Introduction
Laser cordotomy is a specialized neurosurgical procedure designed to alleviate chronic, severe pain, most commonly in patients with malignancies such as advanced cancer. It is a subset of cordotomy, a technique dating back to the early 20th century, which interrupts pain pathways within the spinal cord. By harnessing the precision and minimally invasive benefits of laser technology, laser cordotomy offers targeted pain relief while minimizing collateral damage to surrounding tissues. As medical science continues to evolve, laser cordotomy has become an invaluable tool in palliative care, improving quality of life for patients who have exhausted other avenues of pain management.
Anatomical and Physiological Basis
Understanding the rationale behind laser cordotomy requires knowledge of the neuroanatomy of pain transmission. The human spinal cord contains several pathways for sensory information, but the spinothalamic tract is paramount for the transmission of pain and temperature sensations. This tract runs within the anterolateral quadrant of the spinal cord, ascending from the dorsal horn to the thalamus.
The principle underlying cordotomy is the selective interruption of the spinothalamic tract. By disrupting this pathway, pain signals originating from the contralateral side of the body are prevented from reaching the brain, resulting in substantial pain relief without significant motor or proprioceptive deficits.
Indications
Laser cordotomy is primarily indicated for patients with unilateral, intractable cancer pain, especially when other modalities—pharmacological, interventional, or radiologic—have failed or are not appropriate. Common cancers for which this technique is considered include:
- Lung cancer
- Mesothelioma
- Head and neck cancers
- Abdominal and pelvic malignancies
Other indications may include severe non-malignant pain syndromes, but this is rare, given the irreversible nature of the procedure and the availability of alternative therapies.
Contraindications
Patients with bilateral pain, cognitive impairment, coagulopathies, or poor overall prognosis may not be suitable candidates. Additionally, laser cordotomy is not recommended if pain is diffuse or poorly localized, as interruption of the spinothalamic tract on one side will not provide adequate relief.
Preoperative Assessment
Candidate selection is crucial. A multidisciplinary team—including neurologists, pain specialists, oncologists, and neurosurgeons—performs an exhaustive evaluation of the patient’s clinical status, pain characteristics, imaging studies, and prior treatment history. The patient should be fully informed of the risks, benefits, and irreversible nature of the procedure, with informed consent documented.
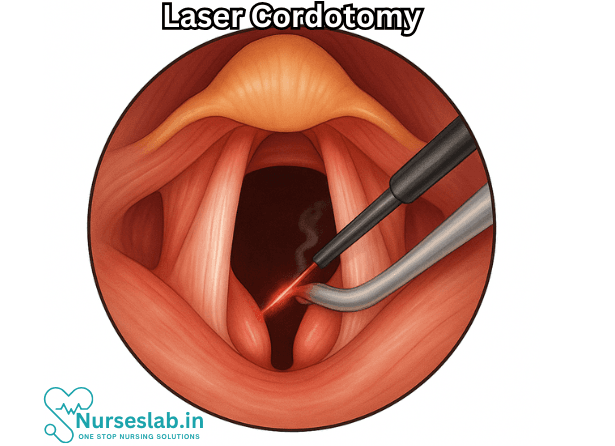
Surgical Technique
Laser cordotomy can be performed via percutaneous or open surgical approaches, though the percutaneous method is favored for its minimally invasive nature and expedited recovery.
- Preparation and Positioning: The patient is typically placed in a supine or lateral position, with the neck slightly flexed to allow precise targeting at the cervical spinal cord.
- Imaging Guidance: Advanced imaging techniques, such as CT or fluoroscopy, are utilized to identify the target area within the anterolateral quadrant of the cervical spinal cord, usually between C1 and C2 levels.
- Needle Insertion: Under sterile conditions and local anesthesia (occasionally with mild sedation), a specialized needle is introduced percutaneously into the cervical spinal cord at the designated level.
- Laser Ablation: Through the needle, a thin optical fiber connected to a laser generator is advanced into position. The laser, commonly a neodymium-doped yttrium aluminum garnet (Nd:YAG) or similar device, delivers focused energy to ablate the spinothalamic tract.
- Monitoring: Throughout the procedure, neurological status is closely monitored. Some centers employ intraoperative somatosensory evoked potentials or direct stimulation to confirm correct localization.
- Completion: After sufficient ablation, the fiber and needle are withdrawn, and the patient is observed for immediate complications.
Postoperative Care
Recovery from laser cordotomy is generally swift, with most patients experiencing a dramatic reduction in pain within hours. Postoperative monitoring focuses on neurological function, airway protection, and pain control. The patient may experience temporary numbness, sensory loss, or dysesthesia on the contralateral side, but motor function is usually preserved.
Outcomes and Efficacy
Laser cordotomy is recognized for providing rapid, profound pain relief. Studies indicate that up to 80-90% of appropriately selected patients achieve significant reduction in pain following the procedure. The degree and duration of relief depend on multiple factors, including cancer type, pain distribution, and procedural technique.
Advantages:
- Minimally invasive with short recovery time
- High efficacy for unilateral, localized pain
- Preservation of motor function
- Reduced need for systemic opioids and associated side effects
Limitations:
- Ineffective for bilateral or poorly localized pain
- Potential for sensory deficits
- Irreversible and non-curative
- Risk of complications (see below)
Complications and Risk Management
While laser cordotomy is generally safe when performed by experienced hands, as with any neurosurgical intervention, complications may arise. These include:
- Respiratory dysfunction, particularly with bilateral procedures, due to interruption of pain and temperature fibers critical for dyspnea perception
- Dysesthesia or neuropathic pain in the affected dermatome
- Transient or permanent numbness
- Motor weakness (rare)
- Infection, bleeding, or hematoma at the puncture site
- Spinal cord injury (extremely rare)
Most complications are minor and transient, but patients should be counseled about the possibility of persistent sensory changes.
Comparative Methods and Innovations
Laser cordotomy is one among several cordotomy techniques, including radiofrequency cordotomy and open surgical cordotomy. The precision and controlled ablation offered by the laser make it preferable in many contexts, though radiofrequency remains widely used and may be more cost-effective.
Emerging technologies, such as MRI-guided focused ultrasound, promise non-invasive alternatives in the future, but laser cordotomy currently stands as a gold standard for refractory unilateral cancer pain.
Nursing Care of Patients Undergoing Laser Cordotomy
Given the critical nature of the procedure and its impact on vital functions, meticulous nursing care before, during, and after laser cordotomy is essential to ensure patient safety, optimize outcomes, and support recovery.
Intraoperative Nursing Care
Assessment
- Review patient’s history, diagnosis, and indication for cordotomy.
- Assess baseline neurological status (motor, sensory, and autonomic function).
- Evaluate respiratory function, particularly in cases of vocal cord paralysis.
- Assess pain level using validated pain scales and document findings.
Patient and Family Education
- Explain the rationale, expected outcomes, and potential risks of the procedure.
- Discuss what to expect before, during, and after the surgery.
- Inform about fasting requirements (usually NPO 6-8 hours before procedure if under general anesthesia).
- Describe the postoperative course, including possible neurologic changes.
- Address concerns and answer questions to reduce anxiety.
Physical Preparation
- Ensure all preoperative investigations (labs, imaging) are complete.
- Obtain informed consent and confirm with the surgical team.
- Establish IV access for medication administration and hydration.
- Assist with preoperative skin preparation and marking of the surgical site as required.
- Prepare emergency equipment, especially suction and airway management tools if there is a risk of airway compromise.
Intraoperative Nursing Care
During the procedure, the nurse’s focus is on patient safety, monitoring, and assisting the surgical and anesthesia teams.
Responsibilities
- Monitor vital signs continuously, including pulse oximetry, ECG, and blood pressure.
- Maintain strict aseptic technique to prevent infection.
- Assist the anesthesiologist or surgeon as needed.
- Document intraoperative events, medications administered, and any changes in patient status.
- Be prepared to manage airway emergencies or other complications.
Postoperative Nursing Care
The postoperative period is critical for monitoring complications and supporting recovery.
Immediate Postoperative Care
- Transfer the patient to the post-anesthesia care unit (PACU) or intensive care unit for close observation.
- Monitor airway patency and respiratory function vigilantly, especially if the procedure involved the upper airway.
- Check vital signs frequently (every 15 minutes initially), watching for signs of hypotension, bradycardia, or hypoxia.
- Assess level of consciousness and orientation.
- Monitor neurological status (motor strength, sensory perception, pain sensation, reflexes).
- Evaluate for early signs of complications, such as hematoma, bleeding, or infection at the surgical site.
- Maintain IV fluids and monitor urine output; insert Foley catheter if indicated and monitor for retention or incontinence.
- Provide pain management as prescribed, monitoring for efficacy and side effects.
- Keep the patient in a comfortable, safe position, often flat for the initial hours unless otherwise directed.
Ongoing Postoperative Care
- Continue frequent monitoring of vital signs and neurological status until stable.
- Assess and document sensory or motor changes, particularly on the contralateral side to the procedure.
- Monitor temperature and pain sensation—loss of these can increase the risk for unrecognized injuries.
- Inspect the surgical site regularly for swelling, erythema, or discharge.
- Encourage early but safe mobilization to prevent complications such as deep vein thrombosis (DVT).
- Instruct patient and family on signs of complications to watch for (e.g., sudden weakness, loss of bladder control, fever).
Pain Management
Although the procedure is performed to reduce intractable pain, some discomfort or new pain may occur postoperatively.
- Assess pain using appropriate scales and provide prescribed analgesics.
- Monitor for neuropathic or new pain syndromes, which may require specialized management.
- Offer non-pharmacological comfort measures, such as positioning and relaxation techniques.
Patient and Family Education
Postoperative education is vital for safe recovery and prevention of injury.
- Teach the importance of protecting areas with diminished sensation—risk of burns or trauma increases due to loss of pain/temperature sensation.
- Instruct on pressure ulcer prevention, especially if mobility is affected.
- Review medication regimen, including the use of pain medications and possible side effects.
- Provide guidelines for activity, mobility, and when to resume normal activities.
- Explain the need for follow-up assessments and rehabilitation, if necessary.
- Encourage open communication regarding new or worsening symptoms.
Discharge Planning and Long-Term Considerations
Preparation for discharge and ongoing care is essential for patients who have undergone laser cordotomy.
- Coordinate with multidisciplinary teams, including physiotherapists, occupational therapists, and pain specialists.
- Ensure appropriate home modifications if there is loss of function or mobility.
- Arrange for community or home nursing support as needed.
- Reinforce education for self-care, skin inspection, and injury prevention.
- Schedule follow-up appointments and provide contact information for support services.
Psychosocial Support
The profound changes resulting from a laser cordotomy—especially in the context of chronic pain or cancer—can have significant emotional and mental health impacts.
- Assess for signs of anxiety, depression, or adjustment difficulties.
- Offer counseling support or referral to mental health professionals as appropriate.
- Include family in discussions and support plans.
- Encourage support group participation where available.
Summary Checklist for Nursing Care
- Comprehensive assessment and monitoring (neurological, respiratory, hemodynamic status)
- Meticulous infection control and wound care
- Effective pain management and patient comfort
- Patient and family education for safety and complication recognition
- Multidisciplinary approach to rehabilitation and discharge planning
- Provision of emotional and psychological support
Laser cordotomy is a valuable surgical option for select patients, but requires vigilant and compassionate nursing care at every stage. Through close monitoring, patient-centered education, and collaborative planning, nurses play a pivotal role in facilitating optimal recovery and enhancing the quality of life for patients undergoing this procedure.
REFERENCES
- American Speech-Language-Hearing Association. Vocal Fold Paralysis. https://www.asha.org/public/speech/disorders/vocal-fold-paralysis/.
- Khalil MA, Abdel Tawab HM. Laser Posterior Cordotomy: Is it a Good Choice in Treating Bilateral Vocal Fold Abductor Paralysis? Clin Med Insights Ear Nose Throat. 2014 Jul 3;7:13-7. doi: 10.4137/CMENT.S15888. PMID: 25057244; PMCID: PMC4085108.
- Virmani, Nitish; Dabholkar, Jyoti. Laser-assisted Posterior Cordotomy for Bilateral Vocal Fold Paralysis: Our Experience. Journal of Head & Neck Physicians and Surgeons 4(1):p 23-28, Jan–Jun 2016. | DOI: 10.4103/2347-8128.182852
- Khalil MA, Abdel Tawab HM. Laser Posterior Cordotomy: Is it a Good Choice in Treating Bilateral Vocal Fold Abductor Paralysis? (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4085108/) Clin Med Insights Ear Nose Throat. 2014 Jul 3;7:13-7.
- Salik I, Winters R. Bilateral Vocal Cord Paralysis. https://www.ncbi.nlm.nih.gov/books/NBK560852/?report=reader. 2023 Jul 10. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan.
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





