Limb salvage surgery has revolutionized the management of complex orthopedic conditions, providing hope and restored function for patients who once faced inevitable amputation. At the intersection of medical ingenuity and compassionate care, limb salvage represents not just a surgical procedure, but a holistic commitment to preserving both the form and function of a patient’s limb whenever possible.
Introduction
The loss of a limb can be a devastating event, not just physically, but emotionally and psychologically. While amputation once represented the standard of care for many severe limb injuries and tumors, advances in surgical techniques, biomaterials, and multidisciplinary care have made limb salvage a realistic and often preferable alternative in suitable cases. By definition, limb salvage surgery (LSS) comprises a set of complex procedures aimed at removing disease or damaged tissue while maintaining the maximum amount of healthy, functional limb tissue. Its overarching goal is to preserve quality of life—maintaining independence, mobility, and self-image.
Indications for Limb Salvage Surgery
Limb salvage is most commonly considered in the following scenarios:
- Bone and Soft Tissue Tumors: Osteosarcoma, Ewing’s sarcoma, chondrosarcoma, and various soft tissue sarcomas often arise in limbs. Where possible, removing the cancer while sparing the limb is preferable to amputation.
- Trauma: Severe injuries, including open fractures, vascular compromise, or crush injuries, may threaten limb viability. When feasible, reconstructive techniques can restore function and avoid amputation.
- Infection: Chronic osteomyelitis and deep soft tissue infections can erode bone and muscle. After removing infected tissue, reconstruction may save the limb.
- Vascular Disease: Peripheral arterial disease can lead to critical limb ischemia. In some cases, restoring blood flow and repairing tissue may allow for limb preservation.
- Congenital and Developmental Disorders: Some congenital deformities may require complex reconstructions best accomplished through limb-salvaging approaches.
Preoperative Evaluation and Planning
Successful limb salvage begins with meticulous preoperative planning. The patient undergoes a comprehensive assessment involving:
- Imaging Studies: X-rays, CT scans, MRI, and sometimes PET scans delineate the extent of disease or injury.
- Vascular Assessment: Doppler studies and angiography evaluate blood supply, which is critical for healing.
- Oncological Staging: In cases of cancer, determining the stage and local extent is key to planning resection margins.
- Functional Assessment: Evaluation of nerve and muscle function informs whether the limb will be usable post-surgery.
- Patient Factors: Age, comorbidities, psychosocial status, and preferences are all considered.
An interdisciplinary team—often including orthopedic and plastic surgeons, oncologists, radiologists, physiotherapists, and social workers—coordinates the plan to optimize both surgical outcomes and postoperative recovery.
Surgical Techniques in Limb Salvage
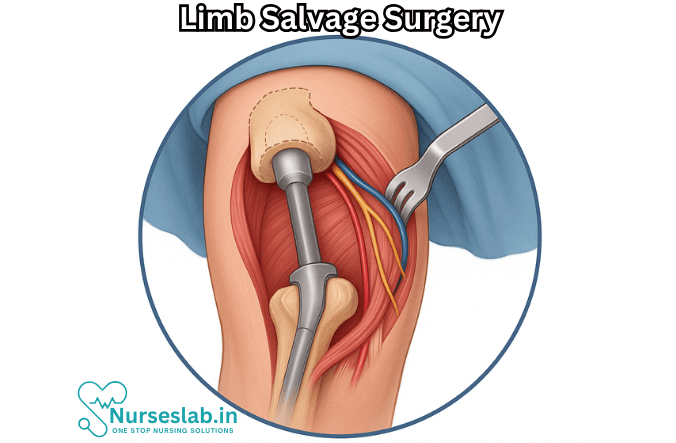
Limb salvage surgery is tailored to the patient’s diagnosis, age, and functional requirements. The mainstays of the procedure include:
1. Tumor Resection
The first and most essential step is the complete removal of diseased tissue (for example, a tumor) with a margin of healthy tissue to minimize the risk of recurrence. This may require removing segments of bone, muscle, blood vessels, and nerves.
2. Reconstruction
After resection, reconstructing the defect is crucial for restoring limb integrity and function. Techniques include:
- Endoprosthetic Replacement: Custom or modular metallic implants can replace resected bone, particularly around joints such as the knee or hip.
- Allografts: Cadaveric bone grafts may be used to bridge large bone gaps.
- Autografts: Tissue taken from the patient’s own body (e.g., fibula) can fill defects.
- Biological Reconstruction: Techniques like distraction osteogenesis gradually lengthen bone using an external fixator.
- Soft Tissue Coverage: Muscle or skin flaps, sometimes with microvascular free tissue transfer, are used to cover exposed implants or bone.
- Vascular and Nerve Repair: Microsurgical techniques may be needed to restore blood flow and nerve continuity.
3. Infection Control
Because limb salvage often involves prosthetics and extensive dissection, infection is a primary concern. Prophylactic antibiotics, antiseptic techniques, and sometimes antibiotic-impregnated materials are employed.
4. Functional Restoration
Efforts are made to maximize the limb’s function, whether by preserving joints, reconstructing tendons, or, in some cases, fusing joints in a stable position.
Risks and Complications
No surgery is without risk, and limb salvage presents unique challenges:
- Infection: Particularly when prostheses or large grafts are used.
- Non-union or Malunion: Bone grafts may fail to heal properly.
- Implant Failure: Endoprostheses may loosen, break, or wear out over time.
- Recurrence: In oncological cases, there is always a risk that cancer may return locally.
- Delayed Healing: Especially in patients with poor blood flow or underlying disease.
- Functional Limitations: Some loss of strength, range of motion, or sensation is common.
Despite these risks, advances in surgical methods and postoperative care have improved outcomes dramatically over the past several decades.
Rehabilitation and Recovery
Limb salvage does not end in the operating room. Rehabilitation is an essential phase, focusing on:
- Early Mobilization: Patients are encouraged to begin moving as soon as safely possible, sometimes with the aid of braces or assistive devices.
- Physical Therapy: Tailored exercises restore strength, flexibility, and endurance.
- Occupational Therapy: Helps patients adapt to changes in limb function and regain independence in daily activities.
- Pain Management: Both surgical pain and phantom limb sensations (in case of partial amputation) are addressed.
- Psychological Support: Adjusting to changes in body image and function is challenging; counseling and peer support are invaluable.
Rehabilitation may last several months or longer, depending on the complexity of surgery and the patient’s condition. The ultimate goal is to optimize the patient’s mobility, independence, and quality of life.
Outcomes and Quality of Life
The success of limb salvage surgery is measured not just in terms of limb preservation, but in long-term function and patient satisfaction. Many studies confirm that, when feasible, limb salvage offers comparable survival rates to amputation in cancer cases, with superior functional and psychological outcomes. Patients are often able to return to work, participate in recreational activities, and enjoy a high degree of autonomy.
Nevertheless, not every limb can or should be saved. In some circumstances—such as overwhelming infection, poor vascular supply, or uncontrollable disease—amputation may still provide the safest and most functional result. The decision process is individualized, weighing risks, benefits, and patient values.
Nursing Care of Patients Undergoing Limb Salvage Surgery
The nursing care of these patients is multifaceted, requiring in-depth knowledge of preoperative, intraoperative, and postoperative considerations, as well as expertise in rehabilitation, psychosocial support, and complication prevention.
Preoperative Nursing Care
Preparation for limb salvage surgery extends beyond medical readiness, encompassing psychological, educational, and logistical factors.
Patient Assessment
- Comprehensive Health History: Gather information about the underlying condition (e.g., osteosarcoma, Ewing’s sarcoma, trauma), previous treatments, allergies, and comorbidities.
- Physical Examination: Assess the affected limb for skin integrity, circulation, edema, range of motion, and neurovascular status. Evaluate for signs of infection or compromised tissue.
- Psychosocial Assessment: Address patient and family fears, expectations, and coping mechanisms. Identify social support systems and educational needs.
Patient and Family Education
- Explain the surgical procedure, expected outcomes, risks, and potential complications in clear, accessible language.
- Discuss anticipated postoperative limitations and the rehabilitation process.
- Prepare the patient for possible use of assistive devices, such as crutches, walkers, or wheelchairs.
- Emphasize the importance of infection prevention strategies and wound care.
Preoperative Preparations
- Ensure all diagnostic tests (imaging, blood work, ECG) are completed and reviewed.
- Coordinate consultations with relevant specialties (oncology, anesthesia, physiotherapy).
- Administer prescribed preoperative medications, including antibiotics if indicated.
- Maintain strict fasting guidelines to reduce aspiration risk during anesthesia.
- Promote relaxation through techniques such as deep breathing, guided imagery, or music therapy.
Intraoperative Nursing Considerations
Role in the Operating Room
- Assist in positioning the patient for optimal access and comfort, preventing pressure injuries or nerve compression.
- Maintain strict aseptic technique to minimize infection risk.
- Monitor vital signs and communicate any deviations to the surgical team promptly.
- Assist in handling and labeling of specimens for pathological analysis.
- Prepare the operating room for specialized equipment, such as prostheses or grafts, and ensure all necessary supplies are available.
Postoperative Nursing Care
The postoperative period is crucial for the restoration of function, prevention of complications, and psychological adaptation.
Monitoring and Assessment
- Vital Signs: Monitor blood pressure, heart rate, respiratory rate, and temperature at regular intervals. Watch for signs of hypovolemia, shock, or sepsis.
- Pain Management: Assess pain using appropriate scales and administer analgesics as prescribed. Consider multimodal pain management techniques (NSAIDs, opioids, nerve blocks).
- Limb Observation: Monitor the salvaged limb for color, warmth, capillary refill, swelling, and movement. Assess for compartment syndrome, vascular compromise, or signs of infection.
- Wound Care: Inspect dressings, monitor for bleeding or discharge, and observe for signs of dehiscence or necrosis.
Prevention and Management of Complications
- Infection Control: Maintain hand hygiene, use sterile techniques for dressing changes, and monitor for fever, redness, or purulent drainage. Administer antibiotics as prescribed.
- Deep Vein Thrombosis (DVT) Prevention: Encourage early mobilization, use compression stockings or devices, and administer anticoagulants per protocol.
- Neurovascular Complications: Perform frequent neurovascular checks (sensation, movement, pulses). Educate the patient to report numbness, tingling, or increased pain.
- Respiratory Care: Encourage deep breathing and coughing exercises to prevent atelectasis or pneumonia, especially in patients with limited mobility.
- Pressure Ulcer Prevention: Reposition the patient regularly and provide skin care, especially if movement is restricted.
Mobility and Rehabilitation
- Collaborate with physical and occupational therapists to develop a tailored rehabilitation plan.
- Assist with safe transfer and ambulation, initially with support and gradually increasing independence.
- Teach the patient exercises to enhance strength and flexibility in the salvaged limb and compensate for any functional loss.
- Encourage use of assistive devices as needed and ensure proper fitting and technique.
- Promote gradual increase in activity level, balancing rest with physical therapy requirements.
Pain and Psychosocial Support
- Validate the patient’s pain experience and respond promptly to requests for relief.
- Offer emotional support, addressing fears about appearance, function, and prognosis.
- Facilitate family involvement and encourage open communication about concerns and goals.
- Refer to counseling or support groups as appropriate, especially if the patient struggles with body image or adjustment issues.
Patient Education for Discharge and Home Care
- Provide detailed instructions on wound care, signs of infection, medication management, and follow-up appointments.
- Educate about lifestyle modifications, such as nutrition to promote healing and strategies to prevent falls or reinjury.
- Discuss the importance of adhering to prescribed rehabilitation exercises and attending therapy sessions.
- Inform about signs and symptoms that should prompt immediate medical attention, such as sudden swelling, loss of limb function, or persistent fever.
- Arrange for community nursing support or home health visits as needed.
Special Considerations
Pediatric and Geriatric Populations
- Children may require age-appropriate explanations, play therapy, and close monitoring of growth and development post-surgery.
- Older adults may have comorbidities or limited mobility requiring extra attention to fall prevention and nutritional status.
Oncologic Patients
- Coordinate care with oncology for those receiving chemotherapy or radiation before or after limb salvage.
- Monitor closely for immunosuppression and delayed wound healing.
Ethical and Cultural Considerations
- Respect cultural beliefs regarding surgery, body integrity, and rehabilitation practices.
- Involve interpreters or cultural mediators as needed to ensure clear communication and consent.
REFERENCES
- American Cancer Society. Surgery for Osteosarcoma. https://www.cancer.org/cancer/types/osteosarcoma/treating/surgery.html.
- Kadam D. Limb salvage surgery. Indian J Plast Surg. 2013 May;46(2):265-74. doi: 10.4103/0970-0358.118603. PMID: 24501463; PMCID: PMC3901908.
- Bonetumor.org. Overview of Limb Salvage Surgery (Limb Sparing Surgery for Bone Tumors. https://www.bonetumor.org/overview-limb-salvage-surgery-limb-sparing-surgery-bone-tumors.
- Kuek T, et al. (2023). The impact of cost on quality of surgical management in non-metastatic extremity sarcoma: A cross-country narrative literature review with a systematic approach.
https://journals.sagepub.com/doi/full/10.1177/10225536231168989#bibr25-10225536231168989 - Evans DR, Lazarides AL, Visgauss JD, Somarelli JA, et al. Limb salvage versus amputation in patients with osteosarcoma of the extremities: an update in the modern era using the National Cancer Database. https://pubmed.ncbi.nlm.nih.gov/33054722/). BMC Cancer. 2020 Oct 14;20(1):995.
- Before your operation for bone cancer. (2024).
https://www.cancerresearchuk.org/about-cancer/bone-cancer/treatment/surgery/before-your-operation - Macmillan Cancer Support. Limb-sparing surgery., https://www.macmillan.org.uk/cancer-information-and-support/treatments-and-drugs/limb-salvage-surgery.
- Qureshi MK, Ghaffar A, Tak S, Khaled A. Limb Salvage Versus Amputation: A Review of the Current Evidence. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7522192/. Cureus. 2020 Aug 28;12(8):e10092.
- Lazarides AL, et al. (2024). Mapping the course of recovery following limb-salvage surgery for soft-tissue sarcoma of the extremities.
https://journals.lww.com/jbjsjournal/abstract/2024/10020/mapping_the_course_of_recovery_following.7.aspx
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





