An In-Depth Exploration of Photodynamic Therapy in Modern Medicine
Photodynamic Therapy (PDT) is an innovative, minimally invasive medical treatment that harnesses the power of light-sensitive compounds to treat a variety of conditions, particularly certain types of cancer and skin disorders. Over the past decades, PDT has emerged as a vital tool in the therapeutic arsenal of dermatologists, oncologists, and ophthalmologists, offering targeted treatment with limited side effects.
What Is Photodynamic Therapy?
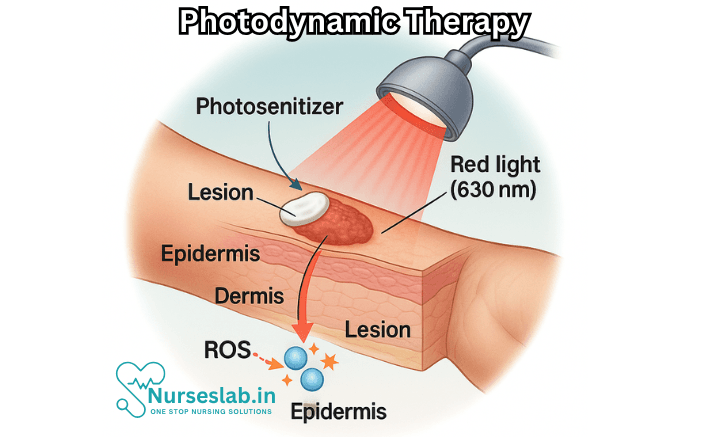
Photodynamic Therapy is a two-stage treatment that combines a photosensitizing agent—a special drug that responds to light—with a specific wavelength of light to destroy abnormal cells. The therapy is based on the principle that certain chemicals can be activated by light energy to produce reactive oxygen species capable of damaging cellular components, ultimately leading to the death of targeted cells.
Historical Background
Although the foundation of photodynamic therapy lies in modern scientific advances, the therapeutic use of light dates back to ancient civilizations. The Egyptians, Greeks, and Indians recognized the healing properties of sunlight. The modern concept of PDT, however, began in the early 20th century with the discovery that certain dyes could sensitize cells to light. In the 1970s, researchers began to realize the clinical potential of this approach, leading to the development of drugs such as Photofrin and the formalization of treatment protocols.
How Photodynamic Therapy Works
PDT involves three essential components:
- Photosensitizer: A drug that is administered systemically (e.g., intravenously) or topically and accumulates preferentially in diseased cells.
- Light Source: A specific wavelength of light (often red or blue) that matches the absorption spectrum of the photosensitizer.
- Oxygen: Cells must be well-oxygenated, as oxygen is required for the generation of reactive oxygen species (ROS), which mediate cytotoxicity.
After the photosensitizer is administered and enough time has passed for it to concentrate in target tissues and clear from healthy tissues, the affected area is exposed to light. This activates the drug, triggering a photochemical reaction that generates singlet oxygen and other ROS, damaging cell membranes, organelles, and DNA. The result is targeted cell death, inflammation, and in some cases, an immune response against the diseased tissue.
Types of Photosensitizers
The efficacy of PDT depends heavily on the properties of the photosensitizer used. There are three generations of photosensitizers:
- First-generation: These include porphyrin-based compounds such as Photofrin. They are effective but have limitations, such as prolonged skin photosensitivity and limited tissue penetration.
- Second-generation: These include agents like temoporfin and aminolevulinic acid (ALA). They offer improved selectivity, reduced side effects, and better absorption of light in deeper tissues.
- Third-generation: These are under development and involve molecular modifications, targeted delivery strategies (such as antibody conjugates or nanoparticles), and dual-acting agents designed for enhanced efficacy and safety.
Clinical Applications of Photodynamic Therapy
PDT has been studied and applied in several medical fields. Its most prominent applications include:
1. Cancer Treatment
Photodynamic therapy is used to treat various malignancies, particularly those accessible to light. Approved indications include:
- Superficial and early-stage skin cancers (basal cell carcinoma, squamous cell carcinoma in situ).
- Esophageal cancer.
- Non-small cell lung cancer (for endobronchial tumors).
- Bladder cancer.
- Head and neck cancers.
In cancer therapy, PDT destroys tumor cells directly, damages tumor vasculature, and stimulates anti-tumor immunity.
2. Dermatological Disorders
PDT is widely used in dermatology for benign and pre-cancerous conditions, such as:
- Actinic keratosis (precancerous skin lesions caused by sun damage).
- Bowen’s disease (squamous cell carcinoma in situ).
- Acne vulgaris (by targeting sebaceous glands and bacteria).
- Psoriasis and other inflammatory skin disorders (under investigation).
The combination of topical photosensitizers and non-invasive light sources make PDT an attractive option for patients seeking alternatives to surgery or systemic therapy.
3. Ophthalmology
PDT has a vital role in the treatment of age-related macular degeneration (AMD), especially for the wet form characterized by abnormal blood vessel growth. Verteporfin, a photosensitizer, is injected intravenously and activated by a laser to selectively destroy these vessels, helping to preserve vision.
4. Antimicrobial and Dental Applications
The photodynamic action that damages human cells is equally effective against bacteria, fungi, and viruses. PDT, therefore, is being explored for:
- Treatment of localized infections, including antibiotic-resistant bacteria.
- Dental plaque and periodontal diseases.
Advantages of Photodynamic Therapy
PDT offers several benefits over traditional therapies:
- Minimally invasive: Most procedures do not require incisions or general anesthesia.
- Targeted treatment: The combination of selective drug uptake and local light exposure minimizes damage to healthy tissues.
- Repeatable: PDT can be repeated multiple times at the same site, unlike radiation therapy, which has limits due to cumulative toxicity.
- Minimal systemic effects: Most side effects are local and temporary, such as redness, swelling, and sensitivity to light.
- Low scarring risk: Particularly for skin conditions, PDT leaves minimal scarring compared to surgery.
Limitations and Side Effects
Despite its many advantages, PDT is not without challenges:
- Light penetration: The effectiveness of PDT is limited by the depth to which light can penetrate tissue. This restricts its use mainly to surface lesions or those accessible via endoscopes or catheters.
- Photosensitivity: Patients may experience heightened sensitivity to light for days or weeks following treatment, necessitating precautions to avoid sunburn or skin damage.
- Incomplete response: Not all lesions respond fully, and some may require repeated treatments or combination therapies.
- Oxygen dependence: The need for oxygen means PDT may be less effective in poorly vascularized or necrotic tumors.
Procedure: What to Expect
A typical PDT session involves:
- Application or administration of a photosensitizer.
- Waiting period (from minutes to several hours) for drug accumulation and clearance from healthy tissues.
- Exposure of the target tissue to a specific light source (LEDs, lasers, or lamps) for a set duration.
- Post-procedure care, including protection from strong light sources.
Most procedures can be performed on an outpatient basis. Side effects are generally mild and temporary.
Recent Advances and Research Directions
Research in photodynamic therapy continues to expand the range of applications and effectiveness. Key areas of innovation include:
- Novel photosensitizers: Developing agents with greater tissue selectivity, rapid clearance from the body, and absorption at longer wavelengths for deeper penetration.
- Nano-delivery systems: Encapsulating photosensitizers in nanoparticles to improve targeting and reduce toxicity.
- Combination therapies: Integrating PDT with chemotherapy, immunotherapy, or radiation to enhance overall treatment outcomes.
- Imaging-guided PDT: Using real-time imaging to monitor drug distribution and treatment response.
- Antimicrobial PDT: Harnessing its potential to combat antibiotic-resistant infections in hospitals and clinics.
- Personalized medicine approaches: Tailoring photosensitizer and light protocols based on individual tumor characteristics or genetic profiles.
Nursing Care of Patients Undergoing Photodynamic Therapy
Providing optimal nursing care for patients undergoing photodynamic therapy requires a thorough understanding of the procedure, potential side effects, and the specialized precautions necessary to ensure patient safety and comfort.
Pre-Procedure Nursing Care
Nurses play a vital role in preparing patients physically and psychologically for PDT:
- Patient Assessment: Review the patient’s medical history, current medications, and allergies. Identify possible contraindications, such as porphyria or hypersensitivity to the photosensitizing agent.
- Patient Education: Explain the purpose of PDT, the steps involved, potential benefits, risks, and expected outcomes. Discuss the importance of photosensitivity precautions and adherence to post-treatment instructions.
- Informed Consent: Ensure that the patient (and family, if appropriate) understands the procedure and has signed informed consent.
- Skin Preparation: For dermatological applications, cleanse the treatment area as directed and remove any cosmetics or topical agents.
- Pre-Medication: Administer prescribed analgesics or anxiolytics if needed, as PDT can sometimes cause discomfort or pain during illumination.
- Psychological Support: Address patient concerns, answer questions, and provide reassurance to alleviate anxiety.
Intra-Procedure Nursing Care
During photodynamic therapy, nursing responsibilities focus on patient monitoring, safety, and comfort:
- Assisting with Administration: Assist the physician in the application or injection of the photosensitizing agent and ensure accurate timing for drug incubation.
- Monitoring for Adverse Reactions: Observe for signs of allergic reactions or local irritation following administration of the agent. Be prepared to manage any hypersensitivity or anaphylactic response.
- Protective Measures: Ensure both patient and staff wear appropriate protective clothing and eyewear, as the photosensitizer can make tissues highly reactive to light.
- Pain Management: Monitor for and address patient discomfort, particularly the stinging or burning sensation during illumination. Use cooling devices, fans, or prescribed analgesics as necessary.
- Vital Signs Monitoring: Record baseline and ongoing vital signs, especially in cases where systemic absorption of the drug is possible.
- Assisting with Light Exposure: Ensure the correct light source and wavelength are used, and that exposure time is carefully monitored to prevent tissue damage.
Post-Procedure Nursing Care
After photodynamic therapy, patients are at risk for photosensitivity reactions and require careful monitoring and education:
- Monitoring for Immediate Complications: Observe the patient for acute side effects such as swelling, erythema, blistering, or signs of infection at the treatment site.
- Pain and Symptom Management: Provide pain relief as needed, and instruct patients on managing post-procedural discomfort, which may include cool compresses or prescribed topical agents.
- Photosensitivity Precautions: Instruct the patient to avoid exposure to direct and indirect sunlight, as well as bright indoor lights, for a specified period following treatment—typically 24 to 72 hours, but sometimes up to several weeks depending on the photosensitizer used. Advise wearing protective clothing, wide-brimmed hats, sunglasses, and using blackout curtains as needed.
- Wound Care: Educate the patient on caring for the treated area. Advise keeping the site clean and dry, avoiding trauma or friction, and watching for signs of infection.
- Patient Education: Supply written instructions on post-treatment care, warning signs of complications, and when to seek medical attention (e.g., severe pain, fever, spreading redness).
- Follow-Up Care: Arrange for follow-up appointments to monitor healing, assess treatment response, and address any concerns or complications.
- Emotional Support: Recognize that patients may experience anxiety or distress due to appearance changes, discomfort, or cancer diagnosis. Provide support and referrals to counseling or support groups as needed.
Management of Side Effects and Complications
While PDT is generally well-tolerated, certain adverse effects may occur:
- Local Skin Reactions: Erythema, edema, blistering, peeling, or crusting. Care includes gentle cleansing, application of soothing agents, and infection prevention.
- Photosensitivity Reactions: Severe burning or blistering upon light exposure. Ensure strict adherence to light avoidance and protective measures.
- Infection: Though rare, infection may develop at the treatment site. Teach patients to recognize early signs and report them promptly.
- Systemic Reactions: Headache, nausea, or general malaise may rarely occur. Monitor and report as appropriate.
- Emotional Responses: Fear, anxiety, and self-image concerns may result from visible skin changes. Provide psychological support and resources.
Patient and Family Education
Education is a cornerstone of successful outcomes in PDT:
- Understanding the Process: Use simple language and visual aids to explain the rationale, process, and expected outcomes of PDT.
- Photosensitivity Precautions: Reinforce the critical importance of avoiding all bright light sources post-treatment, including flashlights, fluorescent lighting, and screens, until cleared by the physician.
- Skincare Instructions: Instruct on gentle cleansing, avoidance of irritants (perfumes, scrubs), and use of moisturizer as recommended.
- Recognizing Complications: Provide a checklist of warning signs that should prompt immediate contact with healthcare providers.
- Emotional Support: Encourage open dialogue about concerns and provide access to patient support groups or counseling as necessary.
Documentation and Interdisciplinary Collaboration
Thorough documentation is vital:
- Record the photosensitizing agent used, dosage, route, timing of administration, and duration of light exposure
- Document pre- and post-procedure assessments, patient education provided, and any complications or interventions
- Communicate with the interdisciplinary team—including physicians, dermatologists, oncologists, and pharmacists—to coordinate care and ensure continuity
REFERENCES
- Jia J, et al. Revolutionizing cancer treatment: Nanotechnology-enabled photodynamic therapy and immunotherapy with advanced photosensitizers. Frontiers in Immunology. 2023; doi:10.3389/fimmu.2023.1219785.
- Al Aboud AM, Randall Dan. Photodynamic Therapy (PDT) for Skin Conditions. Clinical Overview. ClinicalKey. DynaMed, LLC.
- Alvarez N, Sevilla A. Current Advances in Photodynamic Therapy (PDT) and the Future Potential of PDT-Combinatorial Cancer Therapies. https://pmc.ncbi.nlm.nih.gov/articles/PMC10815790/. Int J Mol Sci. 2024;25(2):1023.
- Domka W, et al. Photodynamic therapy for eye, ear, laryngeal area, and nasal and oral cavity diseases: A review. Cancers. 2024; doi:10.3390/cancers16030645.
- American Osteopathic College of Dermatology. Photodynamic Therapy. https://www.aocd.org/page/PhotodynamicTherapy.
- Correia JH, Rodrigues JA, Pimenta S, Dong T, Yang Z. Photodynamic Therapy Review: Principles, Photosensitizers, Applications, and Future Directions. Pharmaceutics. 2021 Aug 25;13(9):1332. doi: 10.3390/pharmaceutics13091332. PMID: 34575408; PMCID: PMC8470722.
- Liu H and Kalia S. Photodynamic Therapy. In: Bolognia JL, Schaffer JV and Cerroni L, eds. Dermatology. 5th ed. Philadelphia, PA: Elsevier. 2025. 2379-2389.
- Ou-Yang Y, Zheng Y, Mills KE. Photodynamic therapy for skin carcinomas: A systematic review and meta-analysis. https://pmc.ncbi.nlm.nih.gov/articles/PMC9892842/. Front Med (Lausanne). 2023;10:1089361.
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





