An In-Depth Exploration of a Lifesaving Medical Advancement
Introduction
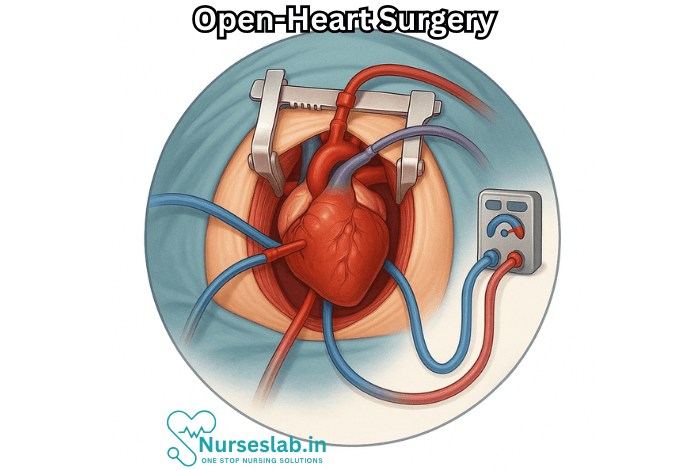
Open-heart surgery stands as one of the pinnacles of modern medicine—a procedure that has saved countless lives and transformed our understanding of cardiac care. It is both a testament to human ingenuity and a direct confrontation with the complexities of the human heart. Through open-heart surgery, surgeons access the heart by opening the chest wall, enabling them to repair or replace structures that, worn by age or damaged by disease, threaten the very core of life.
Defining Open-Heart Surgery
Open-heart surgery is a broad term encompassing any surgical procedure in which the chest is opened and surgery is performed on the heart’s internal structures. Most commonly, open-heart surgery refers to operations that require the use of a heart-lung machine (cardiopulmonary bypass). This sophisticated device temporarily takes over the function of the heart and lungs during surgery, allowing surgeons to operate in a bloodless and motionless field.
Common Procedures Included
- Coronary Artery Bypass Grafting (CABG): The most frequent type of open-heart surgery, CABG is performed to reroute blood around clogged arteries, improving blood flow and oxygen to the heart muscle.
- Heart Valve Repair or Replacement: Surgeons fix or replace faulty valves that regulate the flow of blood through the heart’s chambers.
- Repair of Congenital Heart Defects: Structural defects present from birth, such as atrial or ventricular septal defects, are corrected via open-heart techniques, often in infants or children.
- Heart Transplantation: In cases of severe, irreversible heart failure, a diseased heart is replaced with a healthy donor organ.
A Brief History of Open-Heart Surgery
The journey toward open-heart surgery has been marked by bold experimentation, heartbreak, and triumphant innovation. The first successful open-heart operation is credited to Dr. John Gibbon in 1953, when he used a heart-lung machine to repair a heart defect. Before this revolutionary device, surgeons were limited to procedures on the surface of the heart or had to operate within a few minutes, as blood flow and oxygenation could not be safely interrupted for long.
Milestones
- 1953: Dr. John Gibbon performs the first successful open-heart surgery using a heart-lung machine.
- 1967: The first human heart transplant is performed by Dr. Christiaan Barnard in South Africa.
- 1970s-1980s: Advancements in valve prosthetics and coronary artery bypass techniques expand the range and success of heart surgeries.
- Recent Decades: Minimally invasive and robotic-assisted heart surgeries begin to emerge, further reducing risk and recovery time.
The Surgical Process
Undergoing open-heart surgery is a profound experience, requiring careful planning and coordination among multidisciplinary medical teams.
Preoperative Preparation
Patients are thoroughly evaluated through physical examinations, blood tests, imaging studies (such as echocardiograms and angiograms), and consultations. Risk factors—including age, overall health, and the specific heart condition—are considered. Instructions are provided regarding medication adjustments, fasting, and hospital admission.
Operation Day
The procedure typically begins with the administration of general anesthesia, rendering the patient unconscious and pain-free. The surgeon makes an incision down the middle of the chest, cutting through the sternum to access the heart. The patient is then connected to the heart-lung machine, which circulates and oxygenates blood while the heart is temporarily stopped.
Depending on the surgery’s purpose, the surgeon might:
- Bypass blocked arteries using grafts made from veins or arteries taken elsewhere in the body.
- Replace diseased valves with synthetic or biological prosthetics.
- Repair congenital defects, such as holes in the heart walls.
- Remove the diseased heart and implant a donor organ.
After the operation, the heart is restarted, the patient is disconnected from the heart-lung machine, and the chest is closed with wires and sutures. The patient is then moved to intensive care for close monitoring.
Recovery and Rehabilitation
The road to recovery from open-heart surgery can be challenging but rewarding. Patients typically spend several days in the intensive care unit, followed by additional hospitalization. Pain management, infection prevention, and monitoring for complications such as arrhythmias or bleeding are priorities.
Physical rehabilitation begins soon after surgery, with gentle movement and breathing exercises. A structured cardiac rehabilitation program, overseen by healthcare professionals, helps patients regain strength, endurance, and confidence. Most individuals resume daily activities within six to twelve weeks, though full recovery may take several months.
Risks and Complications
Like all major surgeries, open-heart procedures carry risks. The most common complications include:
- Bleeding
- Infection
- Arrhythmias (Irregular Heartbeats)
- Stroke
- Kidney Failure
- Lung Problems
Certain factors, such as advanced age, underlying health conditions, and emergency procedures, can increase the risk. Nevertheless, improvements in surgical techniques, anesthesia, and postoperative care have dramatically increased the safety and success of open-heart surgeries.
The Emotional Journey
Beyond the physical challenge, open-heart surgery is an emotional journey for patients and their loved ones. The prospect of major surgery can evoke fear, anxiety, and uncertainty, but it also brings hope—hope for a renewed life, free from the constraints of heart disease.
Counseling and support groups offer valuable resources for emotional recovery. Many patients report a newfound appreciation for life and a commitment to healthier habits after their experience.
Nursing Care of Patients Undergoing Open-Heart Surgery
Open-heart surgery represents one of the most complex and invasive procedures in modern medicine, often performed to correct congenital or acquired cardiac defects, replace or repair heart valves, or to bypass blocked coronary arteries. The role of nursing care in the perioperative and postoperative phases is paramount for patient safety, optimal recovery, and long-term well-being.
Preoperative Nursing Care
Patient Assessment and Preparation
- Comprehensive Assessment: Conduct a thorough physical and psychological assessment, including vital signs, cardiovascular status, respiratory function, renal function, neurologic status, and laboratory values.
- Education: Provide information regarding the surgical procedure, expected outcomes, risks, and the recovery process. Address patient and family concerns, and clarify misconceptions to relieve anxiety.
- Preoperative Instructions: Advise on fasting, medication adjustments, and skin preparation. Ensure that consent forms are signed and necessary diagnostic tests are completed.
- Emotional Support: Offer reassurance and psychological support. Anxiety is common; establish trust and encourage expression of fears and expectations.
Preoperative Interventions
- Infection Prevention: Administer prophylactic antibiotics as ordered and ensure proper aseptic techniques.
- Medication Management: Review and manage anticoagulants, antiplatelets, or other relevant medications as per physician’s orders.
- Preparation for Anesthesia: Coordinate with anesthesiology for assessment and preparation, including airway evaluation and intravenous access establishment.
Intraoperative Nursing Responsibilities
Operating Room Preparation
- Ensure all necessary equipment and supplies are available and functioning, including cardiac monitors, defibrillators, and surgical instruments.
- Assist in patient positioning to avoid pressure injuries and facilitate optimal surgical access.
Patient Safety and Monitoring
- Monitor patient’s vital signs, oxygen saturation, and electrocardiogram (ECG) continuously.
- Support the surgical team in maintaining sterile technique throughout the procedure.
- Document intraoperative events, medications administered, and any deviations from expected course.
Immediate Postoperative Care (ICU Phase)
After open-heart surgery, patients are transferred to the intensive care unit (ICU) for close monitoring and support.
Assessment and Monitoring
- Hemodynamic Stability: Monitor blood pressure, heart rate, central venous pressure, pulmonary artery wedge pressure, and cardiac output.
- Respiratory Support: Most patients will be mechanically ventilated initially; monitor airway patency, ventilator settings, and blood gases. Perform regular suctioning and chest physiotherapy as needed.
- Fluid and Electrolyte Balance: Monitor input and output meticulously. Watch for signs of fluid overload, dehydration, or electrolyte imbalances (especially potassium, calcium, and magnesium).
- Neurologic Status: Assess level of consciousness, pupillary response, and motor function to detect early signs of cerebral complications.
Pain Management
- Assess pain using standardized scales and administer analgesics as prescribed.
- Encourage non-pharmacologic pain relief methods, such as relaxation techniques and positioning.
Infection Control
- Monitor incision site for signs of infection: redness, swelling, warmth, discharge.
- Follow strict aseptic technique when handling invasive lines, catheters, and drains.
- Administer antibiotics as ordered and educate patient/family on infection signs.
Prevention of Complications
- Bleeding: Observe chest tube output, vital signs, and hemoglobin/hematocrit levels. Be alert for excessive bleeding and notify the surgical team promptly.
- Thromboembolism: Employ sequential compression devices, encourage early mobilization, and administer anticoagulants as ordered.
- Arrhythmias: Monitor cardiac rhythm continuously. Treat arrhythmias according to protocol and notify the physician of any significant changes.
- Renal Dysfunction: Monitor urine output, renal function tests, and intervene early in cases of oliguria or rising creatinine.
Early Postoperative Care (General Ward)
Once stabilized, the patient is transferred to a cardiac surgical ward.
Ongoing Assessment
- Continue to monitor vital signs, cardiac rhythm, and oxygen saturation regularly.
- Assess wound healing and manage dressings as per protocol.
- Monitor for signs of complications such as pericardial tamponade, pneumonia, deep vein thrombosis, or wound dehiscence.
Mobility and Rehabilitation
- Encourage early, supervised ambulation to promote circulation, prevent thrombosis, and support lung function.
- Collaborate with physiotherapists for individualized rehabilitation plans including breathing exercises, limb exercises, and progressive mobilization.
Nutritional Support
- Assess nutritional status and create a plan for adequate caloric and protein intake to support healing.
- Address swallowing difficulties and dietary restrictions as needed.
Psychological Support
- Continue to provide emotional support to patients and their families.
- Offer counseling and connect with support groups if anxiety, depression, or adjustment difficulties arise.
Discharge Planning and Education
The transition from hospital to home is critical and requires thorough preparation.
Patient and Family Education
- Instruct on wound care, signs of infection, medication regimen, follow-up appointments, and when to seek medical help.
- Educate about lifestyle modifications, including diet, exercise, stress management, and cessation of smoking and alcohol.
- Provide resources for cardiac rehabilitation programs and community support.
Medication Management
- Teach patients the purpose, dosage, side effects, and schedule of each prescribed medication (anticoagulants, antihypertensives, diuretics, etc.).
- Emphasize the importance of adherence and regular monitoring of blood pressure, glucose, and INR as applicable.
Activity Guidelines
- Advise on restrictions regarding heavy lifting, driving, sexual activity, and participation in strenuous activities until cleared by the healthcare provider.
- Encourage gradual increase in activities according to tolerance and recovery progress.
Long-Term Follow-Up and Support
Outpatient Care
- Arrange for regular follow-up visits to monitor for late complications such as arrhythmias, heart failure, or prosthetic valve dysfunction.
- Encourage ongoing participation in cardiac rehabilitation and support groups.
- Reassess psychosocial adjustment and offer counseling as needed.
Special Considerations
Care of Elderly Patients
- Assess and address age-related concerns such as frailty, cognitive impairment, and polypharmacy.
- Work closely with family caregivers and provide tailored education and support.
Pediatric Open-Heart Surgery
- Adapt interventions to developmental stage and family context.
- Provide play therapy, age-appropriate education, and family-centered care.
REFERENCES
- American Heart Association. Congenital Heart Defects Surgery. https://www.heart.org/en/health-topics/congenital-heart-defects/care-and-treatment-for-congenital-heart-defects/congenital-heart-defects-surgery. Last reviewed 9/19/2023.
- American Heart Association. Heart Procedures and Surgeries. https://www.heart.org/en/health-topics/heart-attack/treatment-of-a-heart-attack/cardiac-procedures-and-surgeries. Last reviewed 10/6/2023.
- American Society of Anesthesiologists. Heart Surgery. https://www.asahq.org/madeforthismoment/preparing-for-surgery/procedures/heart-surgery/.
- National Heart, Lung and Blood Institute (U.S.) What Is Heart Surgery?. https://www.nhlbi.nih.gov/health/heart-surgery Last updated 6/1/2022.
- The Society of Thoracic Surgeons. After Heart Surgery. https://ctsurgerypatients.org/before-during-and-after-surgery/after-heart-surgery. Last reviewed 5/2017.
- Heart surgery. (2024).
https://www.asahq.org/madeforthismoment/preparing-for-surgery/procedures/heart-surgery/
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





