Introduction
Open Reduction and Internal Fixation (ORIF) is a cornerstone procedure in the field of orthopedic surgery, employed to treat complex fractures that cannot be managed by conservative means such as casting or splinting alone. The goal of ORIF is to restore anatomical alignment, ensure stability, and promote early mobilization, thereby optimizing the chances for full functional recovery.
Understanding Fractures and the Need for ORIF
Fractures, or breaks in the continuity of bone, can result from trauma, overuse, or pathological weakening of bone tissue. While many fractures are effectively managed with non-operative treatments, certain patterns—such as displaced, comminuted, intra-articular, or open fractures—necessitate surgical intervention. ORIF is indicated when closed reduction (manipulation without incisions) fails to achieve or maintain satisfactory alignment or when stable fixation cannot be achieved otherwise.
Indications for ORIF
- Displaced fractures: Bones are misaligned and cannot be corrected non-surgically.
- Comminuted fractures: The bone is broken into several fragments.
- Intra-articular fractures: The break extends into a joint surface.
- Open fractures: The bone breaks through the skin, increasing infection risk.
- Non-union or malunion: Previous attempts at healing have failed, or bones have healed in poor alignment.
- Fractures associated with neurovascular compromise.
The Principles of ORIF
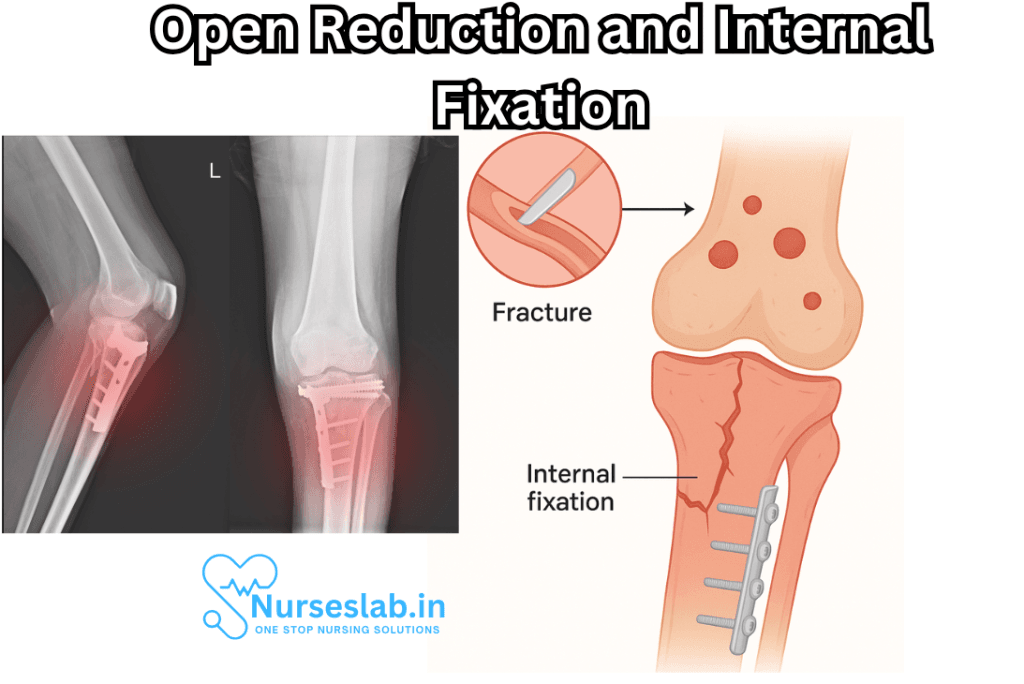
ORIF adheres to the core tenets of fracture management: anatomical reduction, stable fixation, preservation of blood supply, and early mobilization. The procedure involves two main components:
- Open Reduction: Surgically exposing the fracture site to allow direct visualization and manipulation of the bone fragments.
- Internal Fixation: The use of implants such as plates, screws, rods, or wires to stabilize the fracture internally, maintaining the reduction until healing occurs.
Surgical Procedure: Step-by-Step
The ORIF process is a carefully orchestrated surgical event, typically performed under general or regional anesthesia by a specialized orthopedic team.
1. Preoperative Planning
Proper planning is vital for successful outcomes. Surgeons assess the fracture through physical examination, X-rays, CT scans, or MRI to determine the fracture type, location, and complexity. Preoperative planning also includes choosing the most appropriate approach, fixation method, and implant.
2. Patient Positioning and Preparation
The patient is positioned on the operating table to allow optimal access to the fracture site. The area is sterilized, and drapes are applied to create a sterile field.
3. Incision and Exposure
An incision is made over the fracture site. Soft tissues, including skin, subcutaneous layers, and muscle, are carefully retracted to minimize damage and preserve blood supply.
4. Open Reduction
With direct visualization, the surgeon realigns the bone fragments to their anatomical position. Temporary fixation devices, such as bone clamps or pins, may be used to hold the reduction.
5. Internal Fixation
Once proper alignment is confirmed, internal fixation devices—plates, screws, rods, or wires—are applied to hold the bone segments securely in place. The choice of device depends on the bone involved, the fracture pattern, and patient-specific factors.
6. Wound Closure
After achieving stable fixation, the surgical site is irrigated, and the layers of soft tissue are closed sequentially. Sterile dressings are applied.
7. Postoperative Care
Postoperative protocols include pain management, antibiotics to prevent infection, and anticoagulation if necessary to prevent blood clots. Neurovascular status is closely monitored.
Types of Internal Fixation Devices
- Plates and Screws: Commonly used for long bone fractures, they provide strong, rigid fixation.
- Intramedullary Rods (Nails): Inserted into the marrow canal of long bones, suitable for femur, tibia, and humerus fractures.
- Wires and Pins: Used for smaller bones or as adjuncts in complex fractures.
- Specialized Devices: Locking plates, bioabsorbable implants, and external fixators for unique indications.
Benefits of ORIF
ORIF offers several advantages over non-surgical management, especially in complex fractures:
- Restores normal anatomy and joint function.
- Provides stable fixation, enabling early movement and reducing the risk of joint stiffness or muscle atrophy.
- Improves chances for complete healing and functional recovery.
- Reduces the risk of non-union, malunion, and long-term disability.
Potential Risks and Complications
Like all surgeries, ORIF carries risks, and patients must be informed about possible complications:
- Infection: Despite sterile techniques, there is always some risk of infection at the surgical site.
- Neurovascular Injury: Nerves or blood vessels may be injured during the procedure.
- Implant-related Problems: Implants can fail, loosen, or cause irritation, sometimes necessitating removal.
- Non-union or Delayed Union: The bone may heal slowly or not at all.
- Joint Stiffness or Loss of Motion: May result if postoperative rehabilitation is inadequate.
- Blood Clots: Deep vein thrombosis (DVT) or pulmonary embolism may occur, particularly in lower limb surgeries.
- Allergic Reactions: Rarely, patients may react to metal implants.
Recovery and Rehabilitation
Successful ORIF is not simply about the surgical procedure; postoperative rehabilitation is crucial to restoring function. The recovery timeline depends on multiple factors, including the bone involved, patient age, health status, and adherence to rehab protocols.
Early Rehabilitation
Immediately following surgery, physical therapists engage the patient in gentle movements to prevent joint stiffness and maintain circulation. Weight-bearing status depends on the stability of the fixation and the specific bone fractured. Pain and swelling are managed with medication, elevation, and ice.
Progressive Strengthening
As healing progresses, therapy focuses on restoring range of motion, strengthening muscles, and gradually increasing activity levels. The duration and intensity of rehabilitation are individualized.
Return to Normal Activities
Most patients can expect to return to light daily activities within several weeks, but full recovery for complex fractures may take months. High-impact activities and sports are typically delayed until full bone healing is confirmed via imaging.
Outcomes and Prognosis
When performed appropriately, ORIF has a high success rate, enabling patients to regain normal limb function and quality of life. The prognosis is generally favorable, especially when surgery is timely and followed by structured rehabilitation. Factors that may influence outcomes include:
- Patient age and general health
- Severity and location of the fracture
- Presence of comorbidities (e.g., diabetes, osteoporosis)
- Adherence to rehabilitation protocols
Special Considerations and Advances
Recent advances in orthopedic technology have improved both the safety and the outcomes of ORIF. Minimally invasive techniques, computer-assisted surgery, and custom-designed implants are becoming increasingly common. Bioabsorbable fixation devices and biologic agents to enhance bone healing are also areas of active research.
Special populations—such as pediatric or geriatric patients—require tailored approaches. Children have remarkable bone healing capacity, allowing for less rigid fixation and faster remodeling. In older adults, bone quality, healing potential, and risks of surgery must be carefully weighed.
Nursing Care for Patients Undergoing Open Reduction and Internal Fixation (ORIF)
Preoperative Nursing Care
- Patient Education: Provide clear explanations about the ORIF procedure, expected outcomes, and potential risks to alleviate anxiety and facilitate informed consent.
- Baseline Assessment: Perform thorough assessments of neurovascular status, pain level, skin integrity, and functional mobility. Document findings for postoperative comparison.
- Preparation for Surgery: Ensure preoperative protocols are completed, such as fasting, skin preparation, removal of jewellery, and verification of allergies. Encourage deep breathing and coughing exercises to minimise postoperative pulmonary complications.
Immediate Postoperative Care
- Airway, Breathing, Circulation (ABC): Monitor vital signs closely, observe for early signs of shock or respiratory compromise, and maintain airway patency.
- Pain Management: Administer prescribed analgesics promptly. Assess pain using standardised tools and employ adjunctive methods such as positioning, ice packs, and relaxation techniques.
- Neurovascular Checks: Frequently assess the operated limb for colour, warmth, capillary refill, movement, sensation, and pulses. Promptly report any signs of compromised circulation or nerve injury.
- Wound Care: Inspect the surgical site for bleeding, swelling, or discharge. Maintain a sterile dressing and monitor for signs of infection.
- Drain and Device Management: Monitor drains, traction, or external devices if present, ensuring correct function and patency.
Ongoing Nursing Management
- Early Mobilisation: Collaborate with physiotherapists to initiate safe mobilisation as soon as permitted, preventing complications such as deep vein thrombosis (DVT) or muscle atrophy.
- Thromboprophylaxis: Administer anticoagulants as prescribed and encourage leg exercises, compression stockings, and adequate hydration to reduce DVT risk.
- Pressure Injury Prevention: Reposition regularly, protect pressure points, and assess skin integrity to minimise the risk of pressure ulcers.
- Nutrition and Hydration: Support optimal healing by encouraging a balanced diet rich in protein, vitamins, and minerals, and ensure adequate fluid intake.
- Patient and Family Teaching: Instruct on limb care, signs of complications (e.g., infection, hardware failure), medication management, and rehabilitation exercises. Prepare for discharge by providing written information and emergency contact details.
Psychosocial and Long-Term Considerations
- Coping and Adjustment: Support emotional adjustment to temporary or permanent changes in function. Offer psychological support and referrals as needed.
- Rehabilitation Support: Encourage adherence to physiotherapy and occupational therapy regimens to maximise postoperative recovery and functional independence.
- Follow-Up Care: Arrange for follow-up appointments, radiological assessments, and ongoing evaluation of the surgical site and limb function.
With dedicated, patient-centred nursing care, individuals undergoing ORIF can achieve optimal recovery, reduced complications, and improved quality of life.
REFERENCES
- American Academy of Orthopaedic Surgeons. Fractures (Broken Bones). https://orthoinfo.aaos.org/en/diseases–conditions/fractures-broken-bones/. Last reviewed 8/2021
- Rasouli MR, et al. (2015). Hardware removal due to infection after open reduction and internal fixation: Trends and predictors.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4507072/ - American Academy of Orthopaedic Surgeons. Internal Fixation for Fractures. https://orthoinfo.aaos.org/en/treatment/internal-fixation-for-fractures/. Last reviewed 4/2019.
- Amin TK, Patel I, Patel MJ, et al. Evaluation of Results of Open Reduction and Internal Fixation (ORIF) of Fracture of Distal End of Femur with Intra-Articular Extension. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8667249/. Malays Orthop J. 2021;15(3):78-83.
- Open reduction and internal fixation (ORIF) [Fact sheet]. (2012).
https://intermountainhealthcare.org/ext/Dcmnt?ncid=521402750 - AO Surgery Reference. Intramedullary nailing. https://surgeryreference.aofoundation.org/orthopedic-trauma/adult-trauma/tibial-shaft/simple-fracture-oblique/intramedullary-nailing.
- Merck Manual, Professional Version. Overview of Fractures. https://www.merckmanuals.com/professional/injuries-poisoning/fractures/overview-of-fractures. Last reviewed 12/2022.
- National Library of Medicine (U.S.). Broken bone. https://medlineplus.gov/ency/article/000001.htm. Last updated 2/8/2024.
- Smith KS, Drexelius K, Challa S, et al. Outcomes Following Ankle Fracture Fixation With or Without Ankle Arthroscopy. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8697299/. Foot Ankle Orthop. 2020;5(1):2473011420904046. Published 2020 Mar 2.
- Oh CH, Jang I, Ha C, Hong IT, Jeong S, Han SH. Open Reduction and Internal Fixation of Distal Radius Fractures with Complete Intra-articular Involvement and Diaphyseal Extension. Clin Orthop Surg. 2024 Dec;16(6):979-986.
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





