Introduction
Nephrectomy, the surgical removal of a kidney, stands as a vital procedure within the field of urology. Performed for a variety of reasons, nephrectomy can be life-saving or life-enhancing, depending on the patient’s condition. As kidneys are essential organs responsible for filtering waste from the blood, balancing fluids, and regulating blood pressure, the removal of one or both has significant medical implications.
What Is Nephrectomy?
Nephrectomy is derived from the Greek words “nephros” (kidney) and “ektome” (excision). It refers to the surgical removal of all or part of a kidney. Kidneys are bean-shaped organs located on either side of the spine, just below the rib cage. They play a crucial role in filtering blood, removing waste products through urine, and maintaining fluid and electrolyte balance.
There are two main forms of nephrectomy:
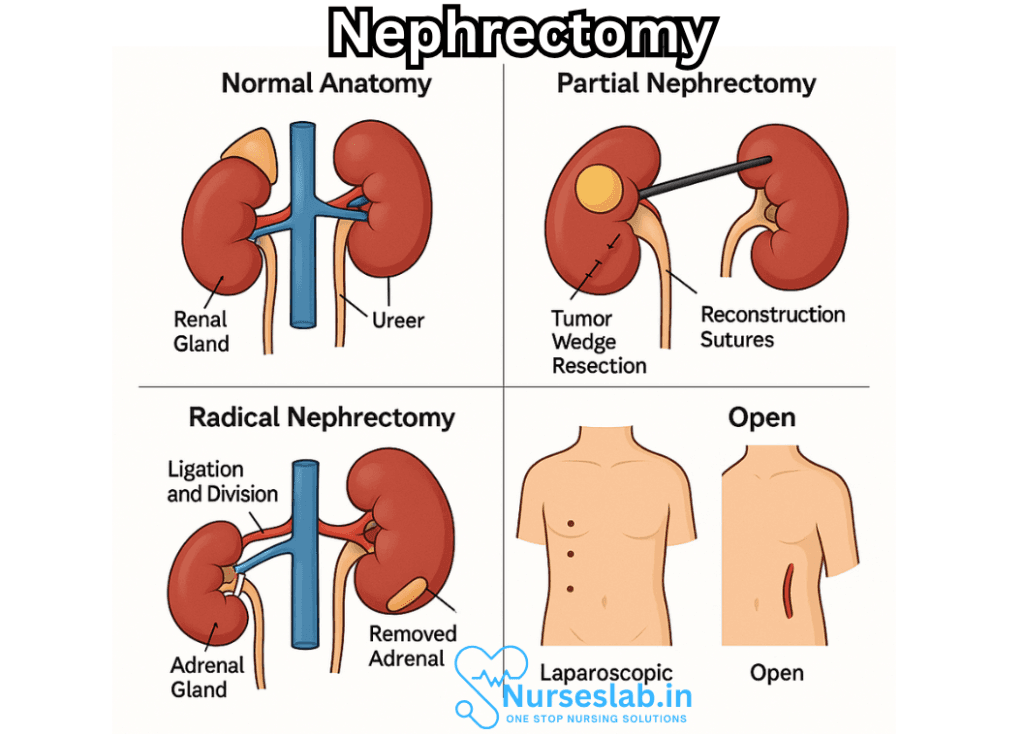
- Total (Radical) Nephrectomy: The entire kidney is removed, sometimes along with surrounding tissues such as the adrenal gland, a segment of the ureter, and nearby lymph nodes, depending on the disease’s extent.
- Partial Nephrectomy: Only the diseased or damaged portion of the kidney is excised, preserving as much healthy tissue as possible. This approach is favored when feasible, to maintain optimal kidney function.
Indications for Nephrectomy
The decision to remove all or part of a kidney is made with careful consideration of several possible indications, including:
- Renal Tumors: The most common reason for nephrectomy is the presence of kidney cancer, such as renal cell carcinoma. Large or malignant tumors often necessitate removal of the entire kidney to achieve cure.
- Benign Kidney Conditions: Non-cancerous growths, such as angiomyolipomas, may require nephrectomy if they cause symptoms, bleed, or have the potential for malignancy.
- Trauma: Severe injury to the kidney, often from accidents or penetrating wounds, may irreparably damage the organ, making nephrectomy necessary.
- Chronic Infection or Obstruction: Recurrent pyelonephritis (kidney infection), chronic hydronephrosis (swelling from urine build-up), or severe stone disease can render a kidney nonfunctional and prone to complications.
- Congenital Abnormalities: Birth defects, such as dysplastic or nonfunctioning kidneys, may be managed with nephrectomy, especially if they contribute to high blood pressure or infection.
- Kidney Donation: In living donor kidney transplantation, a healthy individual voluntarily undergoes a nephrectomy to provide a kidney for someone with end-stage renal disease.
Types of Nephrectomy Procedures
The approach to nephrectomy varies based on the patient’s diagnosis, overall health, and surgeon’s expertise. The main procedural types are:
Radical Nephrectomy
This procedure entails the removal of the entire kidney, surrounding fatty tissue, and sometimes the adrenal gland and adjacent lymph nodes. It is typically indicated for malignant tumors or conditions where cancer spread is possible.
Simple Nephrectomy
Only the kidney is removed without excising neighboring tissues. This method is usually reserved for non-cancerous diseases such as chronic infection or irreversible kidney damage.
Partial Nephrectomy (Nephron-Sparing Surgery)
This technique removes only the diseased segment, preserving as much healthy tissue as possible. It is preferred for small tumors, bilateral tumors, or patients with a single functioning kidney, as it helps maintain renal function.
Surgical Approaches
Advancements in surgical technology have revolutionized nephrectomy techniques, offering less invasive options and improved outcomes. The three primary approaches are:
- Open Nephrectomy: The traditional method, involving a large incision in the abdomen or flank to access and remove the kidney. This is necessary in complex cases or when tumors are large or invading surrounding structures.
- Laparoscopic Nephrectomy: Uses several small incisions, through which a camera and surgical instruments are inserted. The surgeon views the inside of the abdomen on a monitor and removes the kidney with minimal tissue disruption. Benefits include less pain, shorter hospital stays, and quicker recovery.
- Robotic-Assisted Laparoscopic Nephrectomy: A form of laparoscopic surgery where the surgeon controls robotic arms for greater precision and dexterity. This is particularly advantageous for delicate or complex partial nephrectomies.
Preparation for Nephrectomy
Proper preparation is essential for safety and optimal outcomes:
- Medical Evaluation: Comprehensive assessment includes blood tests, urine analysis, imaging (CT or MRI), and cardiac evaluation to ensure fitness for surgery.
- Medication Management: Certain medications, such as blood thinners, may need to be stopped before surgery to minimize bleeding risk.
- Fasting: Patients are generally instructed not to eat or drink for a specified period before the procedure.
- Counselling: Pre-operative discussions cover expectations, risks, and post-operative recovery, allowing patients and families to make informed decisions.
The Nephrectomy Procedure
Depending on the surgical approach, nephrectomy generally follows these broad steps:
- Anesthesia is administered, rendering the patient unconscious and pain-free.
- The surgeon makes the necessary incision(s) and carefully identifies the kidney and its blood supply.
- Blood vessels and the ureter (tube sending urine to the bladder) are clamped and divided.
- The kidney (and any additional tissue, if required) is removed.
- Hemostasis (control of bleeding) is achieved, and the surgical area is checked before closing the incisions.
- Drains may be placed to remove fluid and prevent collection at the surgical site.
The surgery duration typically ranges from 2 to 4 hours, depending on complexity.
Risks and Complications
As with any major surgery, nephrectomy carries risks:
- Bleeding: Significant blood loss may occur and sometimes require transfusion.
- Infection: Both surgical site and internal infections are possible.
- Damage to Surrounding Organs: The bowel, spleen, pancreas, liver, or blood vessels may be inadvertently injured.
- Blood Clots: Deep vein thrombosis or pulmonary embolism risk increases after surgery.
- Respiratory Complications: Pneumonia or breathing problems can occur, especially in patients with pre-existing lung conditions.
- Postoperative Pain: Discomfort is managed with pain medications and supportive care.
- Reduced Kidney Function: With one kidney remaining, there is less reserve; however, most people lead normal lives with a single healthy kidney.
Recovery After Nephrectomy
Postoperative recovery varies with the surgical approach and the patient’s overall health:
- Hospital Stay: Most patients remain in the hospital for 2 to 7 days. Laparoscopic or robotic procedures usually allow for faster discharge than open surgery.
- Pain Management: Pain control is a priority, with medications provided as needed.
- Wound Care: Patients must keep incisions clean and dry, monitoring for any signs of infection.
- Diet and Activity: Patients are often encouraged to move and walk soon after surgery, but strenuous activity is restricted for several weeks.
- Follow-Up: Regular check-ups and imaging assess for complications and monitor remaining kidney function.
Most people adjust well to living with one kidney, but lifelong attention to kidney health is essential.
Life After Nephrectomy
Adaptation to life with one kidney involves some lifestyle considerations:
- Hydration: Staying well-hydrated helps support kidney function, but excessive fluid intake should be avoided.
- Diet: A balanced diet low in salt and protein may be recommended to reduce kidney workload.
- Medication Use: Nonsteroidal anti-inflammatory drugs (NSAIDs) and certain antibiotics should be used with caution, as they may harm the remaining kidney.
- Regular Monitoring: Periodic blood pressure checks and kidney function tests are crucial for early detection of any issues.
Kidney donors typically enjoy normal life expectancy and quality of life, provided they remain vigilant about their health.
Advances and Future Directions
Innovations in surgical technology continue to improve nephrectomy outcomes:
- Minimally Invasive Techniques: Laparoscopic and robotic surgery have reduced pain, shortened hospital stays, and led to faster recoveries.
- Enhanced Imaging: Improved pre-operative imaging enables precise tumor localization and better preservation of healthy tissue.
- Personalized Medicine: Genetic testing and targeted therapies are increasingly guiding treatment choices for kidney cancer.
Ongoing research seeks to further minimize surgical trauma and maximize post-surgical quality of life.
Nursing Care of Patients Undergoing Nephrectomy
The nursing management of individuals post-nephrectomy—whether for malignancy, trauma, or other renal pathology—demands specialised attention across the perioperative continuum. As with neobladder reconstruction, the nurse’s role is multidimensional, encompassing vigilant clinical assessment, patient-centred education, and holistic support.
Preoperative Preparation
- Patient Assessment: Conduct baseline evaluations, including vital signs, renal function tests, and assessment of comorbidities.
- Education: Inform the patient and family about the surgical procedure, expected postoperative course, pain management strategies, and the potential impact on lifestyle and renal function.
- Emotional Support: Address anxieties and misconceptions, encouraging questions and involving caregivers as appropriate, all while maintaining respect for patient autonomy and privacy.
Immediate Postoperative Care
- Monitoring: Closely observe vital signs, urine output, and fluid balance to detect early signs of hemorrhage, shock, or acute kidney injury in the remaining kidney.
- Pain Management: Administer prescribed analgesics and assess efficacy, adapting interventions to individual pain thresholds.
- Wound Care: Inspect the surgical site regularly for signs of infection, dehiscence, or hematoma, and maintain sterile dressing changes.
- Prevention of Complications: Implement measures to reduce the risk of respiratory issues (encourage deep breathing and coughing exercises), venous thromboembolism (early mobilisation, compression devices), and gastrointestinal disturbances (monitor for ileus, provide dietary guidance).
Ongoing Assessment and Support
- Renal Function Surveillance: Regularly monitor laboratory parameters such as serum creatinine, BUN, and electrolytes to assess the function of the remaining kidney.
- Fluid and Electrolyte Management: Adapt fluid therapy based on individual needs and medical advice, watching for signs of overload or dehydration.
- Patient Education: Teach the patient about signs and symptoms of complications (e.g., fever, hematuria, decreased urine output), the importance of medication adherence, and strategies to protect the solitary kidney (e.g., avoiding nephrotoxic drugs, staying well hydrated).
- Lifestyle Modification: Provide guidance on diet, activity level, and infection prevention, encouraging regular follow-up visits and communication with the healthcare team.
Psychosocial and Holistic Care
- Emotional Wellbeing: Recognise and address psychological responses such as anxiety, body image concerns, or fear of recurrence, offering referrals to counselling or support groups as needed.
- Family and Caregiver Involvement: Include significant others in education and care planning when appropriate, always upholding the patient’s wishes and confidentiality.
In summary, nursing care for the nephrectomy patient is rooted in proactive assessment, patient empowerment, and collaboration within the multidisciplinary team. By combining technical proficiency with empathy and advocacy, nurses play a pivotal role in supporting optimal recovery, preserving renal health, and fostering long-term wellbeing.
REFERENCES
- American Cancer Society. Surgery for Kidney Cancer. https://www.cancer.org/cancer/types/kidney-cancer/treating/surgery.html. Last revised 5/1/2024.
- Klaassen Z, Kohut RM Jr, Patel D, Terris MK, Madi R. A single surgeon’s experience with open, laparoscopic, and robotic partial nephrectomy. Int Sch Res Notices. 2014;2014:430914. doi:10.1155/2014/430914
- National Institute of Diabetes and Digestive and Kidney Diseases (U.S.). Solitary or Single-Functioning Kidney. https://www.niddk.nih.gov.Last reviewed 10/2020.
- Bhat S. Role of surgery in advanced/metastatic renal cell carcinoma. Indian J Urol. 2010;26(2):167-176. doi:10.4103/0970-1591.65381
- National Kidney Foundation (U.S.). Nephrectomy. https://www.kidney.org/atoz/content/nephrectomy. Last reviewed 7/2009.
- National Library of Medicine (U.S.). Kidney Removal. https://medlineplus.gov/ency/article/003001.htm. Last reviewed 1/1/2023.
- Bishoff JT, et al., eds. Nephrectomy. In: Atlas of Laparoscopic and Robotic Urologic Surgery. 4th ed. Elsevier; 2023.
- Tantisattamo E, Dafoe DC, Reddy UG. Current Management of Patients with Acquired Solitary Kidney. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6732776/. Kidney Int Rep. 2019 Jul 11;4(9):1205-1218.
- Zaid HB, et al. Outcomes following complete surgical metastasectomy for patients with metastatic renal cell carcinoma: A systematic review and meta-analysis. The Journal of Urology. 2017; doi:10.1016/j.juro.2016.07.079.
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





