visualization of internal organs for the surgeon
- Reduced blood loss during surgery
These benefits have made laparoscopy the preferred approach for many abdominal and pelvic surgeries.
Limitations and Contraindications
Laparoscopy may not be suitable for everyone. Some conditions that might prevent a patient from having this procedure include:
- Severe obesity
- Extensive scar tissue from previous surgeries
- Extremely large tumors or masses
- Certain heart or lung conditions
- Uncontrolled bleeding disorders
In such cases, open surgery may be a safer or more effective option.
Nursing Care of Patients Undergoing Laparoscopy Procedures
The nurse plays a pivotal role throughout the perioperative continuum, providing holistic care that addresses not only the physiological needs but also the psychological, educational, and emotional well-being of the patient. This guide outlines the comprehensive nursing care required for patients undergoing a laparoscopy procedure.
Preoperative Nursing Care
Patient Assessment:
- Obtain a thorough medical history, including prior surgeries, allergies, current medications, and any chronic illnesses (e.g., diabetes, hypertension, respiratory or cardiac diseases).
- Assess for any risk factors that may complicate anesthesia or surgery, such as obesity, bleeding disorders, or pregnancy.
- Perform baseline vital signs and physical assessment, with special attention to the abdomen and respiratory status.
- Evaluate the patient’s psychological state, level of anxiety, and understanding of the procedure.
Patient Education:
- Provide detailed information about the laparoscopy procedure, including the purpose, risks, benefits, and expected outcomes.
- Explain the steps involved, such as the use of general anesthesia, the creation of small incisions, and the expected hospital stay.
- Discuss postoperative expectations, including pain management, mobility, wound care, and possible complications.
- Review fasting guidelines (NPO status), typically nothing by mouth for 6-8 hours before surgery.
- Address questions and concerns, offering reassurance and psychological support.
Physical Preparation:
- Confirm preoperative investigations (blood tests, ECG, imaging studies) and ensure all results are available for the surgical team.
- Ensure that the surgical consent form is signed and witnessed.
- Administer prescribed preoperative medications (e.g., antibiotics, anti-anxiety agents) as ordered.
- Assist the patient to change into a surgical gown and remove jewelry, dentures, contact lenses, and other personal items.
- Perform skin preparation as indicated, including cleansing the operative site.
- Insert an intravenous (IV) line for fluid and medication administration.
Emotional Support:
- Acknowledge the patient’s fears and anxieties, providing empathetic listening and reassurance.
- Offer support to family members and facilitate communication between the patient, family, and surgical team.
Intraoperative Nursing Care
Patient Safety and Positioning:
- Assist the anesthesia team in inducing general anesthesia and monitoring the patient.
- Ensure correct positioning on the operating table (commonly the supine or lithotomy position), with padding to prevent nerve injury and pressure ulcers.
- Apply safety straps and check for proper alignment.
Sterile Technique:
- Maintain strict aseptic technique to minimize the risk of surgical site infection.
- Assist in preparing surgical instruments and equipment for the laparoscopic procedure, including the laparoscope, monitors, insufflators, and light sources.
Monitoring and Documentation:
- Monitor the patient’s vital signs (heart rate, blood pressure, oxygen saturation, temperature) continuously.
- Observe for any signs of complications such as bleeding, arrhythmias, or respiratory distress.
- Document intraoperative events, medications administered, fluid balance, and any deviations from the planned procedure.
Assisting the Surgical Team:
- Anticipate the needs of the surgeons and provide necessary instruments promptly.
- Assist with specimen collection for pathological examination if indicated.
Immediate Postoperative Nursing Care
Patient Monitoring:
- Transfer the patient to the post-anesthesia care unit (PACU) and ensure a safe handover.
- Monitor vital signs and level of consciousness frequently according to hospital protocol.
- Assess airway, breathing, and circulation; provide supplemental oxygen if needed.
- Monitor pain level and administer analgesics as prescribed.
- Check surgical dressings and incisions for bleeding, swelling, or discharge.
- Monitor urinary output and ensure the patency of any drains or catheters.
Pain Management:
- Assess pain using a standardized pain scale and document findings.
- Administer prescribed pain medications (opioids or non-opioid analgesics) as needed.
- Encourage non-pharmacological pain relief measures (e.g., relaxation techniques, positioning, cold packs if indicated).
Prevention of Complications:
- Encourage deep breathing, coughing, and use of an incentive spirometer to prevent atelectasis and pneumonia.
- Assist with early ambulation as tolerated to reduce the risk of deep vein thrombosis (DVT) and promote bowel function.
- Monitor for signs of complications such as infection (fever, redness, purulent discharge), bleeding (tachycardia, hypotension, pallor), or gas embolism (sudden chest pain, shortness of breath).
- Ensure safe environment to prevent falls, especially in patients who are still drowsy from anesthesia.
Ongoing Postoperative Nursing Care
Wound Care:
- Inspect the surgical wounds daily for signs of infection or delayed healing.
- Perform dressing changes as ordered, maintaining strict aseptic technique.
- Educate the patient about wound care at home, including signs to report (redness, swelling, discharge).
Gastrointestinal Function:
- Monitor for the return of bowel sounds and the passage of flatus or stool.
- Gradually advance the diet from clear liquids to regular food as tolerated.
- Watch for signs of ileus, nausea, or vomiting, and notify the medical team if present.
Mobility and Activity:
- Encourage gradual increase in activity, including sitting up, standing, and walking with assistance as needed.
- Provide instruction on activity restrictions (e.g., avoiding heavy lifting or strenuous exercise) as per the surgeon’s advice.
Patient Education:
- Teach the patient and family about the expected recovery process, including timelines for return to normal activities.
- Provide information on medication regimen, wound care, warning signs of complications, and follow-up appointments.
- Encourage the patient to ask questions and express concerns.
Psychosocial Considerations
- Recognize the emotional impact of surgery and hospitalization on patients and their families.
- Provide psychosocial support, encourage family involvement, and facilitate communication regarding prognosis and recovery.
- Refer to counseling services or support groups if the patient exhibits significant anxiety or emotional distress.
Discharge Planning and Home Care
Preparation for Discharge:
- Assess readiness for discharge, including stable vital signs, adequate pain control, and ability to tolerate oral intake.
- Review discharge instructions carefully with the patient and caregiver.
- Arrange for home health services if necessary (e.g., wound care, physical therapy).
Home Care Instructions:
- Emphasize the importance of medication adherence and recognizing signs of infection or complications.
- Advise on maintaining a balanced diet, adequate hydration, and activity as tolerated.
- Provide contact information for the healthcare team in case of questions or emergencies.
Common Complications and Their Nursing Management
Infection:
- Monitor for fever, wound redness, swelling, or discharge; report promptly to the physician.
- Maintain aseptic technique during wound care and educate the patient about signs of infection.
Bleeding:
- Observe for hypotension, tachycardia, increased drainage, or pallor; report any abnormalities.
- Apply pressure dressings as ordered and prepare for intervention if significant bleeding occurs.
Deep Vein Thrombosis (DVT):
- Encourage early ambulation and leg exercises.
- Apply compression stockings or use sequential compression devices as prescribed.
- Monitor for calf pain, redness, or swelling.
Respiratory Complications:
- Encourage deep breathing exercises and use of incentive spirometer.
- Monitor oxygen saturation and watch for signs of respiratory distress.
- Provide supplemental oxygen if required.
Shoulder Pain:
- Shoulder pain is common after laparoscopy due to diaphragmatic irritation from CO₂ insufflation.
- Offer reassurance, provide pain relief, and encourage ambulation to facilitate reabsorption of gas.
REFERENCES
- American College of Obstetricians and Gynecologists. Laparoscopy. https://www.acog.org/womens-health/faqs/laparoscopy). Last reviewed 12/2022.
- National Health Service. Laparoscopy (keyhole surgery. https://www.nhs.uk/conditions/laparoscopy/). Last reviewed 12/20/2023.
- Society of Gastrointestinal Endoscopic Surgeons (SAGES). Diagnostic Laparoscopy Patient Information from SAGES. https://www.sages.org/publications/patient-information/patient-information-for-diagnostic-laparoscopy-from-sages/). Last revised 3/1/2015.
- Weledji EP. An overview of gastroduodenal perforation. Front Surg. 2020;7:573901. doi:10.3389/fsurg.2020.573901
- Soomro MA, Aftab M, Hasan M, Arbab H. Heineke-Mikulicz pyloroplasty for isolated pyloric stricture caused by corrosive ingestion in children. Pak J Med Sci. 2020 Jan;36(1):S87–S90. doi:10.12669/pjms.36.ICON-Suppl.1714
- Laparoscopy: What to expect at home. (2021).
https://myhealth.alberta.ca/Health/aftercareinformation/pages/conditions.aspx?hwid=zc2174
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





