Lung Volume Reduction Surgery (LVRS) is a specialized procedure for severe emphysema that removes diseased, hyperinflated lung tissue to improve respiratory mechanics, enhance oxygen exchange, and relieve dyspnea—offering improved quality of life for select COPD patients unresponsive to medical therapy
Introduction
LVRS (Lung Volume Reduction Surgery) is a surgical intervention designed to improve lung function in patients suffering from severe emphysema, a form of chronic obstructive pulmonary disease (COPD). Emphysema is characterized by the destruction of alveoli, the tiny air sacs in the lungs responsible for oxygen exchange. The damage leads to reduced elasticity in the lung tissue, trapping air and causing over-inflation, which in turn makes breathing difficult and less efficient. LVRS aims to improve the quality of life and respiratory function by removing the most severely diseased portions of the lungs, thereby allowing the healthier parts to function more effectively.
Historical Perspective and Rationale
The concept of surgically removing diseased lung tissue to improve overall function was first introduced in the 1950s. However, it was not until the 1990s, with advances in surgical techniques and perioperative care, that LVRS began to gain wider acceptance. The rationale behind LVRS is based on the observation that the over-inflated portions of the lung occupy excessive space, compressing the healthier tissue and diaphragmatic movement. By reducing the volume of these non-functional areas, the remaining lung can expand more easily, improving ventilation and gas exchange.
Who Are Candidates for LVRS?
Not every patient with emphysema or COPD is a suitable candidate for LVRS. Careful patient selection is critical to achieving the best outcomes. The following criteria are typically considered:
- Severity of Disease: Candidates usually have severe, predominantly upper-lobe emphysema, as identified on imaging studies such as CT scans.
- Level of Disability: Patients should have significant symptoms, such as disabling shortness of breath (dyspnea), that persists despite optimal medical management and pulmonary rehabilitation.
- Non-Smoking Status: Candidates should have abstained from smoking for at least six months before surgery.
- Pulmonary Function Tests: Spirometry and other tests assess the degree of airflow limitation and the extent of hyperinflation. Typically, patients have a forced expiratory volume in one second (FEV1) between 20% and 45% of the predicted value, and a total lung capacity (TLC) greater than 100% of predicted.
- General Health: Adequate heart and other organ function is essential to safely undergo surgery and recover.
- No Severe Comorbidities: Conditions such as severe pulmonary hypertension or advanced heart failure may exclude patients from consideration.
Preoperative Evaluation and Preparation
The preoperative assessment includes a comprehensive evaluation by a multidisciplinary team: pulmonologists, thoracic surgeons, anesthesiologists, and physical therapists. Key steps include:
- Imaging: High-resolution CT scans to identify the most affected areas of the lung.
- Pulmonary Function Testing: To quantify the degree of lung impairment and the distribution of emphysema.
- Exercise Testing: To assess baseline exercise tolerance (e.g., six-minute walk test).
- Cardiac Evaluation: Echocardiography or stress testing to rule out significant heart disease.
- Smoking Cessation: Confirmed by urine or blood testing.
- Pulmonary Rehabilitation: A structured program to optimize physical conditioning and breathing techniques before surgery.
How Is LVRS Performed?
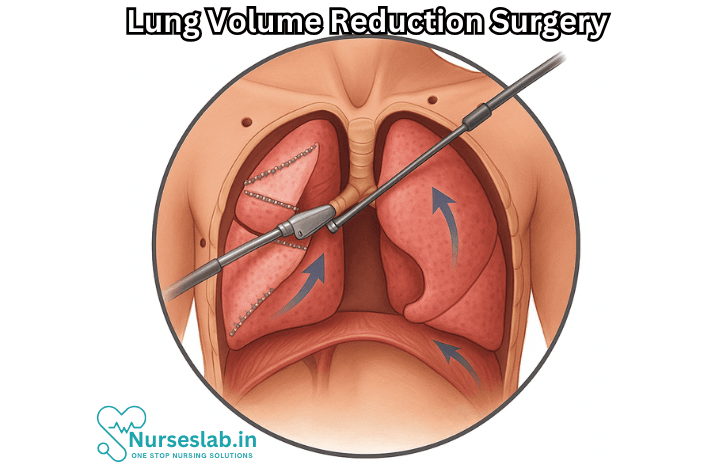
LVRS can be performed using two main approaches:
- Median Sternotomy: A traditional open-chest surgery where the breastbone is divided to allow access to both lungs. This approach is used when both lungs require intervention.
- Video-Assisted Thoracoscopic Surgery (VATS): A minimally invasive technique involving small incisions and the use of a thoracoscope (a camera-equipped instrument). VATS is associated with shorter hospital stays, less postoperative pain, and quicker recovery compared to open surgery.
During the procedure, surgeons remove about 20–30% of the most diseased, non-functioning lung tissue, usually from the upper lobes. The remaining lung tissue is re-expanded, and care is taken to minimize bleeding and air leaks. Sometimes, both lungs are treated in a single operation; in other cases, the procedure is staged.
Expected Benefits of LVRS
LVRS offers several potential benefits for carefully selected individuals:
- Improved Lung Function: Removal of hyperinflated, non-functioning tissue allows the healthier lung to expand and work more efficiently.
- Enhanced Exercise Capacity: Many patients experience significant improvements in their ability to walk, climb stairs, and perform daily activities.
- Reduction in Breathlessness: Shortness of breath often decreases, improving the quality of life and independence.
- Better Diaphragm Mechanics: The diaphragm, the main muscle of breathing, is less compressed after surgery and can function more effectively.
- Potentially Longer Survival: Clinical studies, such as the National Emphysema Treatment Trial (NETT), have shown a survival benefit among specific subgroups, particularly those with upper-lobe disease and low exercise capacity before surgery.
Risks and Complications
Like all major surgeries, LVRS carries certain risks. Complications are more likely in individuals with severe underlying illness. Possible adverse effects include:
- Prolonged Air Leaks: Persistent leakage of air from the lung can delay recovery and may require additional interventions.
- Infections: Surgical site infections or pneumonia may occur postoperatively.
- Bleeding: Rarely, significant bleeding may require blood transfusions or reoperation.
- Acute Respiratory Failure: Some patients may need mechanical ventilation for an extended period after surgery.
- Cardiac Complications: Heart attacks, arrhythmias, or heart failure may arise, especially in those with preexisting heart disease.
- Mortality: The risk of death within 30 days of surgery varies but is generally around 5–10% in large trials. Careful patient selection and modern surgical techniques have helped reduce this risk.
Recovery and Rehabilitation
Hospitalization after LVRS typically lasts from 7 to 14 days, depending on the individual’s progress and the occurrence of any complications. The early postoperative period involves:
- Pain management and monitoring for air leaks or infection
- Respiratory therapy to encourage deep breathing and prevent pneumonia
- Gradual reintroduction of physical activity under supervision
- Nutritional support to promote healing
After discharge, ongoing participation in pulmonary rehabilitation is essential. Such programs focus on building strength, endurance, and confidence, as well as providing education in breathing techniques, medication management, and lifestyle modifications.
Alternatives to LVRS
For those who are not candidates for LVRS, other treatment options include:
- Medical Therapy: Inhalers (bronchodilators, steroids), oxygen therapy, and medications to manage symptoms.
- Endobronchial Valves: Minimally invasive devices placed in the airways to block airflow to diseased lung segments, resulting in volume reduction similar to surgery.
- Pulmonary Rehabilitation: Structured exercise and education programs.
- Lung Transplant: In selected patients with end-stage lung disease and no other options, lung transplantation may be considered.
Long-Term Outcomes and Prognosis
Outcomes after LVRS depend on careful patient selection, the severity and distribution of emphysema, and adherence to postoperative care. Many patients experience improvements in lung function and quality of life for several years following surgery. However, emphysema is a progressive disease, and symptoms may eventually recur as remaining lung tissue continues to deteriorate.
Regular follow-up with pulmonology specialists, adherence to rehabilitation, and avoidance of smoking are critical for maintaining the benefits of the procedure.
Nursing Care of Patients Undergoing Lung Volume Reduction Surgery (LVRS)
Nursing care in the perioperative and postoperative periods is critical to achieving optimal outcomes, minimizing complications, and supporting patients through recovery.
Preoperative Nursing Care
Effective preoperative care forms the foundation for a successful surgical outcome. The period before surgery allows nurses to assess, educate, and prepare patients both physically and psychologically.
Patient Assessment
- Comprehensive Respiratory Assessment: Evaluate baseline respiratory function using spirometry, blood gas analysis, and physical examination.
- Nutritional Status: Assess for signs of malnutrition, which is common in advanced emphysema; collaborate with dietitians for nutritional optimization.
- Pulmonary Rehabilitation: Encourage participation in preoperative pulmonary rehabilitation to improve respiratory muscle strength and exercise tolerance.
- Medication Review: Review use of bronchodilators, corticosteroids, and other medications; ensure appropriate adjustment prior to surgery.
- Psychosocial Assessment: Identify anxiety, depression, or lack of social support; provide counseling and support services.
Patient and Family Education
- Explanation of Procedure: Use simple language to describe the LVRS process, expected outcomes, risks, and benefits.
- Preoperative Preparation: Instruct patients on fasting, medication adjustments, and what to expect in the operating room.
- Breathing Techniques: Teach incentive spirometry, pursed-lip breathing, and effective coughing techniques.
- Postoperative Expectations: Clarify anticipated pain, use of drains, oxygen therapy, and mobility restrictions.
- Family Involvement: Encourage active participation of family members in care planning and support activities.
Immediate Postoperative Nursing Care
The immediate postoperative period is vital for monitoring and managing complications. Nurses must be vigilant in assessment and prompt intervention.
Airway and Breathing Management
- Airway Patency: Maintain airway by monitoring for obstruction, prompt suctioning, and supportive positioning.
- Oxygen Therapy: Administer supplemental oxygen as ordered; monitor SpO2, aiming for target saturation based on individual needs.
- Ventilatory Support: Assist with noninvasive or invasive ventilation if required, and observe for signs of respiratory distress.
- Pulmonary Hygiene: Encourage deep breathing exercises, use of incentive spirometer, and gentle but regular chest physiotherapy.
- Monitoring for Pneumothorax: Watch for sudden changes in respiratory status that may indicate a pneumothorax, a common postoperative complication.
Pain Management
- Analgesia: Administer prescribed pain medications—opioids, nonsteroidal anti-inflammatory drugs (NSAIDs), or nerve blocks—as per orders.
- Pain Assessment: Regularly evaluate pain using visual analog scales and adjust management accordingly.
- Non-Pharmacological Interventions: Employ relaxation techniques, guided imagery, and positioning to alleviate discomfort.
Chest Drain Care
- Drain Management: Secure and monitor chest drains; document output, appearance, and ensure patency.
- Infection Prevention: Maintain strict aseptic technique during drain care and dressing changes.
- Education: Teach patient and family about function and purpose of chest drains, signs of complications, and care after removal.
Hemodynamic and Fluid Balance Monitoring
- Vital Signs: Perform frequent assessment of heart rate, blood pressure, respiratory rate, and temperature.
- Fluid Balance: Monitor intake and output closely; watch for signs of hypovolemia or fluid overload.
- Laboratory Surveillance: Monitor hemoglobin, hematocrit, electrolytes, and arterial blood gases as indicated.
Ongoing Postoperative and Rehabilitation Care
As patients move beyond the immediate postoperative phase, nursing care focuses on supporting rehabilitation, preventing complications, and facilitating return to daily life.
Early Mobilization
- Mobilization Plan: Collaborate with physical therapists to initiate gentle ambulation and mobility exercises, reducing risk of deep vein thrombosis and promoting lung expansion.
- Safety Precautions: Ensure fall prevention strategies are in place with assistance devices and frequent monitoring.
Pulmonary Rehabilitation
- Breathing Exercises: Reinforce use of incentive spirometers, diaphragmatic breathing, and coughing techniques.
- Exercise Tolerance: Gradually increase activity levels, monitoring for signs of fatigue, dyspnea, or hypoxemia.
- Education: Provide ongoing education regarding lifestyle modifications, energy conservation, and home oxygen therapy if needed.
Nutrition and Hydration
- Dietary Support: Continue collaboration with dietitians to optimize caloric intake, protein for healing, and hydration status.
- Appetite Stimulation: Address issues of poor appetite or nausea with appropriate interventions.
Infection Prevention
- Wound Care: Inspect surgical sites for redness, swelling, or drainage; maintain clean, dry dressings.
- Hand Hygiene: Reinforce strict hand hygiene for all caregivers, patients, and visitors.
- Antibiotic Stewardship: Administer prescribed prophylactic antibiotics and monitor for adverse reactions.
Psychosocial Support
- Emotional Wellbeing: Assess for anxiety, depression, and adjustment difficulties; facilitate access to counseling or support groups.
- Family Engagement: Involve family in education and care, preparing them for ongoing support needs at home.
- Coping Strategies: Empower patients with resources to manage the challenges of chronic illness and postoperative recovery.
Common Complications and Nursing Interventions
LVRS carries specific risks due to the underlying respiratory pathology and the nature of thoracic surgery. Vigilant nursing care is key to early identification and intervention.
Respiratory Complications
- Pneumothorax: Monitor for sudden dyspnea, decreased breath sounds, or subcutaneous emphysema; ensure swift medical intervention.
- Persistent Air Leak: Document the duration and volume of air leak; coordinate with surgeons regarding drain management.
- Pneumonia: Promote pulmonary hygiene and monitor for fever, increased sputum, or changes in breath sounds.
Cardiovascular Complications
- Arrhythmias: Observe for irregular heart rhythms; collaborate with medical team on management.
- Hypotension/Hypertension: Monitor closely and adjust fluid and medication therapy accordingly.
Other Complications
- Wound Dehiscence: Reinforce wound care education and monitor for separation of incision.
- Deep Vein Thrombosis: Encourage early mobilization, use compression devices, and administer anticoagulants as ordered.
- Delirium: Implement strategies for orientation, safety, and stimulation to reduce risk for postoperative confusion.
Discharge Planning and Long-Term Follow-Up
Discharge planning begins early and is central to sustained recovery.
Education for Self-Management
- Symptom Monitoring: Teach patients to recognize signs of respiratory distress, infection, or complications.
- Medication Adherence: Ensure understanding of prescribed medications, possible side effects, and importance of compliance.
- Activity Guidelines: Provide clear instructions for graded activity resumption and restrictions.
- Follow-Up Appointments: Stress importance of attending scheduled clinic visits for ongoing assessment and management.
Community Resources
- Home Health Services: Arrange for home nursing, physical therapy, and respiratory therapy as appropriate.
- Support Groups: Facilitate connection with peer support networks for continued education and encouragement.
REFERENCES
- DeCamp MM Jr, McKenna RJ Jr, Deschamps CC, Krasna MJ. Lung volume reduction surgery: technique, operative mortality, and morbidity.., https://pubmed.ncbi.nlm.nih.gov/18453353/ Proc Am Thorac Soc. 2008 May 1;5(4):442-6.
- Goldman L, et al., eds. Interventional and surgical approaches to lung disease. In: Goldman-Cecil Medicine. 27th ed. Elsevier; 2024. https://www.clinicalkey.com
- Nason KS, Ganim RB, Luketich JD. Chest Wall, Lung, Mediastinum, and Pleura. In: Brunicardi F, Andersen DK, Billiar TR, et al, eds. Schwartz’s Principles of Surgery. 11th ed. McGraw Hill; 2019.
- Criner GJ, et al. Multicenter RCT of Zephyr Endobronchial Valve Treatment in Heterogeneous Emphysema (LIBERATE). American Journal of Respiratory and Critical Care Medicine. 2018; doi:10.1164/rccm.201803-0590OC.
- Weaver H, Greening NJ, Rathinam S. Lung volume reduction surgery in patients with low diffusion capacity. https://pubmed.ncbi.nlm.nih.gov/30997185/J Thorac Dis. 2019 Mar;11(Suppl 3):S234-S236.
- Lee M, Sharma S, Mora Carpio AL. Lung Volume Reduction Surgery. [Updated 2024 Aug 11]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK559329/
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





